Dynamic MR imaging of pelvic floor dysfunction
Images





Functional disorders of the pelvic floor such as pelvic organ prolapse and defecation dysfunction are increasingly being recognized as common health problems primarily affecting older, multiparous women. About 15% of women are affected by some pelvic floor disorder.1
Patients present with various symptoms, such as constipation, fecal or urinary incontinence, a feeling of incomplete emptying, pelvic pain or gross organ protrusion.1,2 Obstructed defecation syndrome (ODS) is a pathological condition characterized by impaired defecation upon the urge to defecate.1,3
The aim of this review is to familiarize radiologists with the anatomic complexity of the pelvic floor, as well as the pathological features of and the advantageous role of MRI assessment in pelvic floor dysfunction.
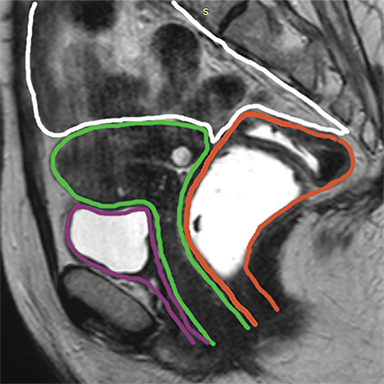
The female pelvis is anatomically divided into three functional compartments: the anterior (urinary bladder and urethra), the middle (vagina, cervix and uterus) and the posterior (anorectum). All three act as one unit (Figure 1).4
Traditionally, urinary incontinence has been evaluated by urologists, reproductive tract problems by gynecologists, and anorectal problems by colorectal surgeons and gastroenterologists.5,6 The basic diagnostic approach for surgeons and clinicians is clinical examination, performed with the patient performing the Valsalva maneuver in the lithotomy position.7, 8
The clinical examination, however, is not reliable for assessing evacuation abnormalities and frequently underestimates the number of affected compartments compared to dynamic cystocolpoproctography (DCP) and dynamic MRI of the pelvic floor.9, 10 During defecation, maximal levator ani relaxation provides the highest stress to the pelvic floor, which is needed to diagnose defecation disorders and pelvic organ prolapse.4
MR imaging of the pelvic floor was first introduced in 1991 by Yang et al and Kruyt et al. MRI has since gained widespread popularity, as it can noninvasively visualize organs in the pelvis and the supportive pelvic structures in greater detail than can DCP. It enables the concomitant assessment of all three compartments.11 Indeed, MRI should be used routinely in preoperative planning for pelvic floor surgery.
MRI Technique: Patient preparation and protocol
Considerable variations in patient preparation and MR imaging sequences have been published. Such differences relate to available equipment and personal preferences.1, 2, 11-16 Images presented in this review were performed on a 1.5T closed MRI system. Dynamic MR imaging consists of imaging patients at rest, during squeezing, straining and defecation. Rectal filling is highly preferable, as it produces the feeling of a full rectum and permits evaluation of the defecation phase. The patient’s position is supine and a torso phased-array coil is placed around the lower pelvis. MR study protocol starts with obtaining scout images. We use T1-weighted images (T1WI) localizer sequences to identify the midsagittal section. The examination proceeds with by obtaining T1WI and T2WI resting anatomic images of the pelvis in which muscle tears and thinning can be visualized.
For dynamic MRI of the pelvic floor, use steady-state imaging sequences.7 High temporal resolution and excellent contrast make it well suited for evaluation of organ movement. The patient is asked to defecate while on the MR scanner table and then asked to go to the toilet to completely empty the urinary bladder, rectum or rectocele. Post-defecation dynamic sequences are repeated at maximum straining to analyze if any fecal content or ultrasound gel remains in a rectocele and to evaluate the presence of enterocele, peritoneocele, or sigmoidocele. The protocol can be completed in 20 minutes.
