Dose reduction in cardiac CTA:The cardiologist's perspective
Images
Dr. Defrance is a Clinical Associate Professor, Stanford Medical School, Stanford, CA, and National Director of CT Workgroups for the SCCT.
I am an interventional cardiologist and I work on both a 64-detector row and a 320-detector row computed tomography (CT) scanner. In the last 25 years, medical radiation exposure has been increasing and CT accounts for the bulk of that increase.So we want to minimize the patient risk from cardiac CT, while obtaining diagnostic-quality images. We have tools like dose modulation and EKG modulation and prospective gating. We can modulate the mA and the kV to suit individual patients. We can limit Z-axis exposure. We can gate and ungate images in a single scan, on some of the vendors’ machines and we also have wide-area detectors.
Measuring dose in cardiac CTA
Are we using these tools? Two studies can help address this issue. First, the Protection I trial, which was a cross-sectional, multivendor, multinational observational study, looking at radiation doses in 50 sites.1The main outcome they were looking at was dose length product (DLP). So, in these 50 sites, over a period of time, they found the mean DLP was 833. Presenting effective dose in mSv they found that there was a massive variation (up to 6 fold) in dose.
Protection I identified how several independent variables were associated with radiation exposure. First, in patients with higher body weight they received about 5% more radiation. If the patient had no sinus rhythm they tended to get a 10% higher dose. Lower scan lengths contributed to dose reductions, particularly the more we minimize our Z axis the less dose we deliver. Every 10 mm of scan length added about 5% of the dose. Lowering kV whenever possible, especially for patients with lower body weight yielded a 46% dose reduction, but only 5% of sites did that. Using prospective instead of retrospective gating led to a massive dose savings of close to 80%. So we see that the prospective imaging technique becomes very important. EKG-gated dose modulation led to a 25% dose reduction and this was used in about 70% of the centers.
Michigan BCBS registry
Switching gears, Raff et al. conducted a Blue Cross-Blue Shield registry in Michigan, and they tracked CT utilization and certainquality metrics. They found alarmingly high average doses in a number of centers enrolled in the registry. Some centers were giving average doses of 35 mSv. The median dose, across all the centers they tracked was 25 mSv. They immediately instituted an education and quality-assurance program, and provided counseling, comparative reporting and scanner-specific training. They re-evaluated sites 9 months later and the median dose was down to 13 mSv. In personal communication, Dr. Raff told me 6 to 12 months later, the doses drifted back up. So, without continual reinforcement, he said they were back up to about 19 mSv to 20 mSv.
64-detector row experience
We started out on a 64-detector row CT, and we primarily performed retrospective gating. We did not have the tools to do prospective gating. We used dose-modulation in 65% of our patients and our average dose was about 16.1 mSv. We then began using calcium scoring to limit the field of view and we reduced our dose to about 14 mSv. By cutting off about 2 cm to 3 cm of irradiated tissue we saw our radiation doses drop accordingly.
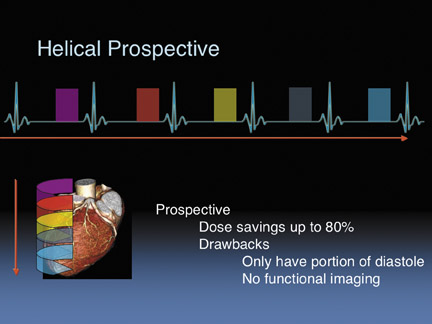
Then we obtained helical prospective gating. Dr. Fleischman talked about step-and-shoot prospective gating. On our particular scanner, we use a helical prospective gating that takes images during each of the cardiac cycles. We can vary the padding or the width of how long you turn on the beam during the cardiac cycle (Figure 1). We found that if we keep a narrow window in which we turn the beam on, we could save up to 80% of the dose. The drawbacks to this method are that we only obtain a small portion of the diastolic phase. We have to make sure that we maintain good control of the patient’s heart rate, and we had to ensure that our physicians could tolerate just a small percentage of the cardiac cycle.
