Imaging benign soft tissue lesions of the foot
Images










Dr. Moholkar and Dr. Sawhney are Specialist Registrars, and Dr. Bhatt is a Consultant Radiologist, Department of Radiology, University Hospitals of Leicester NHS Trust, Leicester, UK.
This review considers imaging features of palpable lesions around the foot that are generally benign.1–3 The foot is a relatively uncommon site of tumors. It contains a large number of tissue types including tendons, plantar fascia, retinaculae and synovium,1 which correspond to the distribution of masses in this region. Vascular tumors also represent common soft-tissue masses of the foot. Ultrasound (US) can be used to confirm the presence of a suspected lesion and is an important adjunct to diagnosis. Magnetic resonance imaging (MRI) is the modality of choice to define the depth and extent of a lesion, the tumor margins and to characterize lesions accurately.
Vascular lesions
Hemangioma
Hemangiomas are the most frequent benign foot tumors of vascular origin.1,3 They can be divided into capillary, cavernous, venous orarteriovenous.4 They can be superficial in the subcutaneous tissue or deep-seated in the muscle.2 Phleboliths can be detected on plain radiographs in the majority of hemangiomas. On T1-weighted (T1W) images the vascular component of hemangiomas demonstrates a low-to-intermediate signal intensity, which can be altered by the presence of non-vascular soft-tissue elements such as fat, smooth muscle, fibroustissue, hemosiderin or thrombus.2
T2-weighted (T2W) MR images show multilobulated and septated lesions of high signal intensity, thought to reflect slow blood flow in cavernous hemangiomas.2 Phleboliths are seen as nodular areas of low signal intensity on all pulse sequences.2 Contrast-enhanced images usually show marked enhancement of the vascular components of the lesions.1
AV malformations
Arteriovenous malformations have abnormal communication between the arteries and veins.4 They are usually congenital, but may also be posttraumatic.5
These can be superficial lesions without arteriovenous shunting or deep lesions with arteriovenous shunting.4 The deep lesions are usually symptomatic. Arteriovenous hemangiomas occur in young patients and children.5 High-flow lesions may cause local changes like limb enlargement and skin warmth with a bruit over the lesion.
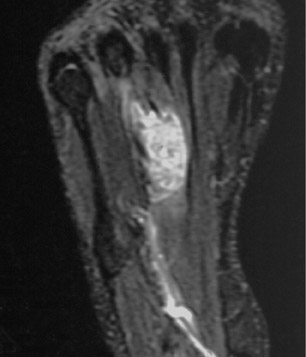
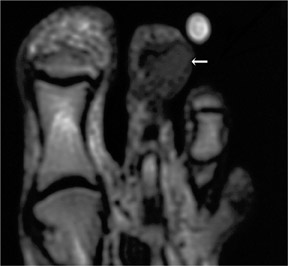
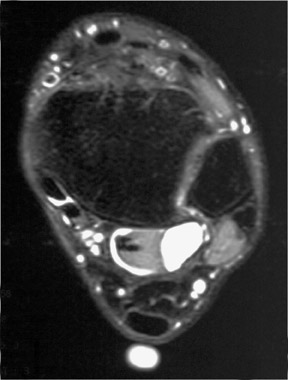
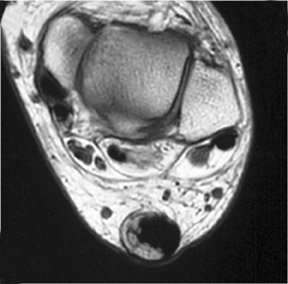
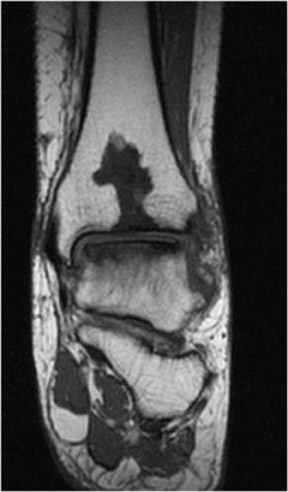
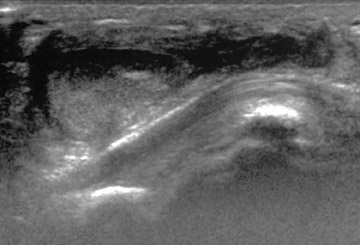
On MRI, arteriovenous malformations are composed of large tortuous often serpiginous arterial and venous vessels with multiple areas of signal void due to the rapid blood flow (Figure 1). MRI is a noninvasive method to demonstrate the soft tissue, bony extent and size of the lesion, thus being an important adjunct to management.5
