Indolent synovial sarcoma in adolescent male: MR, PET, microscopy, and arthroscopy correlation
Images

CASE SUMMARY
A 16-year-old Native American male presented with 2 years of gradually worsening left knee pain initially treated with anti-inflammatory medication and physical therapy. Magnetic resonance imaging revealed the presence of an anterior lesion within Hoffa’s fat pad. After referral to orthopedic surgery, he underwent arthroscopy with subtotal synovectomy/excision.
IMAGING FINDINGS
Sagittal T1-, T2- and proton density (PD)-weighted MR images of the left knee (Figure 1, A-C) demonstrates the 2.3 cm soft tissue mass (arrowheads) within the infrapatellar space displacing Hoffa’s fat pad which shows predominantly T1 hypointensity, and T2/PD heterogeneity with areas of iso, hypo, and hyperintense signal (to muscle). Coronal PD image (Figure 1D) confirms location predominantly within the medial compartment of the left knee with questionable early involvement of the medial femoral condyle (arrow).
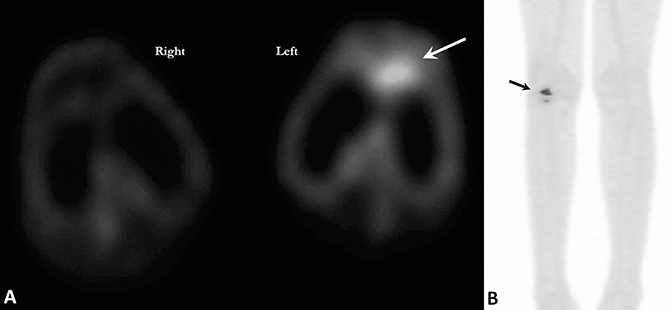
PET/CT images (Figure 2 A-B) performed two months following surgical excision reveal residual focal hypermetabolism in the intraarticular space at the anterior aspect of the left knee joint along the intercondylar notch of the distal left femur. These findings could be seen with either residual tumor or post-operatively. Posterior view PET maximum intensity image (B) shows focal uptake of the left knee with maximum SUV of 2.1. No other foci of hypermetabolism were seen.
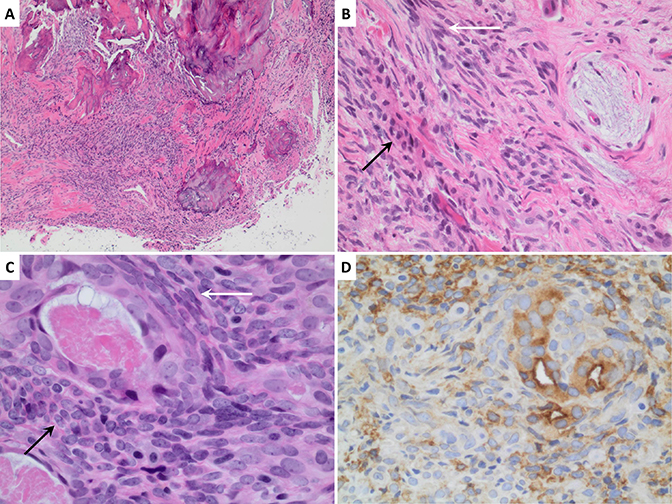
Histopathology images (Figure 3) with low (A), medium (B), and high (C) power H&E staining with characteristic biphasic squamous cell and spindle cell patterns. Epithelial membrane antigen immunoperoxidase stain (D) highlights the epithelial component. By RT-PCR this tumor is positive for an SYT-SSX1 fusion transcript.
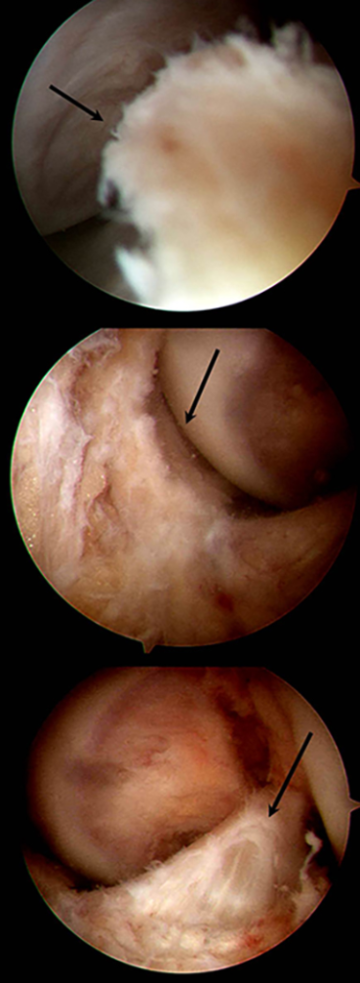
Arthroscopy images (Figure 4) of the left knee reveal the lobulated mass within the anterior fat pad, having the gross appearance of pigmented villonodular synovitis, according to the operative report.
DIAGNOSIS
Biphasic grade 2 synovial sarcoma. Differential diagnosis includes: neoplasm (undifferentiated pleomorphic sarcoma, peripheral nerve sheath tumor), pigmented villonodular synovitis, Hoffa's syndrome, or meniscal cyst.