We now do 85% of our patients prospectively. This has dramatically changed our cardiac CT imaging practice. We use the calcium score to limit the field of view. And we use 100 kV on patients less than 80 kg. Our average dose has dropped from 16 mSv to 14 mSv and now to 7 mSv. We do a small percentage of patients with retrospective gating.
We recently submitted an abstract to the Society for Cardiovascular Computed Tomography about a weight-adjusted protocol. In it, we used a body-weight adjustment for kV. We scored the image quality on a 1 to 4 scale. Scan parameters were:
- 00 – 135 kV (85% done with 120 kV)
- 350 – 500 mA (Average 401 mA)
- 0.35 sec gantry rotation
- Gating window 70% – 85% of RR interval
- Effective dose estimates, and calculated DLP x 0.017
We examined 27 patients who were successfully imaged with this new technique and the average quality score was 3.88 out of 4 with excellent image quality in 91% of studies. Less than 1% of segments were noninterpretable (0.4%) and the average dose was 6.9 ±4.0mSv.
Part of the success of this technique is because we lowered the heart rates below 60 BPM on almost all the patients. So we saw almost no noninterpretable segments.
320-detector row experience
We have imaged more than 1000 patients on our 320-detector row CT scanner. We have used prospective imaging in 70% of patients and we have used retrospective gating with dose modulation in 20%. We have performed full retrospective gating in about 10% of patients. We do not usually use the entire 16 cm detector and we usually opt to cone down to 14 cm or 12 cm. We reduce the kVp for patients weighing <80 kg.
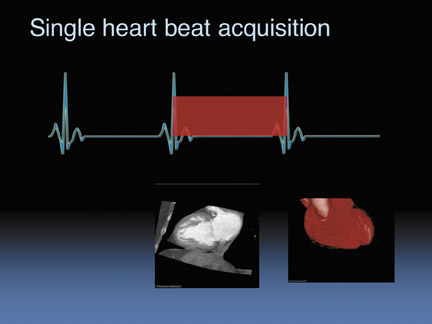
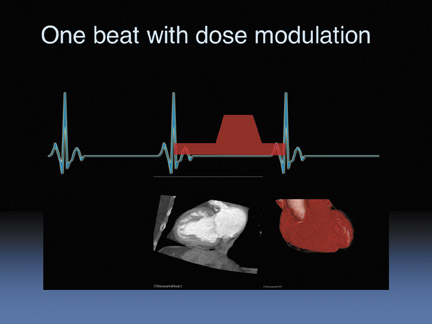
So for the 320-detector row scanner, we can image 14 cm in one heartbeat without dose modulation. And then we can obtain functional images as well. When we modulate the dose (Figure 3) we ramp the beam down during systole and ramp it up during diastole, again, this is acquired in only one heartbeat.
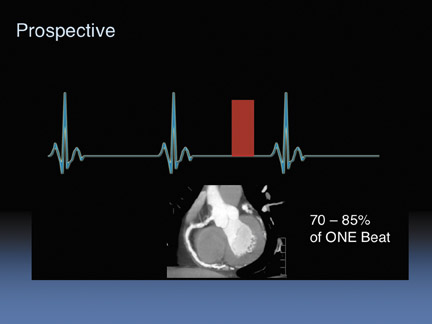
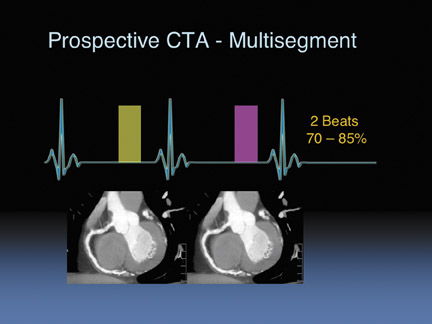
We can also do prospective gating (Figure 4), and we do this in about 70% of patients. We just turn the tube on and off, briefly. We turn the beam on between 70% to 80% of the cardiac cycle. For patients with higher heart rates we can prospectively image during two cardiac cycles (Figure 5) and do segmental averaging. This will obviously increase the dose because you have imaged twice but it does help for higher heart rate patients.