Lymphangioma
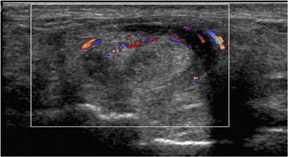
Lymphangiomas are relatively rare, predominantly seen in children <2 years, accounting for 6% of benign childhood tumors.6 They are thought to be congenital in origin, secondary to abnormal embryogenesis.4,6 Patients present with a soft, fluctuant mass, which may show rapid enlargement due to bleeding or infection. Lymphangiomas are infiltrative in nature and spread across tissues. Ultrasound shows a multiseptate cystic lesion with posterior enhancement, with or without a fluid level. It may also help in differentiating a lymphangioma from a hemangioma, as there is no significant Doppler flow in a lymphangioma.6
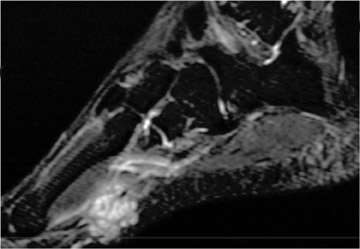
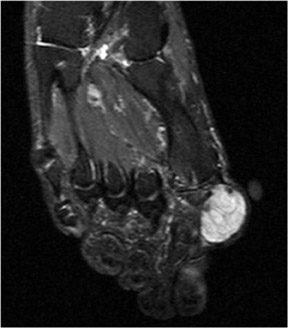
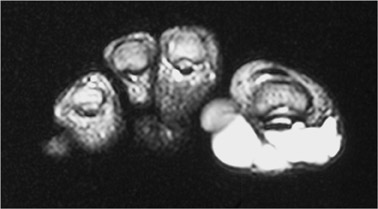
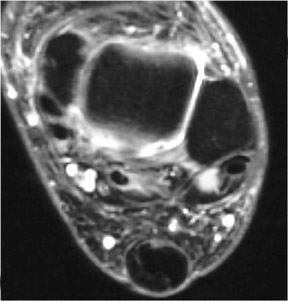
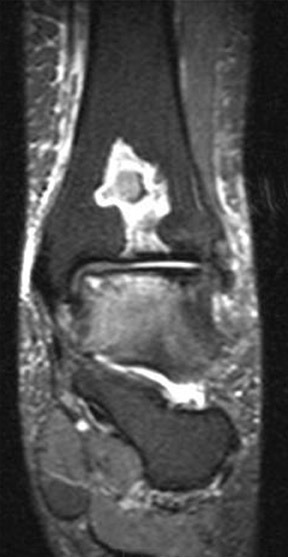
MRI shows a fluid-filled mass with low-to-intermediate signal on T1W images and high signal intensity on T2W images (Figure2).6
Lymphangiomas demonstrate absence of feeding vessels and lack of intense contrast enhancement on MRI. After IV contrast administration, the lack of intense intralesional contrast enhancement is consistent with a lymphangioma.6
Lipoma
Lipomas are the most common of all soft-tissue tumors, in patients who are 30 to 50 years of age with a predilection for the subcutaneous tissues of the trunk and extremities.1 Subcutaneous lipomas are usually encapsulated and show a lobular architecture. Conventional radiographs show a well-defined radiolucent mass that may have areas of calcification.
Lipomas are typically isointense to fat on both, T1W and T2W images; however signal alterations may be caused by infarction,inflammation, areas of hemorrhage or calcification, making the differentiation from liposarcoma difficult.1,2 In these cases, lesions contain regions of isointense fat as well as areas with decreased signal intensity on T1W images and heterogeneous signal intensity on T2Wimages.1,7
Pigmented villonodular synovitis and giant-cell tumor of the tendon sheath
Pigmented villonodular synovitis (PVNS) represents an inflammatory proliferative intra-articular disorder of the synovium.1,2 PVNS occurs as a focal or diffuse synovial mass, most frequently involving large joints. The knee is the most common site followed by the hip,shoulder and ankle.3 Plain radiographic features include joint effusion, bone erosion and cysts, with relative preservation of the joint space. Calcifications within the lesion are very rare and, if present, differential diagnoses of synovial chondromatosis and synovial sarcoma should be considered.
