Blind Spots in Spine Imaging
Images












Spine-imaging volumes are increasing, paralleling the rising number of aging Americans seeking care for back and neck pain.1 The most common reason for nontraumatic outpatient spine imaging remains osteoarthritis, which is more common in older patients.2 In addition, the sustained attention required for level-by-level-analysis of degenerative changes creates a unique environment for extraspinal findings to go undetected by a busy radiologist.
Anecdotally, the potential for diagnostic error is affected by several factors, including the complexity of the diagnostic imaging study, the presence of one or more abnormalities, the expertise of the interpreting physician, the number and type of interruptions, and even the timing of interpretation (early versus late into a work shift). For example, at least one study has shown that errors are more likely to be made in the last two hours of a long shift.3 Multiple studies in radiology have also found that detection errors are more common than interpretive errors.4-6 This is especially relevant to spine imaging, where differential diagnoses for perceived abnormalities tend to be less complex than those for brain imaging. Occasionally, an extraspinal finding may be more serious than the original study indication, making detection even more important. In this article, we provide guide to some common “blind spots” in spinal imaging.
The Importance of Scout Images
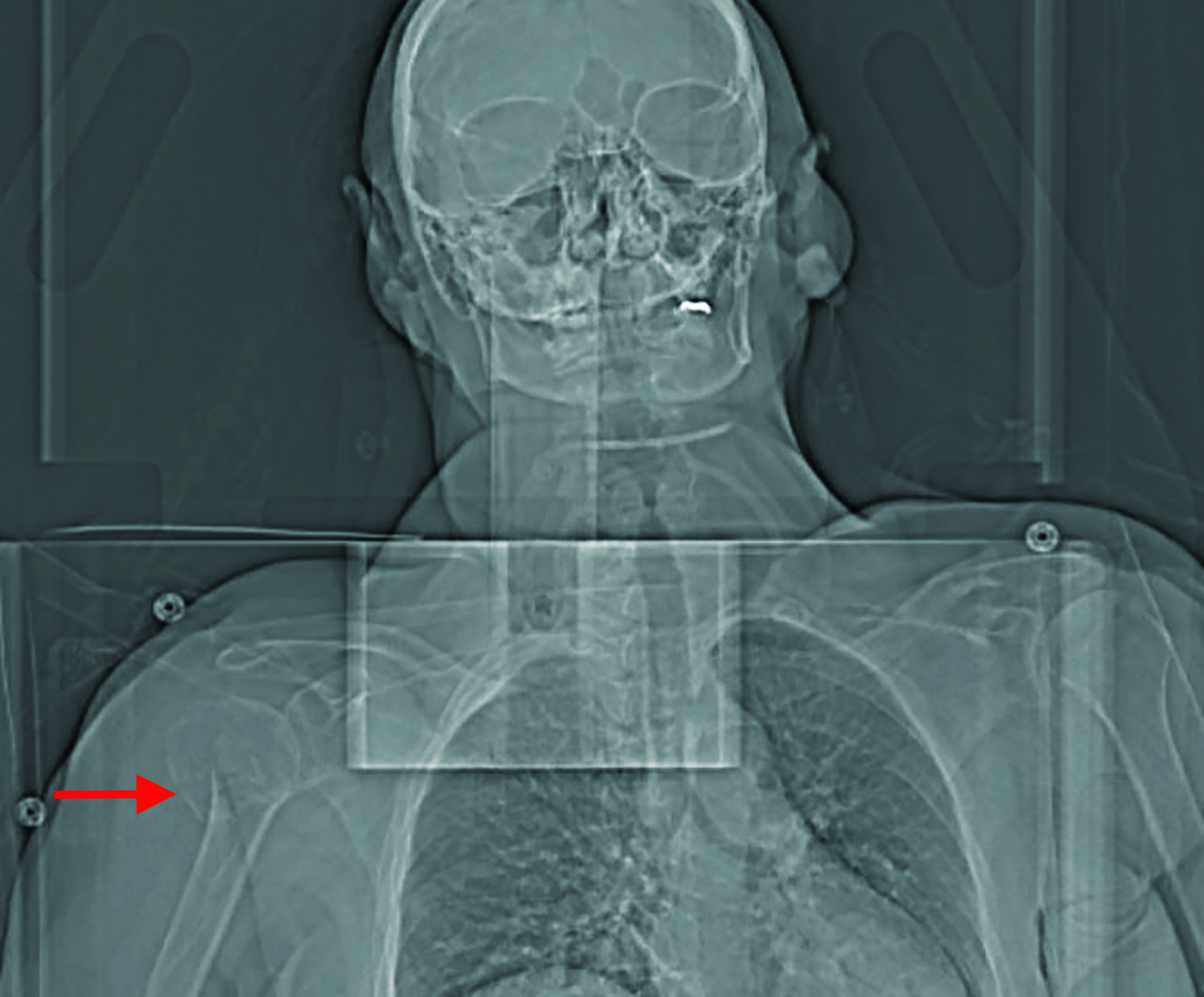
Any interpretation of an imaging study should begin with a careful review of the scout or localizer images, which have been shown to include diagnostic information not included elsewhere in the imaging study.7 Radiologists have been sued for missing information on scout images that went unidentified on the initial interpretation.8,9 Scout images may demonstrate important pathology not included on the cross-sectional computed tomography (CT) or magnetic resonance images (MRI) (Figure 1).