Anatomy of the pelvic floor
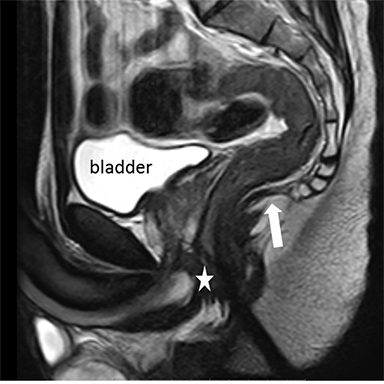
The endopelvic fascia is a layer of connective tissue that provides important anterior and lateral passive support to the vagina, urinary bladder and urethra. The fascia around the vagina and uterus forms a sacrouterine or cardinal ligament that suspends and supports the vaginal vault and pulls it towards the rectum.1,2,17 The pelvic diaphragm consists of the levator ani muscle, which has three important components: the ileococcygeus, pubococcygeus and puborectalis muscles. The pubococcygeus muscle fuses posteriorly to form a midline raphe, called the levator plate. The puborectalis muscle originates from the pubic symphysis and forms a sling around rectum at the anorectal junction. It aligns with the external anal sphincter.1,2
The urogenital diaphragm is composed of connective tissue and the deep transverse perineal muscles. The perineal body is the important anchoring structure for the muscles and ligaments of the urogenital diaphragm: rectovaginal fascia, (condensation of the endopelvic fascia), external anal sphincter and superficial and deep transverse muscles (Figure 2).1,2
Interpretation of MR images
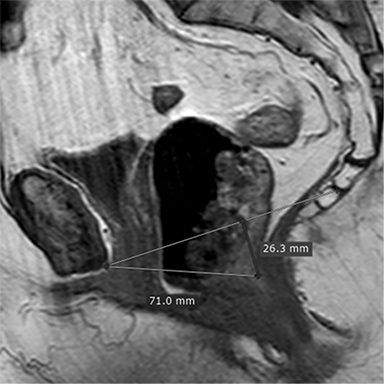
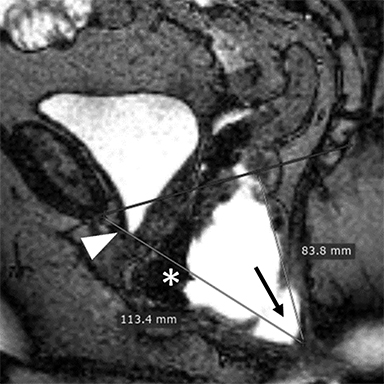
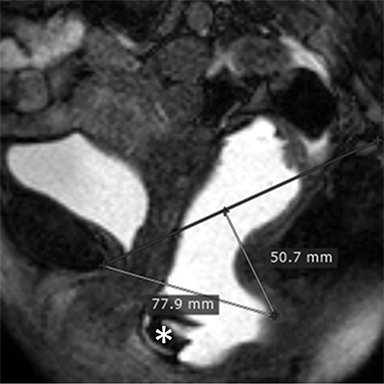
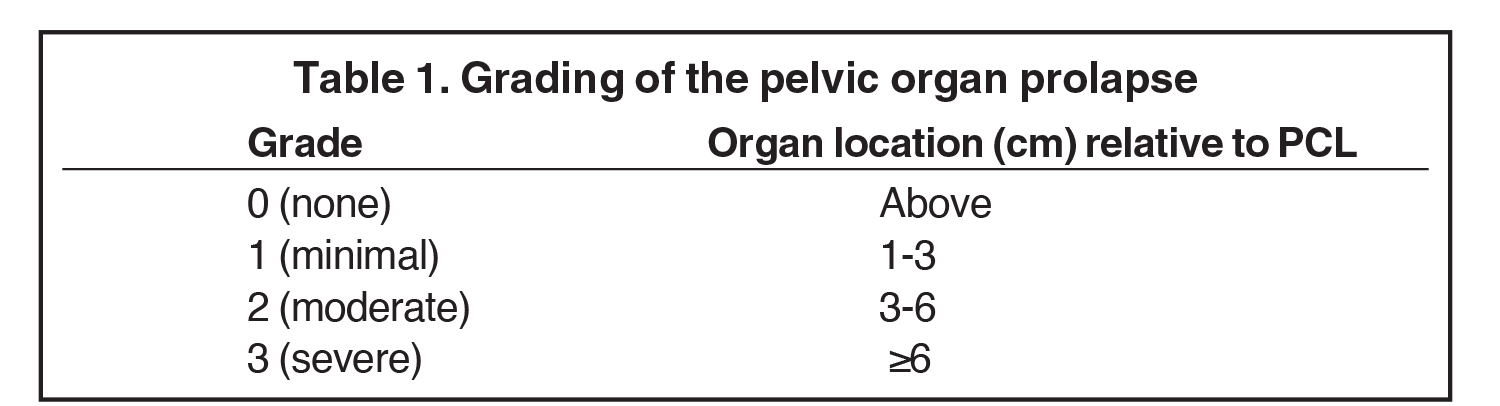