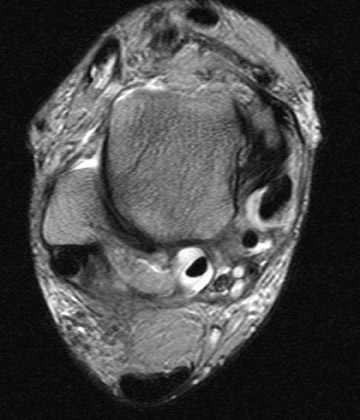
Giant-cell tumor (GCT) of the tendon sheath is the extra-articular counterpart of PVNS, arising from tendon sheaths, bursae or ligaments.1,2 Giant-cell tumors are among the most common soft-tissue tumors of the foot, they occur in young adults, and have a predilection for the digits.2 Pathologically, GCT of the tendon sheath is a highly vascular mass with an admixture of multinucleated giant cells, hemosiderin deposits, macrophages, fibroblasts and xanthoma cells: the same histologic features as PVNS.1 Plain radiography shows a diffuseor localized soft-tissue mass with underlying bone erosions.
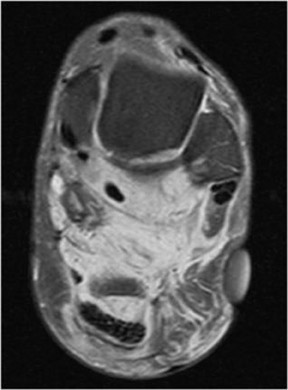
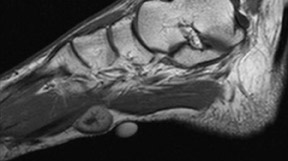
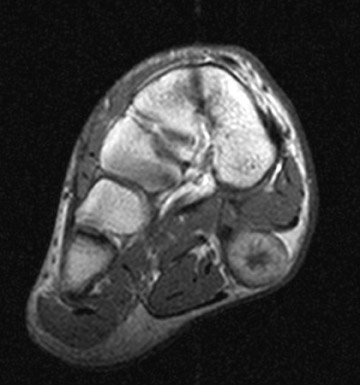
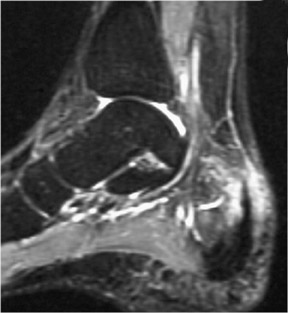
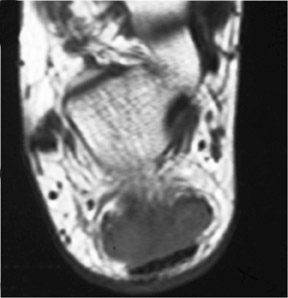
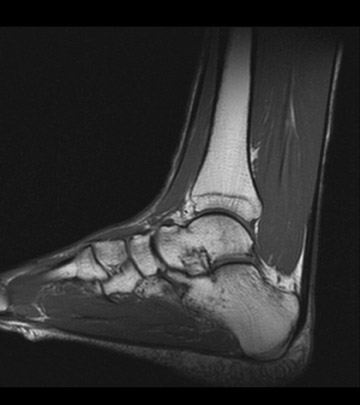
The MRI features of GCT and PVNS are similar and reflect their variable tissue composition.8 T1WMR shows lesions to be isointense to hypointense to muscle and hypointense on T2W images.9 Both lesions demonstrate characteristic low signal on T1W and T2W images due to the paramagnetic effect of hemosiderin (Figure 3).8 Heterogeneous signal intensity may occur depending on the histological composition. Strong, homogeneous enhancement is due to the extensive capillary network in the collagenous stroma.9 The decreased signal intensity on both T1W and T2W images is an uncommon appearance of extra-articular soft-tissue masses, in particular when they occur in the hands or feet, and this may suggest the diagnosis of giant-cell tumor of the tendon sheath.8
Neurogenic tumors
These include schwannoma, neurofibroma and rarely occur in the foot. They usually present as painless lumps or have neurogenic symptoms if a large nerve is involved.
