Congenital Zika Virus Infection and Chorioretinal Coloboma
Affiliations
- 1 Ponce Health Sciences University School of Medicine, Ponce, Puerto Rico
- 2 Edward B. Singleton Department of Radiology, Texas Children’s Hospital and Baylor College of Medicine, Houston, Texas
Case Summary
The patient is a child with clinical presentation and findings consistent with congenital Zika virus (ZKV) infection, who immigrated to the United States at the age of 2 years. The patient has a history of prematurity, seizure disorder, intellectual disability, cerebral palsy, microcephaly, dysphagia, slow transit constipation, and severe malnutrition. The patient presented to our institution due to a significant increase in seizure frequency, progressing from one seizure per day to approximately 6-8 tonic-clonic seizures per day, each lasting about 2.5-3 minutes. The patient has also had myoclonic jerks during the day. Treatment with valproic acid was initiated at the age of 1, and upon arrival in the United States, levetiracetam was subsequently prescribed. Neuroimaging was performed for seizure evaluation. Ophthalmologic consultation was performed because of “misaligned eyes.” The findings on eye examination suggested a left-sided macular coloboma as well as a mild bilateral optic nerve atrophy.
Imaging Findings
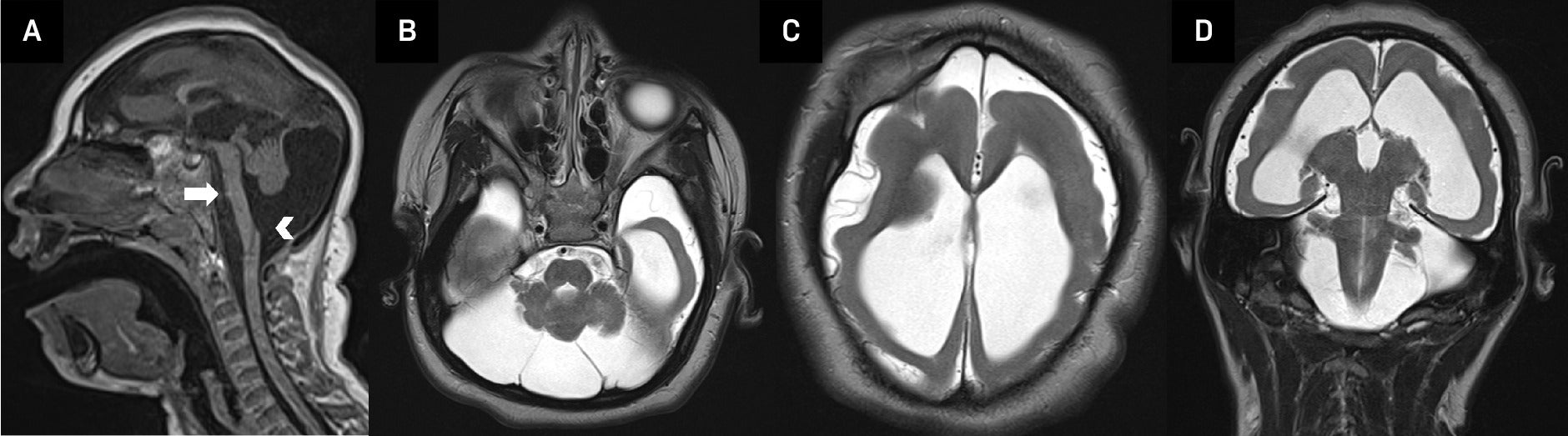
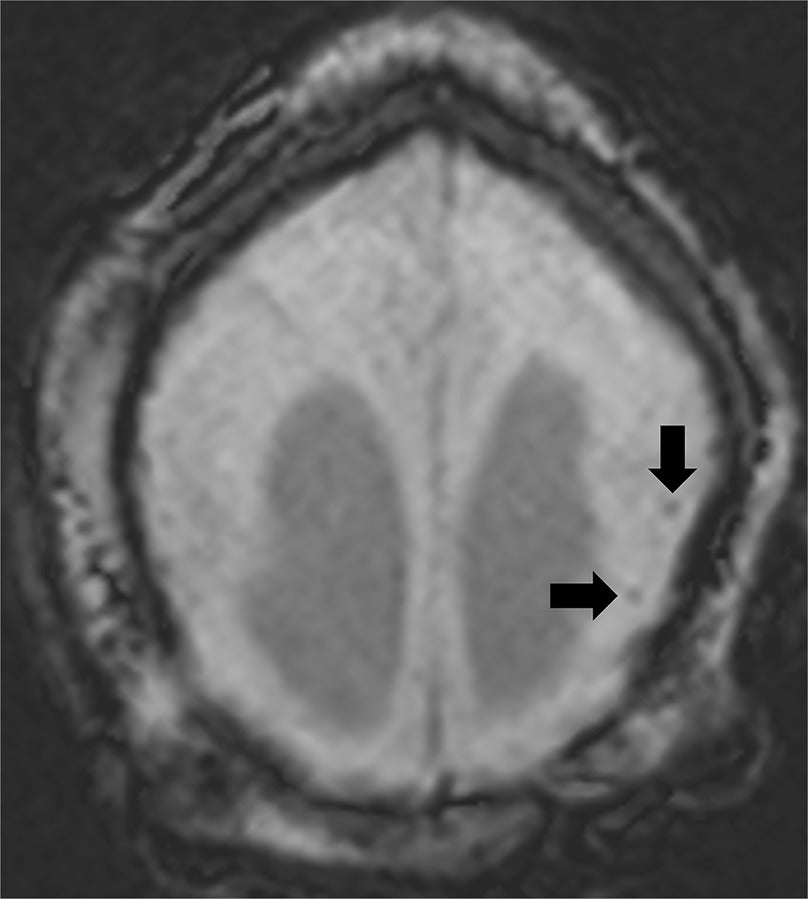
An MRI of the brain ( Figure 1 ) performed at 5 years of age demonstrated severe microcephaly with a markedly diffuse supratentorial simplified gyral pattern. There was incomplete/impaired myelination throughout the parieto-occipital and temporal lobes and subcortical white matter of the frontal lobes bilaterally. Severe global supratentorial white matter volume reduction was seen along with diffuse thinning and apparent foreshortening of the small corpus callosum, predominantly posteriorly. The bilateral lateral and third ventricles were markedly enlarged, while the fourth ventricle was moderately enlarged. The cerebellum appeared diffusely hypoplastic. Furthermore, there was a significantly enlarged mega cisterna magna, which appeared to communicate with the fourth ventricle while rotating and pushing the vermis upward, resulting in a moderately elevated tegmento-vermian angle of 24 degrees. The pons was severely hypoplastic, and the pontine belly is completely missing with an apparent flat ventral pontine surface. In addition, scattered peripheral parenchymal calcifications were seen ( Figure 2 ). Lastly, there was a mid-sized coloboma along the posterolateral left eye globe in the region of the macula measuring approximately 0.6 cm in diameter ( Figure 3 ). Both optic nerves appeared thinned with a maximal cross-sectional diameter of 1.4 mm.
