Focused Ultrasound May Help Identify Stroke Biomarkers
Images
A molecule called glial fibrillary acidic protein (GFAP) rose significantly in the blood of patients who underwent high-intensity focused ultrasound (HIFU), a procedure that is used to treat tremors and causes damage similar to a small stroke. UT Southwestern Medical Center scientists published their discovery in Brain Communications, revealing a potential biomarker for stroke and could eventually lead to blood tests that quickly diagnose brain injuries.
“This is the first study to use HIFU as a controlled model to evaluate brain injury biomarker dynamics,” said Bhavya R. Shah, MD, Associate Professor of Radiology and Neurological Surgery at UT Southwestern as well as in the Advanced Imaging Research Center. He’s also an Investigator in the Peter O’Donnell Jr. Brain Institute and a member of the Center for Alzheimer’s and Neurodegenerative Diseases. “The ability to pair a timed pre- and post-HIFU measurement with precise lesion delivery is unprecedented and offers extraordinary potential for validating blood biomarkers of brain injury in a way that has not been done before.”
Dr Shah co-led the study with Nil Saez-Calveras, MD, a fourth-year Neurology resident at UT Southwestern.
Every year, nearly 800,000 people in the U.S. have a stroke, according to the Centers for Disease Control and Prevention. This condition is characterized by inadequate blood flow to regions of the brain, causing brain cells to die from a lack of oxygen. Although strokes can be diagnosed using MRI, delays in care can lead to worse outcomes, explained Dr Shah, who is also a member of the Harold C. Simmons Comprehensive Cancer Center at UTSW.
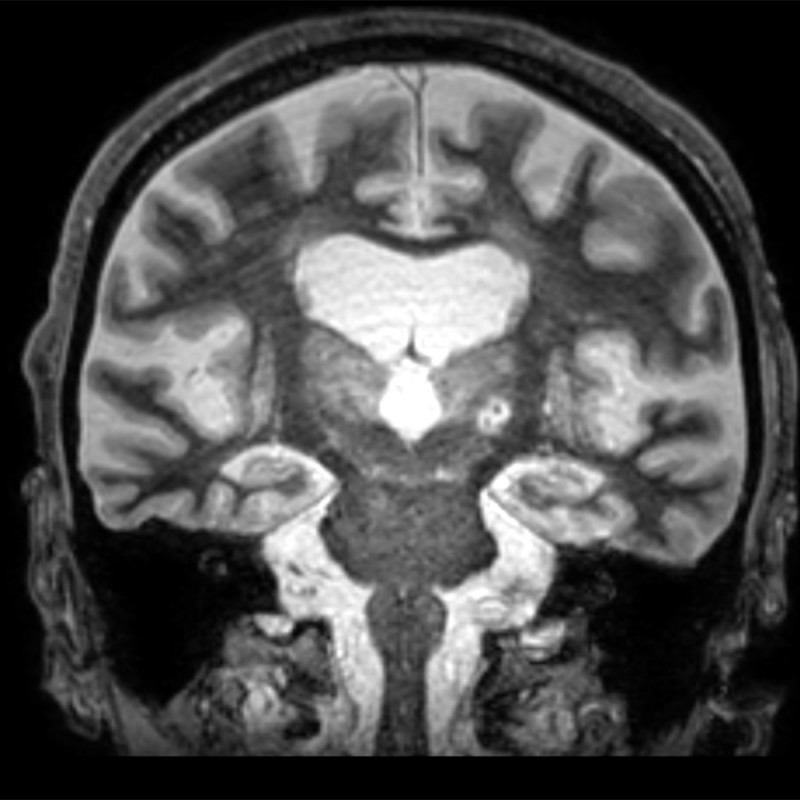
In 2016, the Food and Drug Administration approved a new treatment for tremor disorders in which physicians use HIFU to burn away a targeted portion of the thalamus, the brain region where many types of tremors originate. Six years later, Dr Shah and his colleagues reported a new technique that significantly improved HIFU targeting for this treatment. Recently, the team realized that the controlled brain injury caused by this therapy looks indistinguishable from stroke in brain imaging – the two types of damage have several features in common, including how the brain responds to these injuries, Dr Shah said.
The researchers wondered whether this similarity could help them achieve a long-held goal of diagnosing stroke and brain injury through markers in the blood, Dr Saez-Calveras said. Research toward this end has been stymied by a lack of blood measurements taken before stroke occurs, differences in where brain injury occurs in stroke patients, uncertainty about when a stroke occurred, and physiological differences among patients.
They reasoned that using the HIFU treatment as a research tool could overcome these challenges. In the new study, 30 patients at UTSW with tremor-dominant Parkinson’s disease or another movement disorder called essential tremor received HIFU to treat these conditions. The researchers collected blood samples immediately before the procedure, as well as one hour and 48 hours after. They then measured the concentrations of five molecular markers that previous research suggested might hold promise for diagnosing brain injuries: GFAP, neurofilament light chain, amyloid-beta 40, amyloid-beta 42, and phosphorylated tau 181 (pTau-181).
Forty-eight hours after HIFU treatment, all the molecular markers except pTau-181 had risen significantly; however, GFAP rose the most, more than quadrupling on average compared to pre-treatment measurements.
Based on these findings, Dr Saez-Calveras said, GFAP could hold significant promise as a marker for stroke and other types of brain injury. The researchers plan to continue to study GFAP’s rise at different points after HIFU treatment to determine its feasibility as a diagnostic marker for brain injury. In addition, they are investigating hundreds of other molecules as potential candidates that might suggest possible brain injury earlier than GFAP. The team has also begun collecting blood from emergency stroke patients to determine if GFAP is elevated.
“Our study validates the use of focused ultrasound as a platform for biomarker discovery for brain diseases,” Dr Saez-Calveras said.