Several classification systems exist for evaluating dynamic MRI of the pelvic floor. Most radiologists use the pubococcygeal line (PCL) as representing the level of the pelvic floor and as a reference for grading pelvic organ prolapse. In normal anatomy, the PCL line is parallel to the levator plate. The PCL is based on the bony pelvis structures, which serve as attachment points for the soft-tissue structures of the pelvis. It is drawn from the inferior border of the pubic symphysis to the last coccygeal joint. On static images the position of the urinary bladder neck, cervix, and anorectal junction are detected and are used as the landmarks for measuring the organ descent. The distance (vertical lines) from the PCL to the landmarks should be measured on images obtained during maximal straining. The distance is graded by the rule of 3 (Table 1).15
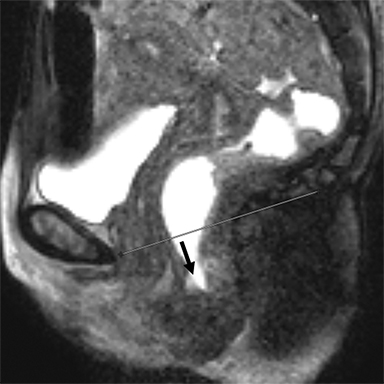
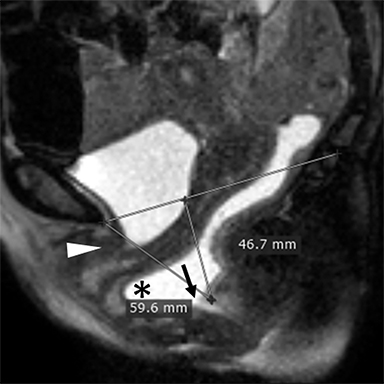
In the HMO system (H-line, M-line and Organ prolapse), according to Comitter et al, two additional lines can be measured (Figure 3). The H-line is drawn from the inferior pubic symphysis to the posterior wall of the rectum at the level of anorectal junction, and it represents the anteroposterior hiatal dimension, allowing the grading of the maximal widening of the pelvis sling