Sagittal T1 brain MRI (A) in a child with congenital ZKV infection shows severe microcephaly, hypoplastic pons (arrow) with a flat ventral surface, and an enlarged mega cisterna magna, which appears to communicate with the fourth ventricle (arrowhead). Axial (B, C) and coronal (D) T2 brain MRI demonstrate a hypoplastic cerebellum, as well as a markedly diffuse simplified gyral pattern with abnormal myelination and ventriculomegaly.
Axial susceptibility weighted imaging brain MRI demonstrating markedly diffuse simplified gyral pattern and scattered peripheral parenchymal calcifications.
Axial T2 brain MRI demonstrating a chorioretinal coloboma (arrow) located in the posterolateral aspect of the left orbit as well as mild bilateral optic nerve atrophy (right optic nerve not shown).

Diagnosis
Congenital ZKV infection.
Discussion
Zika virus is a single-stranded RNA arbovirus of the Flaviviridae family that is generally transmitted by the Aedes aegypti mosquito. In adults, ZKV infection is typically asymptomatic, but when symptoms occur, patients report flu-like symptoms such as fever, headache, conjunctivitis, rash, and joint pain lasting days to weeks.1 - 5 Vertical transmission to a fetus is reported and confirmed to occur when a mother is exposed to ZKV during the pregnancy. Children infected in utero, especially within the first or second trimester, tend to have a much more serious presentation. In early intrauterine infections, more first- and early second-trimester developmental processes, like neuronal migration, neuronal differentiation, sulcation/gyration, and myelination processes, may be impacted, eventually resulting in more severe brain malformations. Manifestations of congenital infection include severe microcephaly, joint contractures, hearing impairments, hypertonia, and ocular findings like chorioretinal atrophy, retinal pigment epithelium mottling, optic nerve hypoplasia or atrophy, iris coloboma, microphthalmia, and lens subluxation.1 - 6 This constellation of abnormal central nervous system (CNS) and optic findings is known as congenital Zika syndrome (CZS).