Schwannoma
Schwannomas are well-circumscribed benign tumors arising from Schwann cells of the nerve sheath. They are commonly seen in adults from 20 to 50 years of age.10 As they grow, they displace nerve fibers eccentrically. T1W MRI shows a well-demarcated lesion with an intermediate signal intensity and low–signal-intensity margin. T2W images demonstrate high signal intensity.2
Neurofibroma
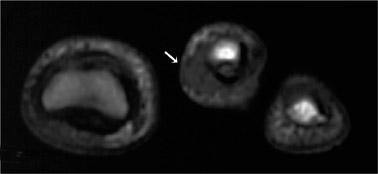
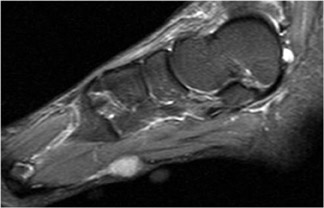
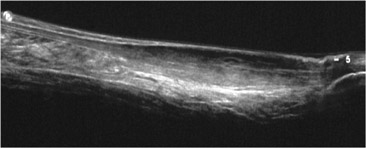
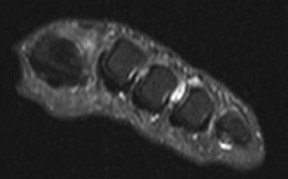
Neurofibromas are nonencapsulated, infiltrative lesions, which separate the nerve fibers causing fusiform enlargement of the nerve. Histologically they are composed of Schwann cells, nerve fibers, fibroblasts and collagen. T1W MR demonstrates a homogeneous lesion, which is isointense to skeletal muscle. The central area of the tumor is composed of nerve fiber bundles or dense collagenous and fibroustissue, which appears as low signal intensity on T2W images resulting in a characteristic “target” appearance.10 On postcontrast images,there is enhancement of the peripheral component, again demonstrating the “target” appearance and a “tail sign” may be seen, showing the origin of the tumor from the peripheral nerve (Figure 4).
Having 2 or more neurofibromas, or plexiform neurofibroma arising from a major nerve and its branches, is one of the diagnostic criteriafor neurofibromatosis type 1. Plexiform neurofibromas are pathognomonic of neurofibromatosis type 1 and often extend into adjacent muscles, fat and subcutaneous tissue.
Ganglion cyst
A ganglion represents a unilocular or multilocular cystic lesion containing mucinous fluid and surrounded by a fibrous capsule. They may communicate with fibrous tendon sheaths or joint capsules, but may be completely separate from them. They present as round, oval, lobulated or septated masses. They occur most frequently in the hand and wrist followed by the dorsum of the foot. Clinical presentation is usually as swelling or pain, which may be related to trauma.
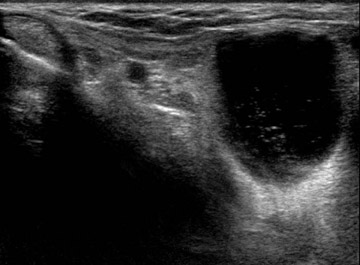
Ultrasound demonstrates a well-defined cystic lesion in close contact to a tendon sheath or joint (Figure 5). It may also show a narrow communication with the above.
MRI shows a well-demarcated cystic lesion with homogeneous low signal intensity on T1W images and high signal intensity on T2W images (Figure 5). The narrow communication or “tail” into the adjacent joint or tendon sheath, when present, is seen well on MRI.11 Cystwalls can demonstrate moderate contrast enhancement.11
Inflammatory lesions
Tendinopathy
Posterior tibial tendinopathy presents as pain and swelling along the medial malleolus. Early diagnosis and treatment can prevent severe disability.12 This commonly occurs in middle-aged or elderly women at risk from hypertension, obesity, SLE, gout, rheumatoid arthritis or Reiter’s syndrome.13 There is a spectrum of disorders ranging from paratendonitis, tendinosis, to partial and eventually complete tearing of the tendon.