A typical scout tomogram/localizer for a cervical spine exam will often provide at least one view of a portion of the lungs, heart, clavicles, and humeri. Occasionally, lung pathology or mediastinal masses may be visible on the scout tomogram but not present on the cross-sectional CT images. Similarly, a fracture (pathologic or otherwise) or other lesion of the humerus may be visible only on the scout tomogram. The lungs and posterior mediastinum also feature prominently in images of the thoracic spine.
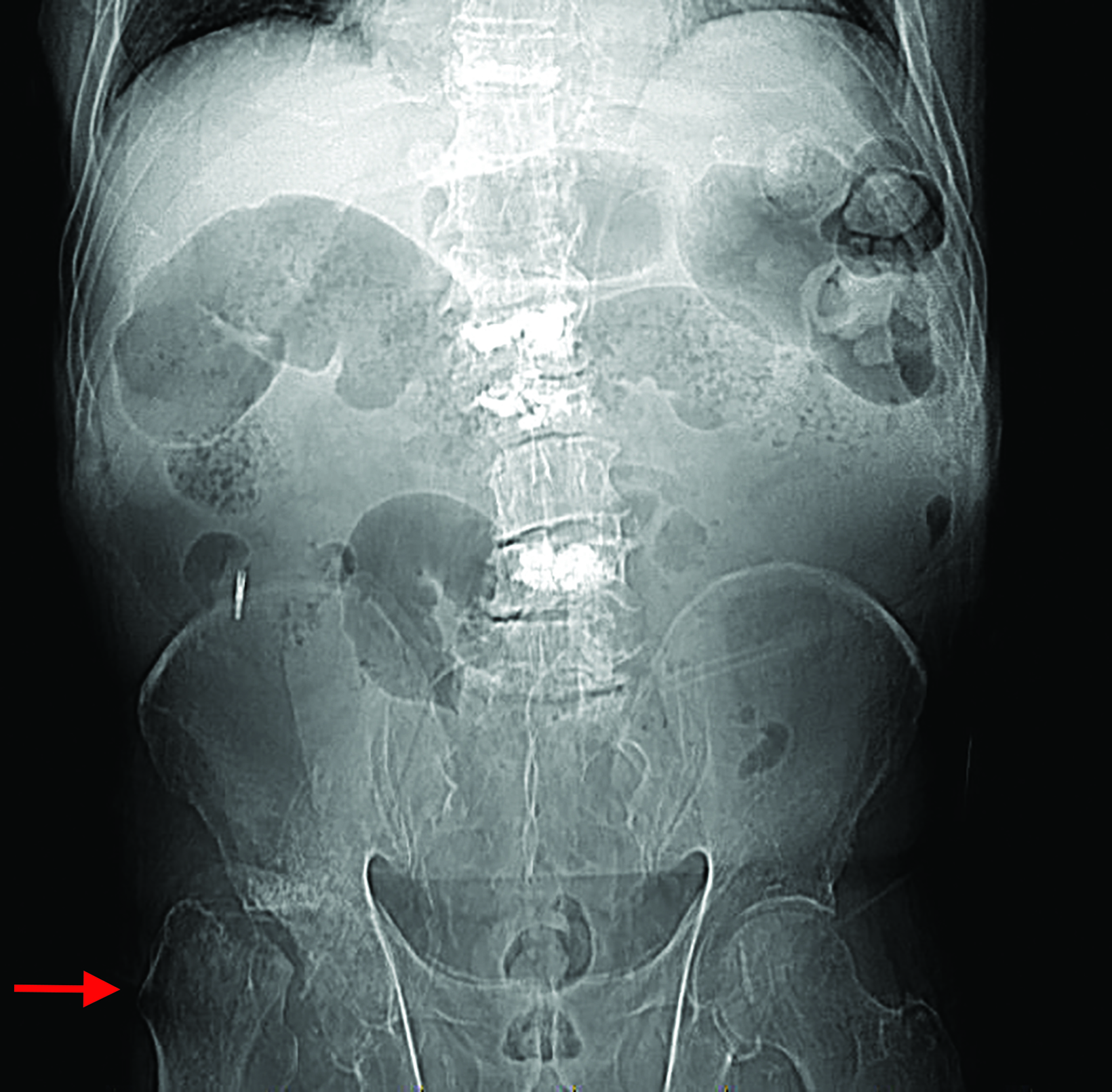