during straining. M-line (muscular pelvic floor relaxation) runs perpendicular from the PCL to the lowest aspect of the H line and is indicative of the descent of the levator hiatus from the PCL. The O classification (organ prolapse) characterizes the degree of pelvic organ prolapse below the H-line during maximum straining.15
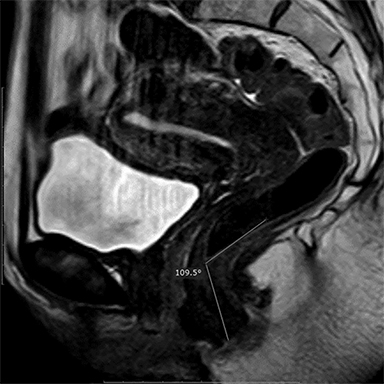
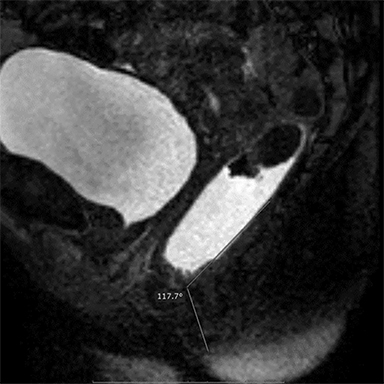
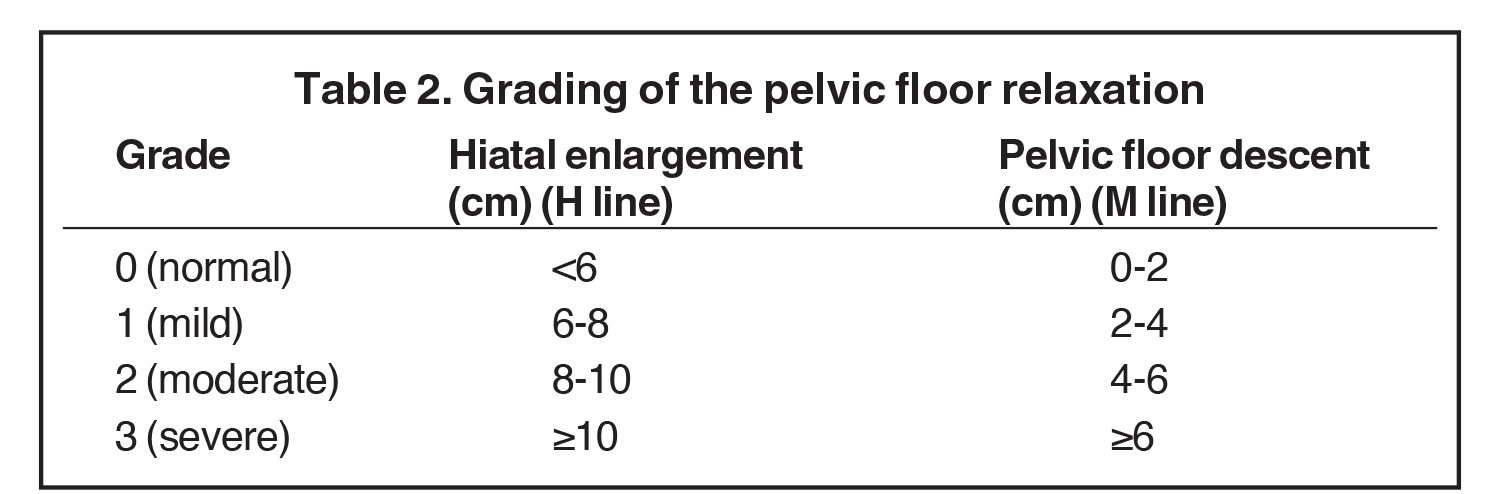
Elongation of the H and M lines is the indicator of pelvic floor relaxation, representing widening of the levator plate and descent of the levator hiatus (Table 2).2 The H line and M line in normal women measure approximately 5 and 2 cm, respectively.18 Additionally, measuring of the caudal angulation of the levator muscle may serve as an indicator of the pelvic floor laxity.16 Organ prolapse is graded as small (grade 1, 0-2 cm below H-line, moderate (grade 2, 2-4 cm), and large (grade 2, >4 cm).2 The anorectal junction is the point where the distal part of rectum meets the anal canal. Anorectal angle (ARA) (Figure 4) is defined as the angle between the two lines, one at the posterior wall of the distal part of the rectum and the other representing the central axis of the anal canal.1
Imaging findings
Pathologic conditions are described topographically as discussed below.