The normal Achilles tendon demonstrates uniformly low signal intensity with a flattened or slightly concave anterior border.14 Achilles tendinopathy involving the calcaneal insertion presents as posterior heel pain with swelling and tenderness over the tendon near its insertion.14 It is frequently seen in athletes and may also be seen in patients with inflammatory arthropathy.1
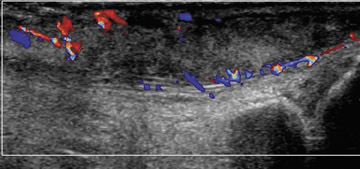
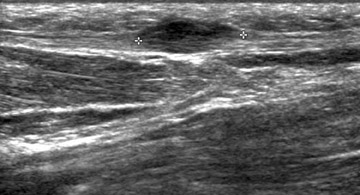
MR in paratendonitis shows circumferential high signal intensity, is slightly hypointense to fluid, and is located distally around the tendon. The tendon itself appears normal with no abnormal signal (Figure 6).13
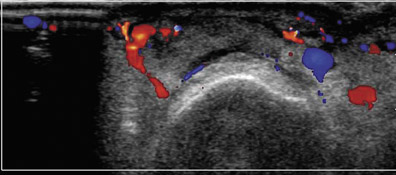
Ultrasound shows increased flow on color Doppler in the peritendon area and an increase in the amount of soft tissue and fluid in the peritendon area (Figure 6).12,13 Tendinosis or tendinopathy is characterized by increased flow within the tendon on color Doppler ultrasound, with heterogeneous echogenicity and an increase in anteroposterior diameter causing a rounding of the tendon (Figure 6). MRIshows an inhomogeneous tendon with abnormal areas of signal intensity and contrast enhancement.12,14
Xanthomas consist of a focal collection of tissue histiocytes containing lipids and can be found in subcutaneous tissue and, less commonly, in tendons. They are seen in patients with hyperlipidemias.14 Tendon xanthomas can present as a swelling over the Achilles tendon near the calcaneal insertion.15 T1W and T2W MRI shows tendon enlargement with heterogeneous signal intensity and a focus of increased signal intensity within the tendon corresponding to the xanthomatous deposit with suppression of the signal on fat-saturated MRI (Figure 7).14
Bursitis
The retrocalcaneal bursa is located between the Achilles tendon insertion and posterior part of the calcaneum. The retroachilleal bursa is situated posterior to the Achilles tendon, beneath the skin.14 Bursitis may present as a tender swelling in the region of the Achilles insertion and may be mistaken clinically for Achilles tendonitis.16 It may present as part of an inflammatory arthropathy or can be an isolatedfinding in athletes. The intermetatarsal region is another common site for bursitis. Bursal fluid appears as high in signal intensity on T2W and short-tau inversion-recovery (STIR) images and as low signal on T1W images (Figure 8).14,17 Ultrasound shows hypoechoic bursal fluid(Figure 8).
Infection
Diabetic patients are prone to foot infections and ulceration due to factors like neuropathy, arteriopathy and increased susceptibility to infection.18,19 Infection may involve the soft tissues as cellulitis, osteomyelitis or septic arthritis (Figure 9). Most of the foot infections result from contiguous spread from an ulcer or skin defect.18–20 Ulcers are most commonly located in the forefoot, around the first andfifth metatarsal heads and the distal phalanx of the great toe and occur in the region of the heel.18 They are uncommon in the midfoot. These areas also correspond to the most common sites of soft-tissue infection and osteomyelitis.18
MRI demonstrates loss of normal marrow or soft-tissue signal with low signal intensity on T1W images, high signal intensity on T2Wand STIR and enhancement postintravenous administration of gadolinium. Marrow signal abnormality may also be associated with other conditions like fractures, inflammatory arthropathy, tumors, neuropathic joint or technical factors like inhomogeneous fat suppression.18–20 In such cases, secondary features like the presence of an ulcer, cellulitis, soft-tissue mass, abscess, sinus tract and cortical interruption increase the likelihood of osteomyelitis.19 Septic arthritis is seen most frequently in the first and fifth metatarsophalangeal jointsin the forefoot, similar to the distribution of ulcers and osteomyelitis.18 MRI shows increased joint fluid, thickening of the synovium with contrast enhancement, and bone erosions with signal changes related to marrow edema.18
Fibrous lesions
Superficial fibromatosis
Plantar fibromatosis, also known as Ledderhose’s disease, is characterized by a non-neoplastic development of fibrous nodules on the superficial surface of the plantar aponeurosis. Single or multiple nodules can be found, most frequently at the medial aspect of the plantar fascia.1 In 20% to 50% of cases the disease occurs bilaterally.21,22 The condition is associated with other superficial fibromatoses, such as palmar fibromatosis and penile fibromatosis (Peyronie’s disease). Men are affected twice as commonly as women, with 10% to 65% of cases having associated palmar fibromatosis.2
Ultrasound demonstrates a well-defined low-echogenicity nodular thickening of the plantar fascia (Figure 10). MRI reveals characteristic features: on T1W and T2W images, most lesions are isointense to hypointense to the adjacent muscle.