The difference in presentation between adults and children is likely due to the ZKV’s tropism for undifferentiated neurons over differentiated neurons.1 - 3 Intrauterine infection, especially in early pregnancy, can have devastating effects on the fetus, resulting in an overall decrease in neurons and consequently a number of brain abnormalities.1, 3 Studies have also revealed that cells lining the blood–retinal barrier, retinal endothelium, and retinal pigment epithelium have an increased susceptibility to ZKV-induced cell death.1, 3 As a result, extensive research has been conducted to investigate ocular manifestations (in addition to the CNS findings) in individuals with ZKV infection. These studies have demonstrated that ocular abnormalities, especially macular atrophy, occur so frequently in CZS that they may serve as valuable diagnostic indicators for ZKV infection, even in the absence of microcephaly.1 - 3 Recent efforts have also given clinicians ways to differentiate ZKV from other similarly presenting pathologies like rubella and toxoplasmosis.1 Chorioretinal colobomas however are a much more rare presentation with only a few cases reported in the current literature.1, 3, 5, 6 To understand how chorioretinal colobomas occur in CZS, it is essential to discuss what colobomas are, as well as how and when they form.
Colobomas are focal discontinuities or areas of missing tissue in the eye’s structure.7 They occur when the embryonic choroidal fissure fails to completely close during weeks 5-7 of fetal life.7, 8 They can present anteriorly in the iris or ciliary body, or more rarely, posteriorly in the choroid, retina, or optic nerve.7 Those diagnosed with posterior colobomas tend to be older in age.7, 8 Patients with chorioretinal colobomas have a significantly increased risk for retinal detachment, with an incidence reported as high as 42%.8 Given the emergency of this complication, prompt diagnosis and patient education of red-flag symptoms are key. This is especially important in patients with diseases such as CHARGE (Coloboma, Heart defects, Atresia choanae, Retardation of growth, Genital abnormalities, and Ear abnormalities) syndrome, VATER (Vertebrae, Anus, Trachea, Esophagus, and Renal) syndrome, MPPC (Microcornea, Posterior megalolenticonus, Persistent fetal vasculature, and Chorioretinal coloboma) syndrome, and DiGeorge syndrome where chorioretinal colobomas can occur.7, 8
ZKV’s neurotropism for undifferentiated neurons, in conjunction with our knowledge of posterior coloboma formation and presentation, allows us to form a reasonable hypothesis for why chorioretinal colobomas are so rare in ZKV patients. First, to develop a coloboma, fetal exposure to ZKV must occur early in the first trimester as colobomas typically form within weeks 5-7.7 Second, to find a chorioretinal or optic nerve coloboma, a patient must undergo a thorough ophthalmologic evaluation, likely with neuroimaging included. Given this knowledge, it is crucial for newborns suspected of early intrauterine ZKV infection to be promptly screened for orbit abnormalities via comprehensive ophthalmologic and neuroimaging evaluations. In cases of severe microcephaly, radiologists specifically should place special emphasis on studying the eyes in addition to the brain to prevent these ophthalmologic findings from being missed.
Conclusion
Congenital ZKV syndrome is characterized by a series of CNS and optic findings, with chorioretinal colobomas being one of the more rare ocular presentations. This is likely due to the combination of the timing of coloboma formation and the neurotropism ZKV exhibits. As a result, interdisciplinary care of infants with suspected early intrauterine ZKV infection is essential for minimization of complications like retinal detachment, optimal management, and long-term patient care. Specifically, ophthalmologists and radiologists should ensure appropriate communication and perform careful and thorough evaluations of the orbit in patients suspected of congenital ZKV syndrome.
References
Citation
Tirado OAG, Mertiri L, Huisman TAGM.Congenital Zika Virus Infection and Chorioretinal Coloboma. Appl Radiol. 2025;
doi:10.37549/AR-D-25-0109
November 1, 2025