Anterior compartment
Cystocele and urethral hypermobility
Cystocele is defined as the urinary bladder descent during straining 1 cm below the PCL.2, 16, 19 The entity results from a tear in the pubocervical fascia that may be located in the central part of the fascia, in the lateral part (paravaginal) or a combination of both.2, 17 Intact endopelvic fascia is seen on axial images as a straight line of the posterior bladder wall (Figure 2). In most cases, women present with some degree of stress urinary incontinence. It is related to urethral sphincter deficiency which occurs due to diminished support from the anterior vaginal wall.2, 13 The distal two-thirds of the urethra and the anterior vaginal wall are inseparable. Because the proximal urethra and the bladder neck are mobile in a large cystocele, the posterior wall of the urinary bladder may descend more than the anterior wall, causing the downward and clockwise urinary bladder rotation and the rotation of the urethral axis into a horizontal position, which can be seen on sagittal images. When the urethral axis rotates over 30° it is defined as urethral hypermobility. Other MR findings associated with it are partial defects or complete distortion of the urethral ligaments and an abnormal vaginal configuration (the normal H-shape) which is best seen in the axial plane (Figure 5).17, 20 If the urinary bladder prolapse is severe, the ureters may become entrapped in the muscles of the pelvic floor, resulting in hydronephrosis.21 Treatment ranges from nonsurgical interventions, such as pessary in mild cases of cystocele, to surgical procedures (eg, retropubic urethropexy) in more severe cases to restore the original organ position.1,16
Urethral funneling (beaking) is a condition where dilatation of the proximal urethral lumen and apparent shortening of the urethra occurs (Figure 6). It can indicate loss of intrinsic urethral sphincter integrity in an incontinent women. It can be observed even in continent women and is therefore considered to be a nonspecific sign.1, 17 On midsagittal images, separately assessing the urethra and the urinary bladder is important, as high-grade cystocele may mask urethral hypermobility.2 Urethral hypermobility requires a pubovaginal sling procedure to provide midurethral support and avoid subsequent stress incontinence.1, 2, 16
Middle compartment
Uterine and vaginal vault prolapse
Vaginal or cervical prolapse is diagnosed as the vaginal vault descends below the PCL line.1It results from the laxity of the uterosacral ligaments and muscle damage that allow the cervix to move anteriorly, resulting in progressive uterine retroversion and subsequent prolapse. On axial images, the vagina loses the typical H shape and is displaced inferiorly, and on dynamic images, the distal portion moves anteriorly. On coronal images, the iliococcygeus muscle appears flat or convex downward.2