Deep fibromatosis
Deep fibromatosis, also known as aggressive fibromatosis or extra-abdominal desmoid, is the most common soft-tissue tumor of thefoot.3 It originates from connective tissues of the muscle, fascia or aponeurosis.1,2 It is characterized by an aggressive, infiltrative growth pattern with a high recurrence rate following surgical resection.21 Aggressive fibromatosis does not metastasize, and multicentric lesions occur.2 Patients in the first 3 decades of life are most commonly affected.2
Histologically, deep fibromatosis consists of a variable amount of fibroblasts with collagenous and myxoid stroma, represented on MRI as heterogeneous signal characteristics. MRI reflects the aggressive growth pattern with displacement or entrapment of adjacent tissues. Most lesions demonstrate low-to-intermediate signal intensity on T1W images and high signal intensity on T2W images.1 Moderate-to-marked contrast enhancement is seen, with the exception of the intralesional bands. They are of low signal intensity on all pulse sequences, representing areas of dense collagenous matrix.21
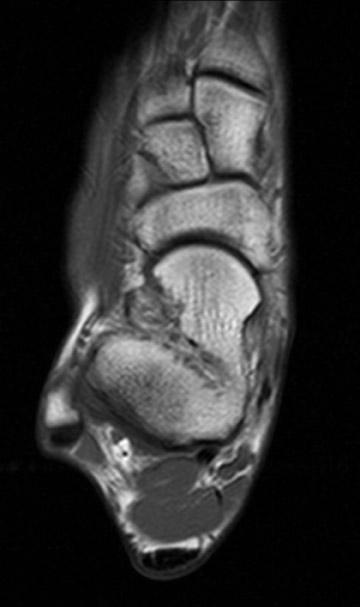
Accessory muscles
An accessory soleus muscle is an uncommon anatomic variant found in 10% of individuals, that may present as a soft-tissue mass in the posteromedial aspect of the ankle and can cause pain related to exercise.23 The muscle arises from the anterior surface of the soleusor from the fibula and soleal line of the tibia.24 It inserts either onto the Achilles tendon or as a separate tendon on the posteromedial aspect of the calcaneus.23
MRI is the examination of choice to confirm the nature of the mass and clearly differentiate it from other tumors (Figure 11). No treatment is required if it is an incidental and asymptomatic finding, however complete resection of the supernumerary muscle is advised in symptomatic cases.24
The peroneus quartus muscle is more common, presenting in 13% to 22% of the population.23 It can originate as a separate muscle from the fibula or from the peroneus brevis or longus muscles and inserts onto the peroneal tubercle or retrotrochlear eminence of the calcaneus.23,25 MRI at the level of the malleolus demonstrates the muscle as medial or posterior to both peroneal tendons. It is usually an incidental finding, but may give rise to lateral ankle pain and instability of the ankle joint. It may also predispose to subluxation of peroneal tendons.25
Conclusion
MR imaging in conjunction with ultrasound and careful correlation with clinical history are helpful for specific diagnosis in the majority of palpable lesions around the foot. MRI is the modality of choice in differentiating palpable masses around the foot from anatomical variants like accessory muscles.
REFERENCES
- Waldt S, Rechl H, Rummeny EJ, Woertler K. Imaging of benign and malignant soft tissue masses of the foot. Eur Radiol. 2003;13:1125-1136.
- Llauger J, Palmer J, Monill JM, et al. MR imaging of benign soft-tissue masses of the foot and ankle. Radiographics.1998;18:1481-1498.