DISCUSSION
Sarcomas are rare mesenchymal tumors that account for 1% of all malignancies.1,2 Synovial sarcoma (SS) is a sarcoma subtype consisting of spindle-cell tumors with variable epithelial differentiation that is often associated with SYT-SSX gene fusion.1-5 SS comprises 2.5%–10.5% of all primary soft-tissue malignancies worldwide2 and occurs in both the pediatric and adult populations, remaining the commonest non-rhabdomyosarcoma soft tissue sarcoma (NRSTS) in childhood.3-5Approximately 30% of patients are younger than 20 years of age.4
SS most frequently affects the musculoskeletal system with the extremities involved in over 85% of cases. The lower extremities (~70%) especially the knee and peri-popliteal fossa, tendon sheaths, and bursae are effected in younger adults (≤40 years of age).1-3,6 Contrary to the implied nomenclature, these neoplasms do not arise intra-articularly or within the synovium, rather these mesenchymal cells differentiate just enough so as to resemble synovial spindle cells. An increasing number of reports are describing extra-extremity primary SS.2,6 The lung is the most common site for metastasis, and post-metastatic survival is rare.4 As an intermediate to high-grade tumor, the risk of local recurrence and distant metastasis is consequential, despite initial aggressive surgical resection.2 Optimal treatment remains elusive in the absence of randomized clinical trials, owing to its rarity.3 Recurrent SS is considered chemosensitive and typically treated with rhabdomyosarcoma protocols by pediatric oncologists.3,4
Patients typically present with slow-growing palpable masses (frequently ≥ 5cm). The paradoxically insidious onset often delays the diagnosis up to several years, prolonging the time from initial symptoms to treatment and worsening the stage.
While radiographic features are infrequently diagnostic, common findings include a juxtaarticular soft tissue mass with peripheral calcifications.7-9 CT findings show a well-circumscribed muscle-density mass with heterogeneous enhancement and peripheral punctate calcification. MRI is most useful demonstrating multi-lobulation and marked heterogeneity with the “triple sign” (areas of hypo, iso, and hyperintensity on T2) seen in upwards of 35% of patients.7-9 Additional studies report a “bowl of grapes” sign with multiple internal septations and cystic necrosis.8 PET imaging is particularly helpful for initial staging, post-treatment management with the literature reporting at least 80% F18-FDG sensitivity, and for prognostication utilizing SUVmax.10
CONCLUSION
Synovial sarcomas are rare mesenchymal tumors representing the most common non-rhabdomyosarcoma soft tissue sarcoma of childhood, especially of the lower extremity and knee. These can masquerade as pigmented vilonodular synovitis having a similar appearance on arthroscopy and MR imaging. Common MR findings include a hypointense homogenous appearance on T1 with a heterogenous multilobulated appearance on T2 and varying degrees of internal septations (triple sign, bowl of grapes sign). The insidious onset and propensity for recurrence/metastasis warrants heightened diagnostic suspicion. Histopathology remains a crucial diagnostic component.
REFERENCES
- Baheti AD, Sewatkar R, Hornick JL et al. Imaging features of primary and recurrent intrathoracic synovial sarcoma: a single-institute experience. Clinical Imaging. 2015; 39: 803–808.
- Bakri A, Shinagare A, Krajewski K et al. Synovial sarcoma: Imaging features of common and uncommon primary sites, metastatic patterns, and treatment response. AJR. 2012; 199: W208-W215.
- Ferrari A, De Salvo G, Brennan B, et al. Synovial sarcoma in children and adolescents: the European Pediatric Soft Tissue Sarcoma Study Group prospective trial (EpSSG NRSTS 2005). Ann Oncol. 2015 Mar; 26(3):567-72.
- Andrassy R, Okcu M, Despa S, Raney R. Synovial sarcoma in children: surgical lessons from a single institution and review of the literature. J Am Coll Surg. 2001 Mar; 192(3):305-13.
- Schmidt D, Thum P, Harms D, Treuner J. Synovial sarcoma in children and adolescents. A report from the Kiel Pediatric Tumor Registry. Cancer. 1991; 67(6):1667-72.
- Hernandez RA, Lino-Silva LS, Luna-Ortiz K. Synovial sarcomas of the head and neck: Comparative analysis with synovial sarcoma of the extremities. Auris Nasus Larynx. 2013; 40: 476–480.
- McCarville M, Spunt S, Skapek S, Pappo A. Synovial sarcoma in pediatric patients. AJR Am J Roentgenol. 2002 Sep; 179(3):797-801.
- Liang C, Mao H, Tan J, et al. Synovial sarcoma: Magnetic resonance and computed tomography imaging features and differential diagnostic considerations. Oncology Letters. 2015; 9: 661-666.
- Murphey MD, Gibson MS, Jennings BT et al. Imaging of synovial sarcoma with radiologic-pathologic correlation. RadioGraphics. 2006; 26:1543–1565.
- Charest M, Hickeson M, Lisbona R et al. FDG PET/CT imaging in primary osseous and soft tissue sarcomas: a retrospective review of 212 cases. Eur J Nucl Med Mol Imaging. 2009; 36(12): 1944-1951.