Vaginal prolapse in patients who have undergone hysterectomy is termed “apical prolapse.” It is due to a defect in the superior vaginal support (pubocervical and rectovaginal part of the endopelvic fascia). In these women, support of the vaginal vault is provided by paracolpium.13 Mild vaginal vault prolapses can be managed with pelvic floor exercise. In more severe cases, reattachment of the vaginal vault to the sacrospinous ligament, ileococcygeus muscle or uterosacral ligaments is needed and the procedure is called uterosacral suspension.2, 16 Uterine prolapse is usually treated with hysterectomy.2
Posterior compartment
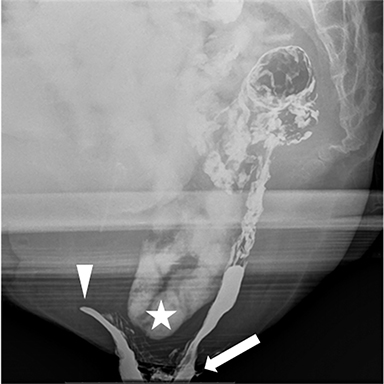
Enterocele, peritoneocele and sigmoidocele
Small-bowel and peritoneal mesenteric structures can herniate downward along the ventral rectal wall, passing more than one-third of the vagina into the rectovaginal space (cul-de-sac) or posterior perineum.1, 2 Depending on the content (small intestine, omental fat or sigmoid colon) it is called an enterocele, peritoneocele or sigmoidocele. Enterocele may be simple or complex, depending on presence of vaginal vault prolapse, which is important for surgical planning.2 When enterocele occurs at the end of defecation, it may result in incomplete evacuation due to outlet obstruction, which is manifest by repetitive and unproductive straining.3 Patients who have undergone hysterectomy are particularly prone to vaginal prolapse. Vaginal descent creates a wide rectovaginal space, predisposing patients to enterocele and peritoneocele.1 A large cystocele may mask coexisting enterocele or rectocele because of tight space in the pelvic floor.13
Surgical repair aims to obliterate the cul-de-sac and is called a culdoplasty.1 Another operation, the sacrocolpopexy, lifts the vagina to its normal position and attaches it by a mesh to the sacrum.19
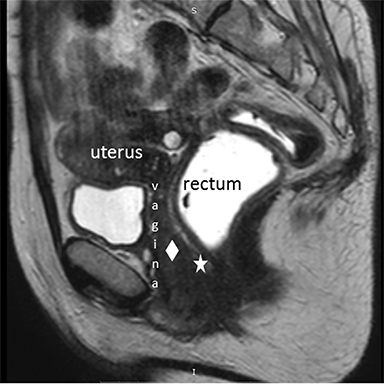
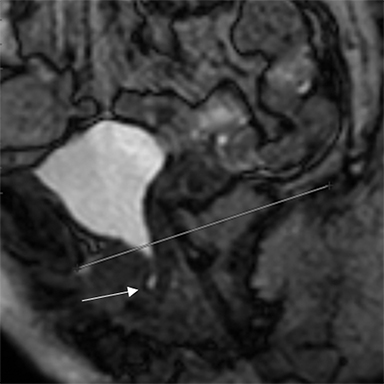
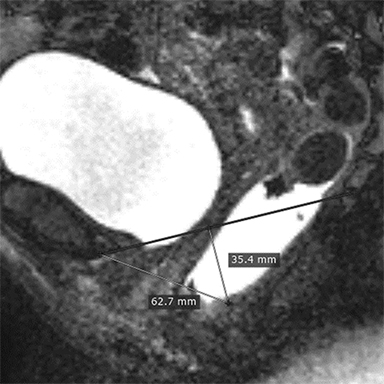
Rectocele
Anterior rectocele is the most common pathology in the posterior compartment and is considered when the rectal wall protrudes or bulges beyond the expected margin of the anterior rectal wall into the posterior vaginal wall. It is graded as small (when measuring <2 cm), moderate (measuring 2 - 4 cm), and large (measuring >4 cm). Small rectoceles are common findings in asymptomatic women. Rectocele becomes clinically relevant when there is retention of contrast medium after defecation that correlates with a feeling of incomplete evacuation.1 Less frequently there is bulging of the posterior or lateral rectal wall. It results from the defects in the prerectal and pararectal fascia (endopelvic) or rectovaginal septum. Anterior rectocele can easily be identified on the midsagittal image. Moreover, rectoceles are classified based on the complete or incomplete evacuation of the contrast media at the end of defecation (Figure 7).19 Surgical treatment involves rectovaginal fascia repair or posterior fixation of the rectum with possible sigmoid or rectal resection.2
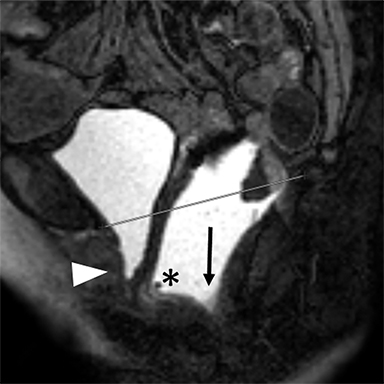
Intussusception
