Leiomyosarcoma of the Inferior Vena Cava
Images
Case Summary
An adult with a history of metastatic prostate cancer presented for routine surveillance CT.
Imaging Findings
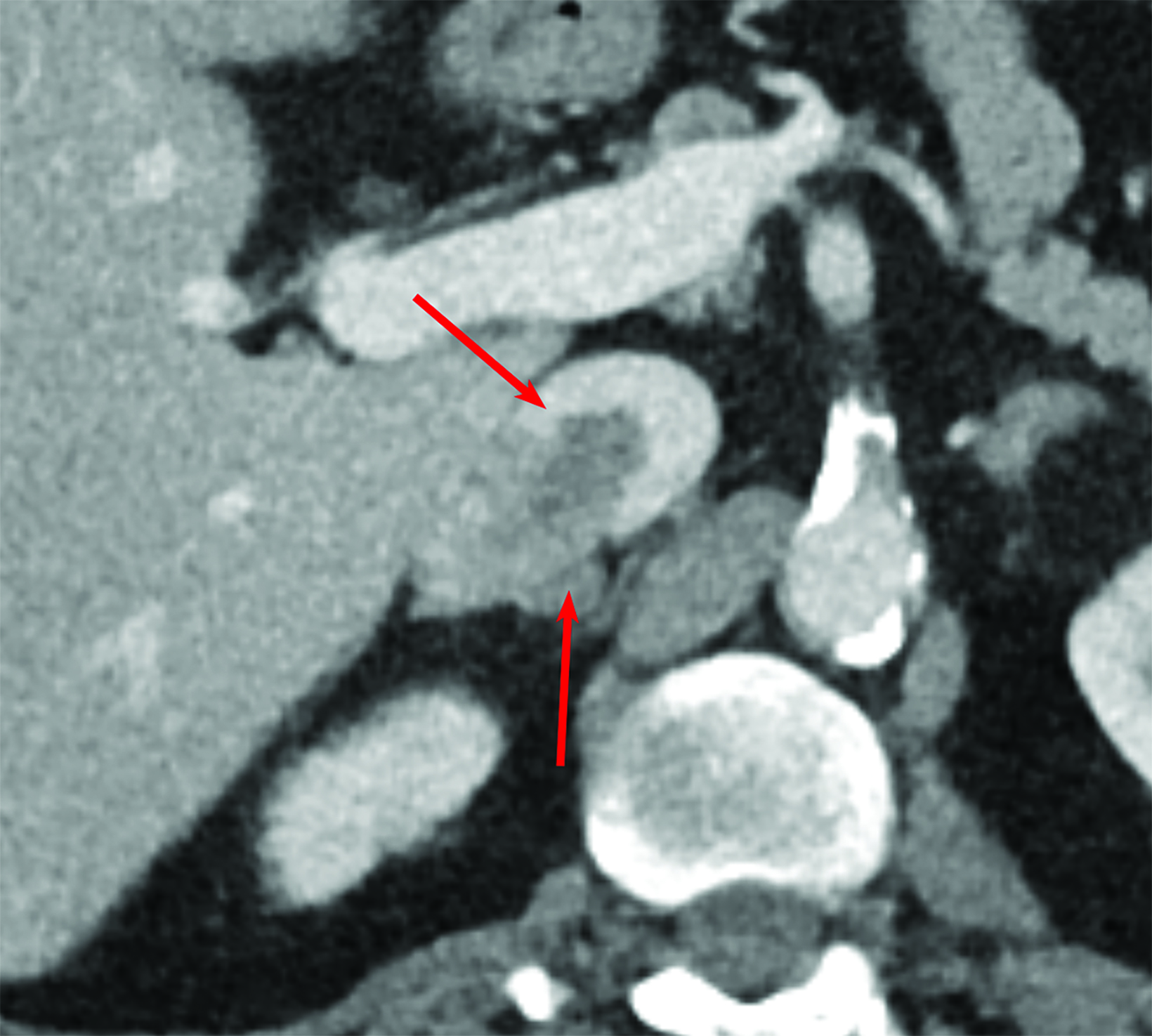
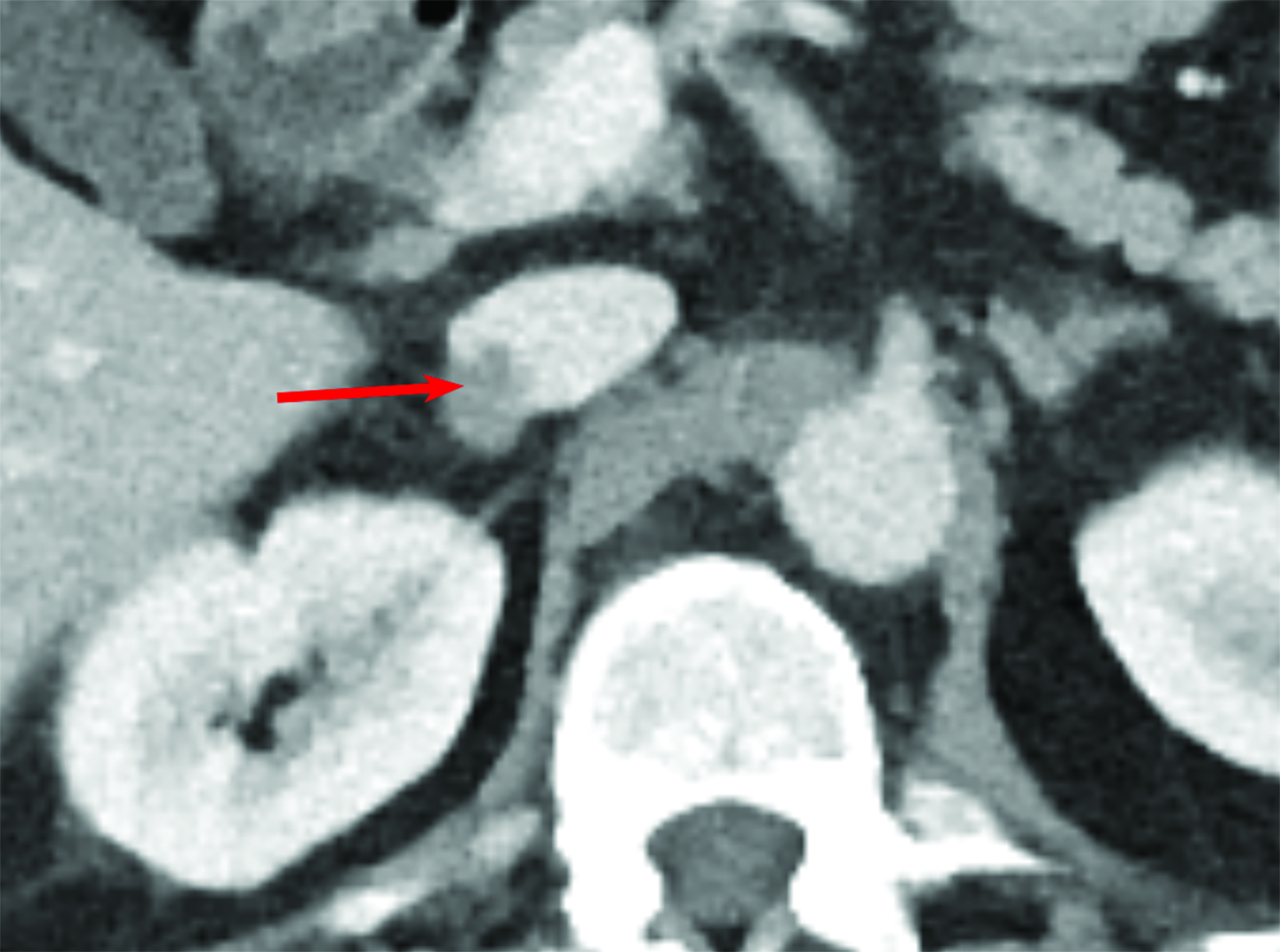
Contrast-enhanced CT of the chest, abdomen, and pelvis showed no evidence of metastatic bone disease or pelvic lymphadenopathy. A low-density filling defect was observed within the inferior vena cava (IVC) contrast column (Figure 1). Low-density tissue extended beyond the lumen of the IVC into the adjacent right adrenal gland, forming a 2.7 × 2.4 × 2.4 cm nodule. Initial prostate cancer staging CT seven years prior showed the tumor to be centered along the IVC with 50% being intraluminal and 50% extraluminal (Figure 1). The patient underwent adrenalectomy and resection of the involved portion of the IVC.
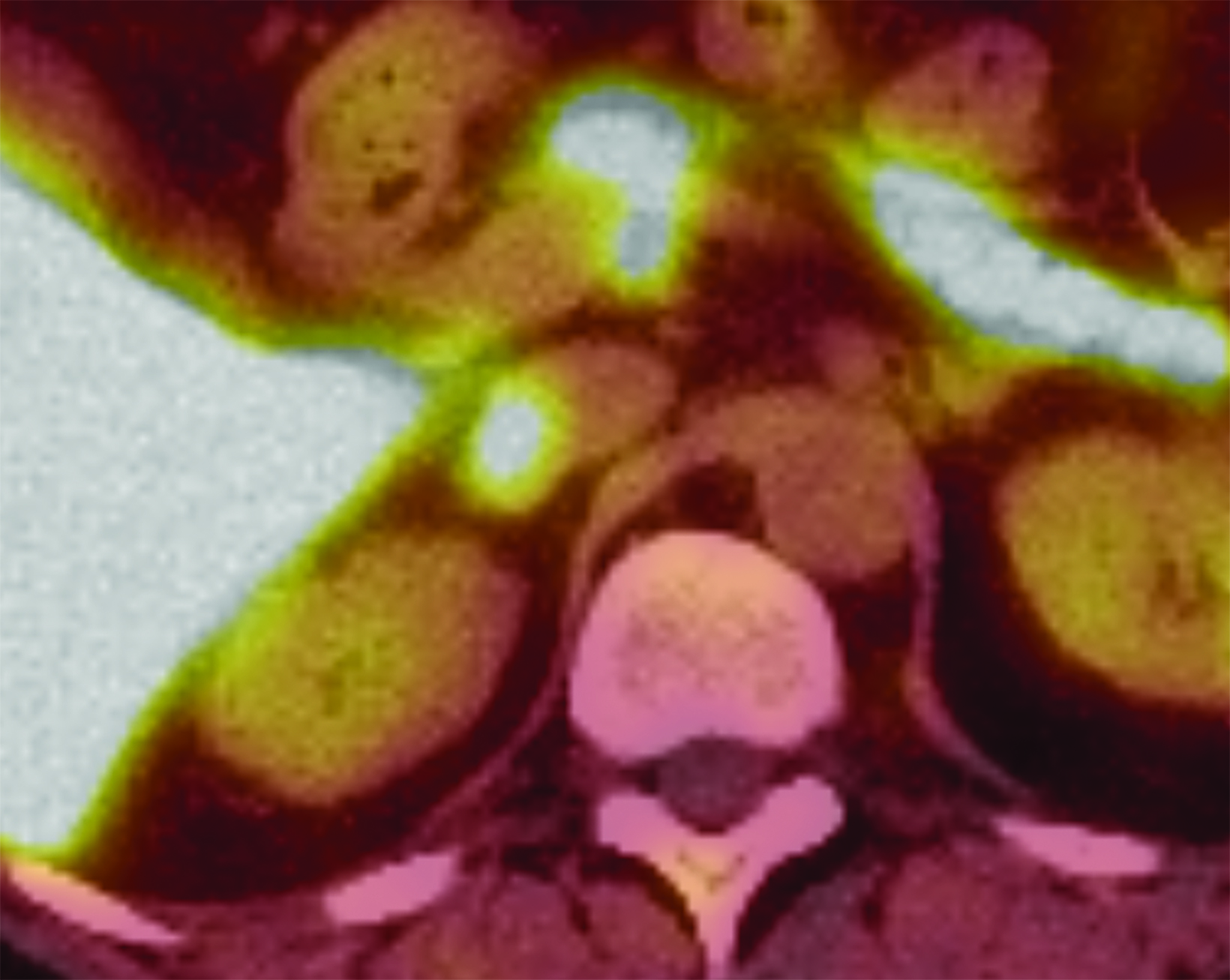
Retrospective evaluation of multiple studies showed growth of the intra- and extraluminal components, with greater growth extraluminally into the adrenal gland with varying degrees of intraluminal conspicuity related to contrast bolus timing. The lesion also demonstrated significant F-18 fluciclovine uptake adjacent to physiologic liver activity (Figure 2).
Diagnosis
Leiomyosarcoma of the IVC.
