Heart Inflammation After COVID Vaccine Found Only in Patients With Acute Myocarditis
 A study published in Radiology: Cardiothoracic Imaging reports that researchers found evidence of heart muscle inflammation in a small number of patients with acute myocarditis after COVID-19 vaccination, but not in patients without acute myocarditis.
A study published in Radiology: Cardiothoracic Imaging reports that researchers found evidence of heart muscle inflammation in a small number of patients with acute myocarditis after COVID-19 vaccination, but not in patients without acute myocarditis.
“To our knowledge, this is the first prospective study to report comprehensive cardiac investigations and imaging in both symptomatic and asymptomatic patients after COVID-19 vaccination,” said the study’s senior author Kate Hanneman, M.D., M.P.H., associate professor in the Department of Medical Imaging and director of cardiac imaging research at the University of Toronto in Toronto, Canada.
Billions of people worldwide have received at least one dose of a COVID-19 vaccine. Some instances of myocarditis (non-ischemic inflammation of the heart muscle) have been reported following administration of mRNA-based COVID-19 vaccines. Myocarditis can affect the heart’s rhythm and ability to pump blood and may leave behind lasting damage in the form of scarring of the heart muscle.
Most instances of myocarditis after COVID-19 vaccination have occurred in adolescent and young adult males. However, the overall risk is very low.
Some patients may experience cardiac symptoms after vaccination, including shortness of breath, palpitations, and chest pain, yet do not meet diagnostic criteria for acute myocarditis.
“We know that some patients are at risk of myocarditis following mRNA-based
COVID-19,” Dr. Hanneman said. “However, there are limited data on potential myocardial tissue changes in patients who are asymptomatic after COVID-19 vaccination. Similarly, we have very limited data to date on patients who present with new symptoms after vaccination but do not meet diagnostic criteria for acute myocarditis.”
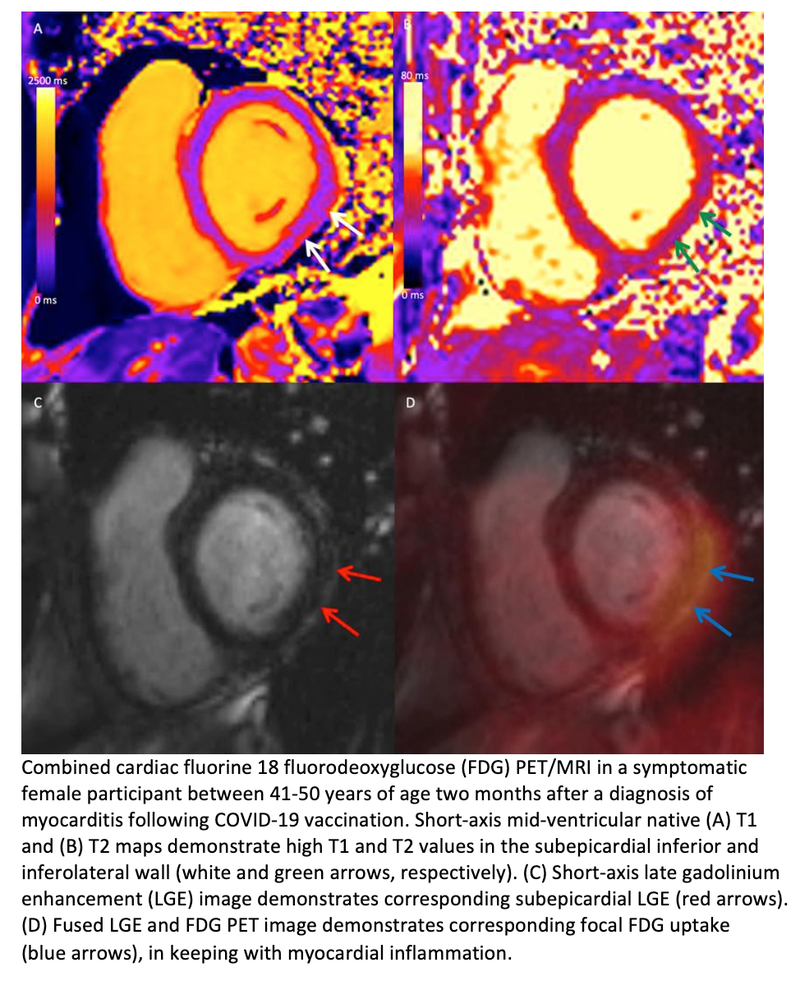
Cardiac MRI plays an important role in the assessment of acute myocarditis with unparalleled ability for noninvasive characterization of myocardial tissue. Cardiac fluorine 18 (18F) fluorodeoxyglucose (FDG) PET allows for assessment of changes in myocardial metabolism.
For this prospective study, Dr. Hanneman and a multi-disciplinary team of radiology, cardiology and vascular biology researchers set out to investigate cardiac effects of COVID-19 vaccination at two-month follow-up and relate cardiac symptoms to myocardial tissue changes on FDG PET/MRI, blood biomarkers, health-related quality of life and adverse outcomes.
Fifty-four participants were evaluated a median of 72 days after COVID-19 vaccination. Seventeen were symptomatic with myocarditis, 17 were symptomatic without myocarditis, and 20 were asymptomatic.
No participants in the symptomatic without myocarditis or asymptomatic groups had focal FDG uptake, myocardial edema or impaired ventricular function. Two participants with symptomatic myocarditis had focal FDG uptake. Health-related quality of life was lower in the symptomatic myocarditis group than the asymptomatic group. There were no adverse cardiac events beyond myocarditis in any participant.
“None of the symptomatic participants in our study who did not meet diagnostic criteria for acute myocarditis had elevated troponin levels, impaired left ventricular function, or detectable cardiac inflammation two months after COVID-19 vaccination,” Dr. Hanneman said. “This suggests that symptoms alone are a poor indicator of myocardial injury after vaccination.”
The results also suggested that subclinical myocardial injury is not common after COVID-19 vaccination, based on normal cardiac PET, ECG, and blood biomarker findings in the asymptomatic patient group. The researchers hope these findings reassure patients who did not experience symptoms after COVID-19 vaccination but worry about the possibility of subclinical cardiac disease.
Dr. Hanneman cautioned that further study is needed to investigate non-cardiovascular causes of symptoms after vaccination in individuals who do not meet diagnostic criteria for acute myocarditis.
Related Articles
Citation
Heart Inflammation After COVID Vaccine Found Only in Patients With Acute Myocarditis. Appl Radiol.
March 9, 2023