Rectal intussusception is the invagination of the rectal mucosa into the rectal lumen. It may remain internal (in which case it is classified intrarectal), may extend into the anal canal (intra-anal) or pass the anal sphincter (extra-anal or extrarectal) which is most often called rectal prolapse. Low-grade intussusception is defined when rectal mucosa infolding is seen, but not extending intra-anal. High-grade intussusception or prolapse is full-thickness rectal wall prolapse that penetrates the anal canal.1, 12 Rectal intussusception and rectal prolapse often coexist.19 Simple intussusception may be treated with transanal excision of the prolapsing mucosa, while full-thickness rectal invagination requires rectopexy alone or in combination with colporrhaphy or levatoplasty.1,19
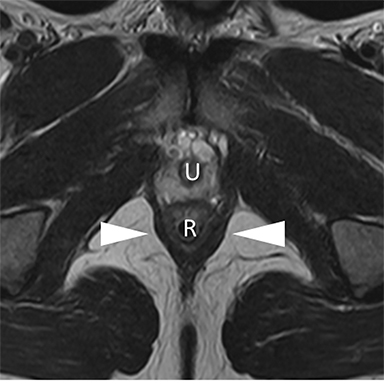
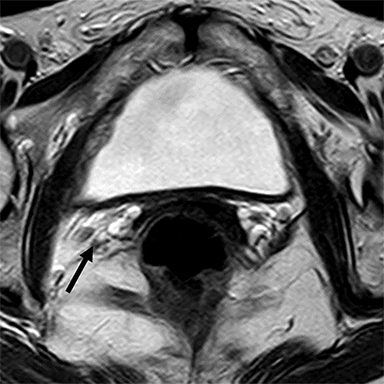
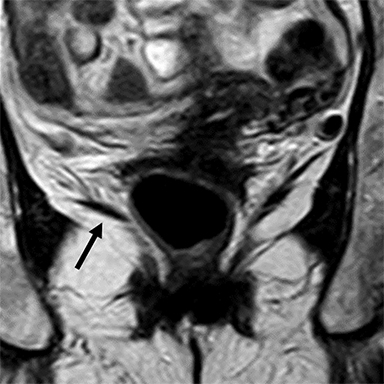
Pelvic floor descent
Pelvic floor descent or descending perineal syndrome occurs when pelvic muscles lose tone, resulting in excessive descent of the entire pelvis floor at rest or during evacuation. On dynamic imaging, pelvic floor descent is defined as anorectal junction descent of more than 2.5 cm below the PCL. Patients suffer from symptoms of outlet obstruction, associated with pelvic pain and feeling of incomplete evacuation. Focal asymmetry of the levator ani muscle may also occur and is best imaged in the coronal plane (Figure 8).1
Spastic pelvic floor syndrome
Spastic pelvic floor syndrome is observed in some constipated patients. During progressive straining no physiological relaxation of the puborectal muscle occurs. Instead, inappropriate and paradoxical contraction of the pelvic floor muscles is observed.14 There is a long time interval between opening of the anal canal and start of defecation; therefore, the evacuation is prolonged and sometimes incomplete.1
Anal incontinence
Muscles that maintain continence are the internal and external anal sphincters and puborectal muscles.4 MR signs of anal incontinence are inability to hold an enema, anorectal decrease by 10°, pelvic floor descent in addition to possible coexistence of intussusception or rectocele. Patients in whom sphincter tear or atrophy is detected are candidates for surgical repair.1
Postoperative imaging
Postoperative imaging can be done for follow up and in cases of symptom recurrence. In recurrence, knowing which surgery has been performed is important for easier evaluation of the postsurgical anatomy and to plan a successive procedure (Figure 9).16
Conclusion
Pelvic floor dysfunction syndrome is a common clinical problem. Dynamic MRI of the pelvic floor is mandatory in patients in whom conservative management is unsuccessful to determine the extent of the pathology and for choosing an appropriate surgical procedure. It is also a comfortable diagnostic method for patients. Recent study by Schreyer et al showed that pelvic organs in healthy volunteers are highly mobile and suggested that normal values should be reassessed on a large group of healthy subjects.11
References
- Colaiacomo MC, Masselli G, Polettini E, et al. Dynamic MR imaging of the pelvic floor: A pictorial review. Radiographics. 2009;29(3):e35.
- Boyadzhyan L, Raman SS, Raz S. Role of static and dynamic MR imaging in surgical pelvic floor dysfunction. Radiographics. 2008;28(4):949-967.
