Giant hypothalamic hamartoma
Images
CASE SUMMARY
A 9-year-old girl was referred to our endocrinology service for short stature. She was otherwise well without a history of headaches or visual symptoms. She was a full-term baby with normal birth weight and no prenatal abnormalities. Upon endocrinologic evaluation, she was found to have central growth hormone deficiency and hypothyroidism. She was referred to radiology for a brain MRI to rule out a structural cause for her multiple endocrinopathies.
IMAGING FINDINGS
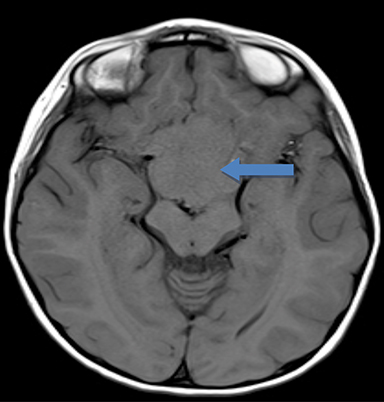
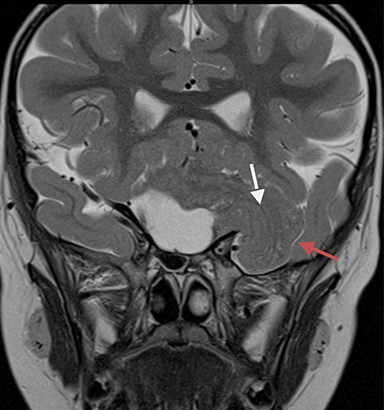
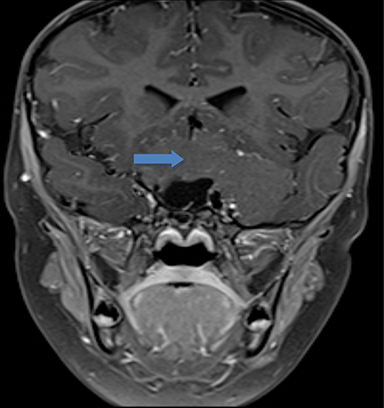
MR imaging of the brain without and with contrast was performed, and showed a large, slightly heterogeneous mass in the suprasellar region. The mass was isointense to the brain on the unenhanced T1- and T2-weighted images (Figures 1 and 2), without abnormal enhancement (Figure 3). The mass had a cerebriform appearance, resembling a ‘brain-within-a-brain’ architecture. There was associated mass effect on the optic chiasm, and superolateral displacement of the bilateral internal carotid arteries. There was no hydrocephalus or vascular encasement/narrowing. The pituitary gland was separate from the mass, and the sella was not expanded.
DIAGNOSIS
Giant hypothalamic hamartoma. Differential diagnosis includes craniopharyngioma, pituitary macroadenoma, and germ cell tumor.
DISCUSSION
Hypothalamic hamartomas are congenital malformations characterized by disorganized but normal neural tissue in the hypothalamic region.1 Patients with hypothalamic hamartomas classically present with gelastic seizures (laughing seizures), but other seizures types may also occur.2 Hypothalamic hamartomas are also an important structural cause of precocious puberty, and have been reported to be the most common cause of central precocious puberty.3 Treatment is usually medical, with a focus on correcting any associated endocrinologic abnormalities or controlling seizures. Surgery is usually reserved for medically refractory seizures, or precocious puberty in some cases.4,5
On imaging, hypothalamic hamartomas are similar in appearance to distorted but normal brain tissue.6 Hypothalamic hamartomas arise from the floor of the third ventricle and project into the suprasellar cistern. When large, these lesions can distort the suprasellar cistern and compress or displace multiple structures including the optic chiasm and prechiasmatic optic nerves, internal carotid arteries, and pituitary stalk. On CT, these lesions appear isodense to the normal brain parenchyma, and do not enhance after contrast administration. Hemorrhage and calcification within hypothalamic hamartomas are exceedingly rare. MRI imaging shows a soft tissue mass in the hypothalamic region that is isointense to brain on T1 and T2, without abnormal enhancement.
The differential diagnosis for a suprasellar mass in a pediatric patient is extensive,7 but the majority of the lesions are uncommon. Major considerations for a solid suprasellar mass would include a craniopharyngioma, pituitary macroadenoma, or a germ cell tumor (including teratomas). Craniopharyngiomas in pediatric patients are usually of the adamantinomatous type. These lesions are typically cystic, contain calcifications, and enhance after contrast administration.8 Pituitary macroadenomas usually expand the sella, and may extend into the suprasellar cistern when large. These lesions have a propensity to invade the cavernous sinus, and may encase the internal carotid artery without causing significant narrowing. Suprasellar germ cell tumors (most commonly germinomas) arise from the hypothalamic region and grow along the pituitary stalk. When large, they present as heterogeneous masses with enhancement and mild restricted diffusion. These tumors have a tendency for cerebrospinal fluid dissemination, and additional enhancing foci elsewhere in the ventricles should be viewed with suspicion and considered to be metastases until proven otherwise.
CONCLUSION
Hypothalamic hamartomas are an important cause of precocious puberty and epilepsy in young patients. When small in size, these lesions can be subtle and easily overlooked due to their similarity to normal brain tissue. When large, a cerebriform or ‘brain-within-a-brain’ appearance helps to clinch the diagnosis of a hypothalamic hamartoma and distinguish this lesion from other pediatric suprasellar masses.
REFERENCES
- Coons S, Retake H, Prenger E, et al. The histopathology of hypothalamic hamartomas: Study of 57 cases. Journal of Neuropathology and Experimental Neurology. 2007;66:131-141.
- Mullati N, Selway R, Nashef L, et al. The clinical spectrum of epilepsy in children and adults with hypothalamic hamartoma. Epilepsia. 2003;44:1310-1319.
- Kornreich L, Horev G, Blaser S. et al. Central precocious puberty: Evaluation by neuroimaging. Pediatric Radiology. 1995;25:7-11.
- Albright A, Lee P. Neurosurgical treatment of hypothalamic hamartomas causing precocious puberty. Journal of Neurosurgery. 1993;78:77-82
- Nishio S, Morioka T, Fukui M, et al.Surgical treatment of Intractable Seizures Due To Hypothalamic Hamartomas. Epilepsia. 1994;35:514-519.
- Barkovich JA, Raybaud C. Pediatric Neuroimaging, 5th Edition.
- Rheinboldt M, Blasé J. Exophytic hypothalamic cavernous malformation mimicking an extra-axial suprasellar mass. Emergency Radiology. 2011;18:363-367.
- Kollias S, Barkovich A, Edwards M. Magnetic resonance analysis of suprasellar tumors of childhood. Pediatric Neurosurgery. 1991;17:284-303.
Citation
J CMA, J KVP. Giant hypothalamic hamartoma. Appl Radiol. 2017;(5):31A-31B.
May 9, 2017