Measuring subcutaneous fat patterning with precision: An ultrasound technique for every body
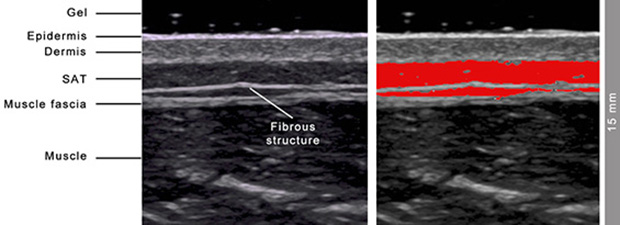
Typical example of an ultrasound image of SAT. Image by Wolfram Müller, Medical University of Graz. Used with permission.
Accurately measuring subcutaneous adipose tissue (SAT) is important when assessing body composition, particularly with respect to treating obese and anorexic patients and evaluating the health of athletes. An ultrasound technique developed at the University of Graz in Austria for precisely measuring SAT and embedded fibrous structures in lean and normal-weight individuals has now been validated for use with the overweight and obese. The method, described in Ultrasound in Medicine and Biology and in the British Journal of Sports Medicine, can be used to assess response to weight intervention treatments, including comparison of fat profiles of patients pre- and postbariatric surgery.
The ultrasound imaging and tissue-thickness-evaluation technique maximizes both accuracy and reproducibility and ensures multiple thickness measurements with an accuracy of approximately 0.2 mm. at eight specific sites. Site locations include the upper and lower abdomen, erector spinae, distal triceps, brachioradialis, front and lateral thigh, and medial calf. All sites overlie muscle with a clear visible fascia. This simplifies the acquisition of clear images, typically within a 20-minute period for the entire process.
Principal investigator Wolfram Müller, MD, Professor for Biophysics, and colleagues explain that standardizing the marking and measuring procedure is important to obtain precise and reproducible results because precision is influenced by the viscoelastic movements of SAT depending on the actual body position. Orienting and positioning the ultrasound probe at the center of each site is necessary to avoid mapping another region of SAT because of SAT’s furrowed borders. For this reason, using measurement sites where the SAT thickness does not change much in the region surrounding the center of the site is essential.
After marking, the ultrasound scan is performed on the right side of the body while an individual is lying in a supine, prone, and/or rotated position. To avoid SAT compression and fat compression errors, a 3-5 mm layer of gel is applied to the skin. An 18-MHz probe is used with conventional ultrasound systems for thin persons and lower frequencies for persons with thicker SAT layers. A sound speed of 1450 m/s is used in the evaluation software to avoid a sound speed error of about 6%. Low frequencies of 4 to 6 MHz also are necessary to penetrate the thick layers of SAT in overweight and obese patients. While low frequencies are associated with lower tissue border resolution, the relative error remains small.
The authors advise orienting the ultrasound probe longitudinally to the muscle. The gel between the probe and the skin appears as an upper black layer. The SAT layer is imaged as a dark band between the lower contour of the skin and the upper contour of the fascia of the muscle that is situated below the SAT. FAT software (US Tissue-FAT 3.3, Rotosport, Stattegg, Austria), specifically designed for multiple semi-automatic evaluations of SAT layer thicknesses, is used to interactively evaluate acquired ultrasound images.
A total of 38 individuals with body mass index (BMI) values between 18.6 and 40.3 kgm-2 participated in the study. A standard error of estimate equated to 1.1 mm and 95% of measurements were within 2.2 mm in this group that included overweight and obese persons.
“This ultrasound method allows detection of fat profile changes on a finer scale than any other method. It enables longitudinal studies of fat patterning changes with a sensitivity not reached by any other technique. The method can also be applied to optimize the image segmentation algorithms of other imaging techniques like MRI or CT,” the authors wrote.
Dr. Müller, said, “This measurement method is very useful for controlling any fat reduction intervention. It is also of high relevance to get accurate values of the fat layer thicknesses and the fat patterning in underweight or anorectic persons and in all weight sensitive sports where low weight problems and eating disorders are currently among the major challenges of sports medicine. Any weight intervention can be quantified accurately in terms of fat amount changes. This enables distinguishing between fat and muscle mass changes, which cannot be based on weight measurement alone.”
REFERENCES
- Müller W, Lohman TG, Stewart AD, et al. Subcutaneous fat patterning in athletes: selection of appropriate sites and standardisation of a novel ultrasound measurement technique: ad hoc working group on body composition, health and performance, under the auspices of the IOC Medical Commission. Br J Sports Med. 2016 50: 45-54.
- Störchle P, Müller W, Sengeis M, et al. Standardized Ultrasound Measurement of Subcutaneous fat patterning: High Reliability and Accuracy in gGroups Ranging from Lean to Obese. Ultrasound Med Biol. 2017 43;2: 427-438.