In our experience, our prospective average dose is around 4 mSv.The lowest dose we’ve seen is <2 mSv in an adult heart with 100 kVand 12 cm coverage. We deliver an average dose of around 5 mSv.
We submitted an abstract to RSNA where we imaged 15 consecutive patients with our prospective protocol. We used 14 cm coverage for 12 of 15 patients, and we used 12 cm coverage for smaller patients. Our gating window was turned on 65% through to 85% of the RR interval. We assessed image quality. And we showed DLP and reported effective dose. Everyone was successfully imaged, with very high image quality. There were no noninterpretable segments. The average radiation dose was about 4 mSv.
The most important key to our success has been patient preparation. We give beta blockers to all of our patients, unless they have a severe contraindication. We give 2 oral doses: one the night before and another 90 minutes before the study. We will deliver additional IV beta blockade, as necessary, to get the heart rate below 60 BPM. So our patients are optimally prepped, and that is what gives us the confidence to just turn on the tube for very brief periods of the cardiac cycle. This preparation allows reliable prospective imaging, with minimal padding. I cannot emphasize enough that beta blockers are the key to our ability to do this.
CT limitations
So how can we compare CT to other modalities? I agree that we cannot compare CT dose to the dose from a number of chest X-rays. The modality should be compared to an invasive angiogram, a stress nuclear study, or any other test you would order to diagnose coronary disease.
Equipment limitations have been a problem in some cases. The vendors have done a very good job innovating the technology, but some of the machines being used clinically are several years old, and some of them do not have the latest software or hardware in order to do prospective imaging.
Additionally many imagers are simply unaware of the dose they are delivering. They do not look at it regularly, and have no idea about the implications. In the Raff study, people had no idea they were delivering 35 mSv, in some cases. There is also inadequate education for the physicians who are being trained to read cardiac CT. Further, clinical routines are hard to change. People get in a pattern, and it can be very difficult to get them to alter their routines. And then many of the patients are not adequately prepped. They may show up with a heart rate of 70 BPM. So the decision in many imaging centers is not to spend 20 to 30 minutes beta blocking the patient and instead they elect to do retrospective gating.
Addressing the challenges
We need simplified standards and clear recommendations for the clinicians ordering CT. The SCCT is drafting a set of guidelines to address this need. We need to get knowledge of tools like prospective imaging into everyone’s hands, especially when it is possible to do prospective gating on older scanners. Vendors need to address the issue by making prospective techniques affordable.
In terms of awareness, we can do a better job with training programs, seminars and conferences. Apart from meeting in person or virtually over the Internet, we can publish newsletters and more articles to make people aware of these beneficial techniques.
We also need to do a better job emphasizing the risk-to-benefit ratio and appropriateness criteria for referring clinicians. Additionally, it would help to standardize and simplify how we record dose.
Ultimately it comes down to a difficult question: How do you get people to change their behavior? One step is encouraging a proper clinical routine. This is never an easy task but it simplifies with repetition. Clearly, radiation dose reduction is the buzz right now and it falls to the thought leaders and professional organizations to reinforce these concepts. We can also get our technologists involved and trained in how to use the most dose-optimized techniques. We should also require dose tracking and we could ultimately link facility accreditation to dose reduction methods. Finally, we should push for standards that are reproducible and understandable.
Conclusion
So I think, in terms of using the tools, we have to get patients beta blocked, get good protocols in place, and train the referring doctors about why it is necessary to appropriately order these scans. We need to develop clear, concise protocols for PO and IV beta blockade. When we perform our cardiac CTAs, our average patient heart rate is 56 BPM; we achieve this because we are aggressive about beta blocking.
There are excellent tools available to provide high-quality cardiac CT imaging at low doses, but the tools are not being used consistently. Organizing a campaign is essential in educating and informing physicians and technologists.
REFERENCES
- Hausleiter J, Meyer T, Hermann F, et al. Estimated radiation dose associated with cardiac CT angiography. JAMA. 2009;301:500-507.
- Raff G, Chinnaiyan K, Abidov A. Abstract 4717: Marked radiation dose reduction in a statewide coronary CT quality improvement registry.Circulation. 2008;118:S936