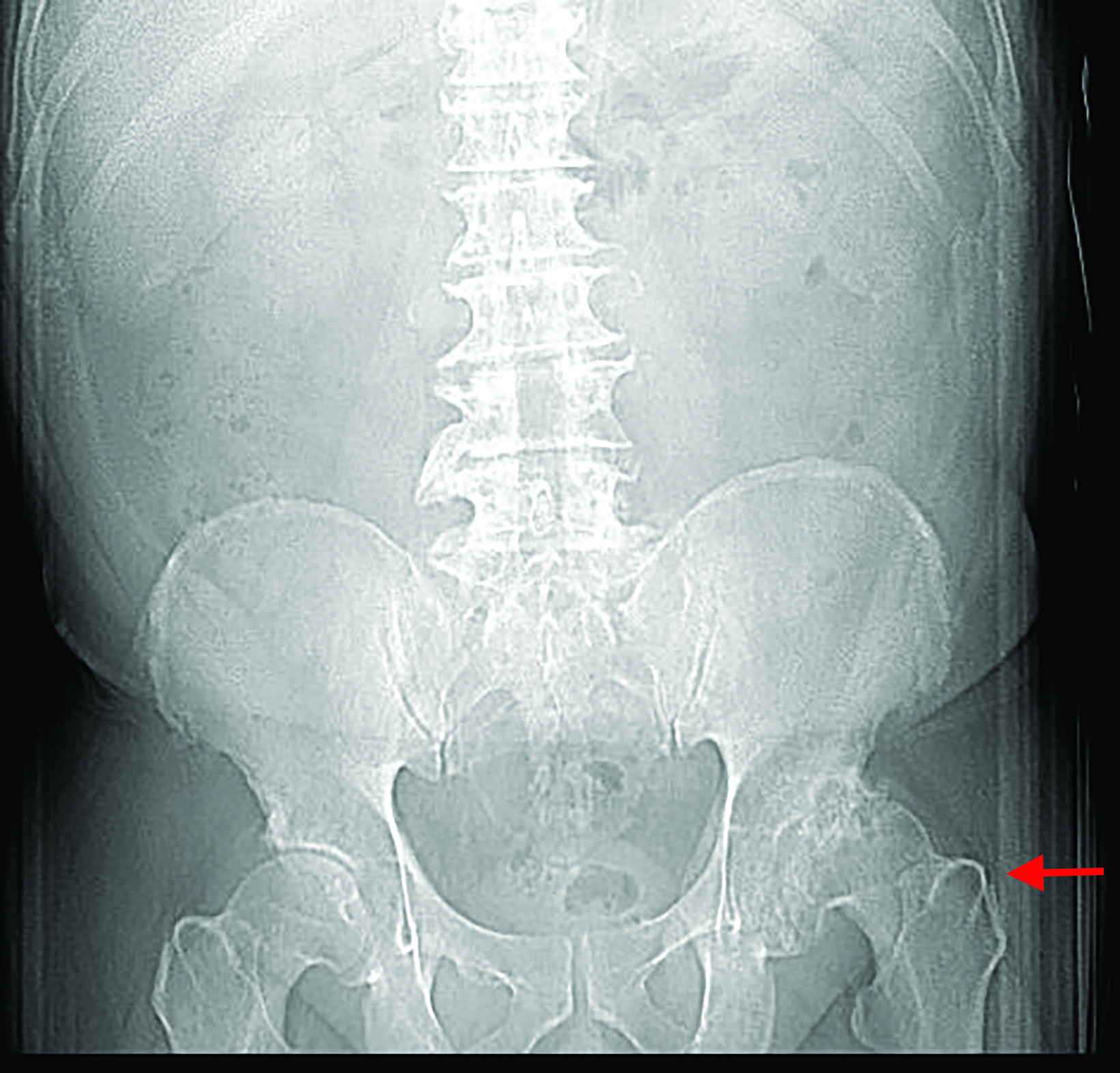
The lumbar spine scout tomogram is particularly challenging because it usually provides an anteroposterior view of both hips. Patients with back pain and spinal degenerative changes also frequently have hip pathology, some of which may be severe (Figure 2). Even a cursory review of the hips on lumbar scout tomograms is occasionally high yield. Incorporating a review of the scout and localizer images into the interpretive process will make detection of such abnormalities more likely.