Differential diagnosis includes metastasis and adrenal origin neoplasms such as low-grade adrenal malignancies, including pheo-chromocytoma, low-grade adrenal carcinoma, and primary adrenal lymphoma.
Discussion
Venous leiomyosarcomas predominantly involve the IVC and represent fewer than 1% of malignant tumors.1 Roughly 300 have been reported since 2006.2 This tumor affects women more than men, with a ratio of 3:1, and occurring most frequently between the ages of 40 and 60 years.3
The appearance of an IVC leiomyosarcoma on imaging can be somewhat variable. Most commonly, these tumors grow extraluminally at a rate of 2:1 versus intraluminal growth.3 They typically appear as heterogeneously enhancing masses with at least some intraluminal component causing a filling defect.
Filling defects on routine contrast-enhanced CT present a frequent dilemma for the radiologist. The most common reason for poor contrast opacification of a vein or portion of a vein is admixture of blood containing contrast with blood not yet saturated with contrast. These wispy or streaking filling defects are readily recognized by the radiologist and determined to be normal. Occasionally, these filling defects demonstrate a more distinct border, which can indicate thrombus, neoplasm, or often simply an atypical appearance of admixture.
Intravenous neoplasms are commonly associated with solid organ tumors which extend into the venous drainage of the organ. The benign primary tumor of the venous smooth muscle layer, leiomyoma, and its malignant counterpart, leiomyosarcoma, are rarer causes for venous filling defects. These tumors may develop cystic necrosis. Leiomyosarcoma uptake of F-18 fluciclovine has not previously been reported.
The level of the IVC involved is important for prognosis and treatment planning. Renal and suprarenal levels are most common (42%-50%) and have the most favorable prognosis. Intrahepatic is the rarest level of involvement (6%-20%) and has the worst prognosis. Approximately 37%-44% of leiomyosarcomas of the IVC are infrarenal. Although indolent, significant mortality is associated with these tumors, with an overall 10-year survival of 14% after complete resection.4
Conclusion
Inconsistent contrast opacification on CT makes the IVC prone to artifact from admixture. Inclusion of the IVC into the radiologist search pattern is essential for identifying true pathology, including the rare leiomyosarcoma, as well as relatively common pathologies such as bland and tumor thrombus.
References
Citation
CD T, K S.Leiomyosarcoma of the Inferior Vena Cava. Appl Radiol. 2024; (3):42-43.
May 7, 2024