- Piloni V, Tosi P, Vernelli M. MR-defecography in obstructed defecation syndrome (ODS): Technique, diagnostic criteria and grading. Tech Coloproctol. 2013;17(5):501-510.
- Maglinte DD, Hale DS, Sandrasegaran K. Comparison between dynamic cystocolpoproctography and dynamic pelvic floor MRI: Pros and cons: Which is the „functional“ examination for anorectal and pelvic floor dysfunction? Abdom Imaging. 2013;38(5):952-973.
- Miedel A, Tegerstedt G, Maehle-Schmidt M, et al. Symptoms and pelvic support defects in specific compartments. Obstet Gynecol. 2008;112(4):851-858.
- Broekhuis SR, Futterer JJ, Hendriks JC, et al. Symptoms of pelvic floor dysfunction are poorly correlated with findings on clinical examination and dynamic MR imaging of the pelvic floor. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20(10):1169-1174.
- Garcia del Salto L, de Miguel Criado J, Aguilera del Hoyo LF, et al. MR imaging-based assessment of the female pelvic floor. Radiographics. 2014;34(5):1417-1439.
- Abrams P, Andersson KE, Birder L, et al. Fourth international consultation on incontinence recommendations of the international scientific committee: Evaluation and treatment of urinary incontinence, pelvic organ prolapse, and fecal incontinence. Neurourol Urodyn. 2010;29(1):213-240.
- Bump RC, Mattiasson A, Bo K, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996;175(1):10-17.
- van der Weiden RM, Rociu E, Mannaerts GH, et al. Dynamic magnetic resonance imaging before and 6 months after laparoscopic sacrocolpopexy. Int Urogynecol J. 2014;25(4):507-515.
- Schreyer AG, Paetzel C, Furst A, et al. Dynamic magnetic resonance defecography in 10 asymptomatic volunteers. World J Gastroenterol. 2012;18(46):6836-6842.
- Bertschinger KM, Hetzer FH, Roos JE, et al. Dynamic MR imaging of the pelvic floor performed with patient sitting in an open-magnet unit versus with patient supine in a closed-magnet unit. Radiology. 2002;223(2):501-508.
- Law YM, Fielding JR. MRI of pelvic floor dysfunction: Review. AJR Am J Roentgenol. 2008;191(6 Suppl):S45-53.
- Roos JE, Weishaupt D, Wildermuth S, et al. Experience of 4 years with open MR defecography: Pictorial review of anorectal anatomy and disease. Radiographics. 2002;22(4):817-832.
- Yang A, Mostwin JL, Rosenshein NB, et al. Pelvic floor descent in women: Dynamic evaluation with fast MR imaging and cinematic display. Radiology. 1991;179(1):25-33.
- Fielding JR. Practical MR imaging of female pelvic floor weakness. Radiographics. 2002;22(2):295-304.
- Macura KJ, Genadry RR. Female urinary incontinence: Pathophysiology, methods of evaluation and role of MR imaging. Abdom Imaging. 2008;33(3):371-380.
- Comiter CV, Vasavada SP, Barbaric ZL, et al. Grading pelvic prolapse and pelvic floor relaxation using dynamic magnetic resonance imaging. Urology. 1999;54(3):454-457.
- Hausammann R, Steffen T, Weishaupt D, et al. Rectocele and intussusception: Is there any coherence in symptoms or additional pelvic floor disorders? Tech Coloproctol. 2009;13(1):17-25; discussion 25-6.
- Macura KJ, Genadry RR, Bluemke DA. MR imaging of the female urethra and supporting ligaments in assessment of urinary incontinence: Spectrum of abnormalities. Radiographics. 2006;26(4):1135-1149.
- Pannu HK, Kaufman HS, Cundiff GW, et al. Dynamic MR imaging of pelvic organ prolapse: Spectrum of abnormalities. Radiographics. 2000;20(6):1567-1582.
Citation
MV T, M P.Dynamic MR imaging of pelvic floor dysfunction. Appl Radiol. 2017; (8):21-27.
August 1, 2017