How we do it: Localizing-small-pulmonary-nodules
Images


HOW WE DO IT
Localizing small pulmonary nodules for resection
There seems to be increasing interest by caregivers and patients to rapidly diagnose the etiology of small pulmonary nodules (e.g., suspected metastases, fungal infiltrates or PTLD). Lesions > 1 cm and those abutting or near to the pleural surface are usually amenable to transthoracic image-guided core or fine needle aspiration (FNA) biopsy. Small and deeply located nodules have in the past required open thoracotomy and lobectomy for diagnosis since the lesions could not be identified by inspection or palpation because they are generally not palpable and they do not distort the lung or pleural surface. In order to assist diagnosis and surgical resection, a nodule can be localized for removal using a minimally invasive approach. A Kopans Breast Lesion Localization Needle (Cook Inc., Bloomington, Indiana) is an excellent tool along with sterile 1% methylene blue (Akorn, Inc., Lake Forest, Illinois) (Figure 1) to visually identify the location of the nodule so that it can be precisely removed thoroscopically. This approach will minimize the amount of tissue removed while maximizing the probability of successfully obtaining the target nodule for histologic diagnosis. The redundant use of methylene blue (MB) in addition to the localization needle, is to ensure that the location of the nodule is identifiable, even if the Kopans wire is dislodged prior to or during the video-assisted thoracoscopic procedure.
TECHNIQUE
Preoperatively, high-resolution CT is the method of choice and is used for diagnostic confirmation and route. The procedure is performed under general anesthesia (GA) and the patient is transported to the operating room (OR)directly from the IR suite after needle localization of the pulmonary nodule. Rapid transport to the OR decreases the likelihood of migration of the localization wire and diffusion of the methylene blue. Although a pneumothorax may occur, it is uncommon for it to become symptomatic. If it does become problematic, needle aspiration may be performed with chest tube placement, only required in rare cases.
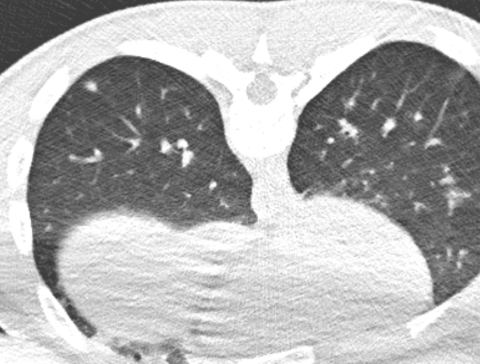
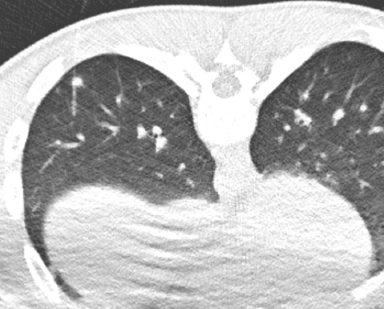
At the time of the procedure, a multi-detector CT in the CT suite or cone beam CT in the IR suite is performed and the nodule re-identified. Route trajectory is determined utilizing several factors, including the avoidance of crossing fissures and the use of the shortest, most direct route to the target nodule. The skin entry site is confirmed using an E-Z-Mark dot(E-Z-M Inc., Westbury, NY) and marking on the skin surface with washable ink, when using a multi-detector CT for imaging guidance, or by placement of a hemostat on the skin surface and then marking with washable ink when cone beam CT with fluoroscopic overlay is utilized. The chest wall is prepared and draped in sterile fashion and 1% lidocaine is slowly injected into the skin at the pre-determined entry site. The “fish hook” localization wire is removed from the needle and the tip submerged in methylene blue (Figure 1). The wire is then reinserted into the Kopans needle, with the tip of the wire positioned at the tip of the needle. Methylene blue dye is an important backup to the hooked needle since the Kopans localization wire may accidently come out of the lung. It is essential to use a miniscule volume of methylene blue (< 0.1 mL) or the entire hemithorax will become “Smurf” blue, masking the pleural entry site of the needle to the target nodule, if the wire were to become dislodged. After the localization needle is prepped, the dermatotomy is made. Using CT-guidance with the previously determined depth and angle, the Kopans localization needle is inserted so that the tip is adjacent to and 1-5 mm deep to the nodule (Figure 2). The guide needle is removed after ideal position of the needle tip is confirmed with CT or cone beam CT. The Kopans needle is removed over the wire as if doing a catheter exchange, leaving the hooked wire in place. The external portion of the wire is then looped on the skin surface and covered with gauze and a transparent dressing. More than one nodule may be localized during the same session by this method1,2 . It is valuable to position the needle in the desired location on the first pass. Pneumothorax or pulmonary hemorrhage may move or obscure the nodule if this is not achieved. The child is then moved to the stretcher and immediately transported to the OR for thoracoscopic removal of the nodule (and Kopans wire). Keep in mind that methylene blue stains skin and clothing and will not readily wash off.
Post-procedural care is provided by the anesthesia and surgical services since the child is immediately transported to the OR for video-assisted thoracoscopic resection of the nodule(s) and Kopans wire. It is important to communicate the position of the wire tip in relation to the nodule to the surgeon, and to advise the anesthesiologist of the potential for pneumothorax following the localization procedure.
In our experience, small asymptomatic pneumothorax (PT) commonly occurs. In most children, the PT is not under tension and does not cause difficulty in either oxygenating or ventilating the child. Although possible, neither pulmonary infection nor empyema has occurred in our patients. Self-limited pulmonary hemorrhage usually occurs along the wire tract, as it does along the biopsy needle tract after lung biopsy, but this is considered an expected outcome of the procedure that is simply more conspicuous due to the air/fluid interface.
CONCLUSION
In conclusion, CT-guided pulmonary nodule localization and marking is a safe technique in children, with a high diagnostic yield and a low complication rate following thoracoscopic resection3-6. Such a minimally invasive alternative to open thoracotomy is emblematic of the successful collaboration possible between surgical and interventional services.
REFERENCES
- Thaete FL, Peterson MS, Plunkett MB, Ferson PF, Keenan RJ, Landreneau RJ (1999) Computed tomography-guided wire localization of pulmonary lesions before thoracoscopic resection: results in 101 cases. J Thorac Imaging 14:90-98.
- Kakuda J, Omari B, Renslo R, Scott R, Baumgartner F (1997) CT guided needle localization for video-thoracoscopic resection of pulmonary nodules. Eur J Med Res 2:340-342.
- Waldhausen JH, Shaw DW, Hall DG, Sawin RS (1997) Needle localization for thoracoscopic resection of small pulmonary nodules in children. J Pediatr Surg. 32:1624-1625.
- Partrick DA, Bensard DD, Teitelbaum DH, Geiger JD, Strouse P, Harned RK (2002) Successful thoracoscopic lung biopsy in children utilizing preoperative CT-guided localization. J Pediatr Surg. 37:970-973.
- Wicky S, Mayor B, Cuttat JF, Schnyder P (1994) CT-guided localizations of pulmonary nodules with methylene blue injections for thoracoscopic resections. Chest. 106:1326-1328.
- Fernandez MT, Bustos A, Ferreiros J, Gomez A, Hernando F, Torres A (2000) [Localization of lung nodules with CT-guided hookwire before videothoracoscopic surgery]. Med Clin (Barc). 114:333-335.
Citation
How we do it: Localizing-small-pulmonary-nodules. Appl Radiol.
June 19, 2019