- Kransdorf MJ, Murphey MD. Soft tissue tumors in a large referral population. In: Kransdorf MJ, Murphey MD, Eds. Imaging of soft tissue tumors. Philadelphia, Pa:Saunders;1997:3-37.
- Murphey MD, Fairbairn KJ, Parman LM, et al. Musculoskeletal angiomatous lesions: Radiologic-pathologic correlation. Radiographics. 1995;15:893-917.
- Cohen JM, Weinreb JC, Redman HC. Arteriovenous malformations of the extremities: MR imaging. Radiology. 1986;158:475-479.
- Ly JQ, Gilbert BC, Davis SW, et al. Lymphangioma of the foot. AJR Am J Roentgenol. 2005;184:205-206.
- Kransdorf MJ, Moser RP Jr, Meis JM, Meyer CA. Fat-containing soft tissue masses of the extremities. Radiographics. 1991;11:81–106.
- Jelinek JS, Kransdorf MJ, Shmookler BM, et al. Giant cell tumor of the tendon sheath: MR findings in nine cases. AJR Am J Roentgenol. 1994;162:919-922.
- De Beuckeleer L, De Schepper A, De Belder F, et al. Magnetic resonance imaging of localized giant cell tumour of the tendon sheath. Eur Radiol. 1997;7:198-201.
- Blacksin MF, Doo-Hoe H, Hameed M, Aisner S. Superficial soft tissue masses of the extremities. Radiographics. 2006;26:1289-1304.
- Steiner E, Steinbach LS, Schnarkowski R, et al. Ganglia and cysts around joints. Radiol Clin North Am. 1996;34:395–425.
- Premkumar A, Perry MB, Dwyer AJ, et al. Sonography and MR imaging of posterior tibial tendinopathy. AJR Am J Roentgenol. 2002;178:223–232.
- Schweitzer ME, Karasick D. MR Imaging of disorders of the posterior tibialis tendon. AJR Am J Roentgenol. 2000;175:627–635.
- Narváez JA, Narváez J, Aguilera ROC, et al. Painful heel: MR imaging findings. Radiographics. 2000;20:333–352.
- Fahey JJ, Stark HH, Donovan WF, Drennan DB. Xanthoma of the Achilles tendon: Seven cases with familial hyperbetalipoproteinemia. J Bone Joint Surg Am.1973;55:1197–1211.
- Kier R, McCarthy S, Dietz MJ, Rudicel S. MR appearance of painful conditions of the ankle. Radiographics. 1991;11:401-414.
- Bottger BA, Schweitzer ME, El-Noueam KI, Desai M. MR imaging of the normal and abnormal retrocalcaneal bursae. AJR Am J Roentgenol. 1998;170: 1239–1241.
- Ledermann HP, Morrison WB, Schweitzer ME. MR image analysis of pedal osteomyelitis: Distribution, patterns of spread and frequency of associated ulceration and septic arthritis. Radiology. 2002; 223:747–755.
- Morrison WB, Schweitzer ME, Batte WG. Osteomyelitis of the foot: Relative importance of primary and secondary MR imaging signs. Radiology.1998;207:625-632.
- Craig JG, Amin MB, Wu K, et at. Osteomyelitis of the diabetic foot: MR imaging pathologic correlation. Radiology. 1997;203:849-855.
- Dinauer PA, Brixey CJ, Moncur JT, et al. Pathologic and MR imaging features of benign fibrous soft-tissue tumors in adults.Radiographics. 2007;27: 173-187.
- Lee TH, Wapner KL, Hecht PJ. Plantar fibromatosis. J Bone Joint Surg Am. 1993;75:1080–1084.
- Link SC, Erickson SJ, Timins ME. MR imaging of the ankle and foot: Normal structures and anatomic variants that may simulate disease. AJR Am J Roentgenol. 1993;161:607-612.
- Kouvalchouk JF, Lecocq J, Parier J, Fischer M. The accessory soleus muscle: a report of 21 cases and a review of the literature. Rev Chir Orthop Reparatrice Appar Mot.2005;91:232-238.
- Cheung YY, Rosenberg ZS, Ramsinghani R, et al. Peroneus quartus muscle: MR imaging features. Radiology. 1997;202:745-750.
Related Articles
Citation
. Imaging benign soft tissue lesions of the foot. Appl Radiol.
October 26, 2009