Morel-Lavalle lesion
Images

CASE SUMMARY
A 56-year-old police officer was involved in an altercation in August 1995 during which he sustained multiple stab wounds.
Initial evaluation by Physical Medicine and Rehabilitation (PM&R) in February 2010 was for chronic left hip pain worsening over the past five months. He reported 4 to 5 year history of localized “band-like pain” around the left hip with a second sharp inguinal pain. The pain was characterized as deep, achy, throbbing and constant; better in the morning and progressively worse later in the day; alleviated with Vicodin, ASA, NSAID; and aggravated by activity and prolonged sitting. Objective examination noted for mild tenderness at the mid-line thigh/inguinal junction and decreased sensation in the left thigh consistent with meralgia paraesthetica.
Patient underwent a protracted course of treatment with multiple evaluations by various specialties, including PM&R, interventional pain, orthopedics, rheumatology and interventional radiology. An interventional pain specialist performed multiple ultrasound-guided fluid aspirations (Figure 1) over a two-year period. Fluid was initially noted to be translucent yellow in color and progressed over the course of aspirations to serosanguinous in nature. Repeated fluid analysis noted no growth. Patient subsequently underwent surgical excision. Pathology confirmed suspected diagnosis. Patient initially experienced excellent pain relief sustained for two months. However, follow-up established insidious return of previous symptoms.
IMAGING FINDINGS
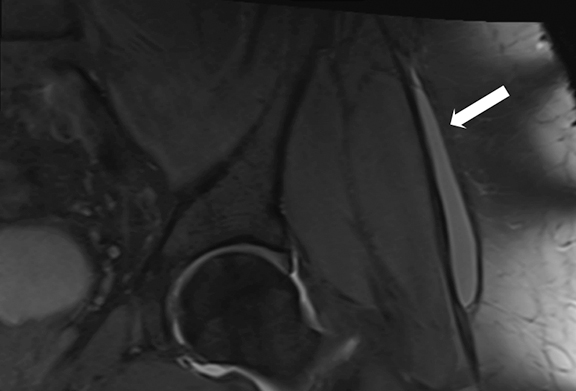
Diagnostic studies included MRI, which revealed a fluid collection consistent with ganglion cyst under the left tensor fascia lata.
Subsequently, the imaging was re-reviewed with musculoskeletal radiology and the MRI picture was most consistent with Morel-Lavalle lesion (Figure 2).
DIAGNOSIS
Morel-Lavalle lesion. Differential diagnosis includes ganglion cyst, fat necrosis, sarcoma, hemangioma, subcutaneous hematoma, aneurysmal bone cyst.1
DISCUSSION
This report outlines a case study of a unique presentation of a Morel-Lavalle injury. We describe the case of a patient who presented with recurrent thigh pain after multiple stab wounds. The patient was seen by several specialists, tried various medications, and underwent repeated aspirations and injections.
Morel-Lavalle lesions are closed internal degloving injuries that are uncommon. They can occur in the pelvis or proximal thigh and are usually due to trauma, involving a force of combined compression and shear causing separation of the subcutaneous fat from the underlying fascia.2-3
CONCLUSION
Morel-Lavalle lesions are often underdiagnosed because they are rare.2,3 Clinical diagnosis may present as a soft, fluctuant mass in an area that has a history of injury. Lesions may or may not be associated with contusions, abrasions and/or decreased sensation. Because Morel-Lavalle lesions are not well known and there can be variable presentation, subsequent diagnosis and appropriate treatment of these lesions can be difficult.4 Several potential therapeutic options include non-operative compression, aspiration, surgical percutaneous drainage or surgical excision.
Further diagnostic evaluation of fluid accumulation improves identifying the etiology and directing appropriate treatment.
REFERENCES
- Gilbert BC, Bui-mansfield LT, Dejong S. MRI of a Morel-Lavellée lesion. AJR Roentgenol. 2004;182 (5):1347-1348.
- Powers ML, Halem SF, Sundaram M. Diagnosis: Morel-Lavalee lesion. Orthopedics. 2007;30:322-323.
- Phillips T, Jeffcote B, Collopy D. Bilateral Morel-Lavallee lesions after complex pelvic trauma: a case report. J Trauma. 2008;65:708-711.
- Zhong B, Zhang C, Luo C. Percutaneous drainage of Morel-Lavallee lesions when the diagnosis is delayed. Canadian Journal of Surgery. 2014;57(5):356-357.
Citation
RS O, S P.Morel-Lavalle lesion. Appl Radiol. 2017; (2):38-39.
February 8, 2017