Vascular Abnormalities
Vascular abnormalities can be a significant source of morbidity and mortality; some can be mitigated or even prevented by early detection and treatment. One of the most common serious abnormalities on a cervical spine study is dissection of the vertebral artery. It is not uncommon for patients with a vertebral artery dissection to present with neck pain, a frequent complaint in patients with musculoskeletal disorders of the neck. The dissection may be pre-existing and exacerbated by chiropractic manipulation,10 or it potentially may be the inciting event in patients with vascular fragility syndromes such as fibromuscular dysplasia.
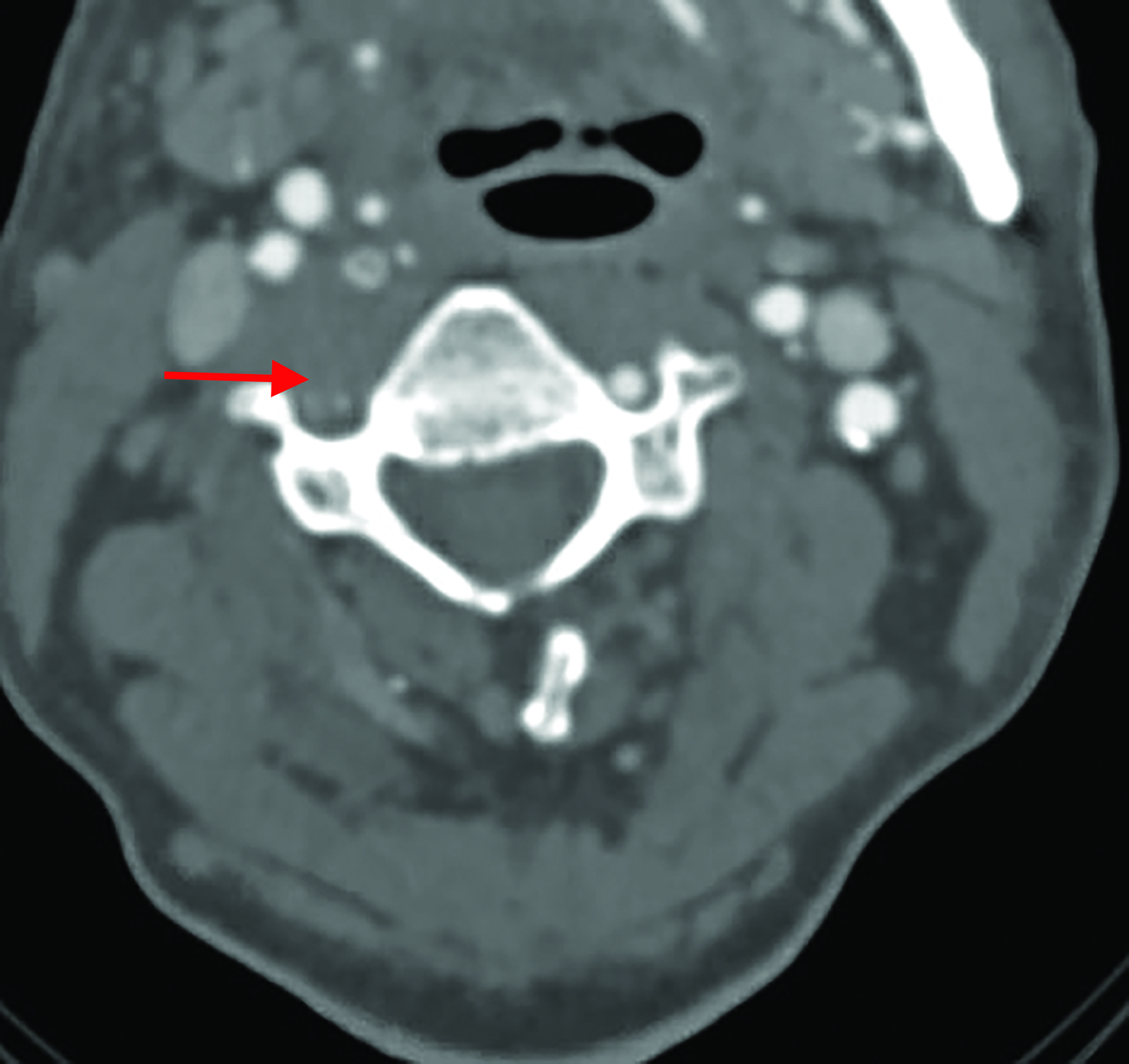
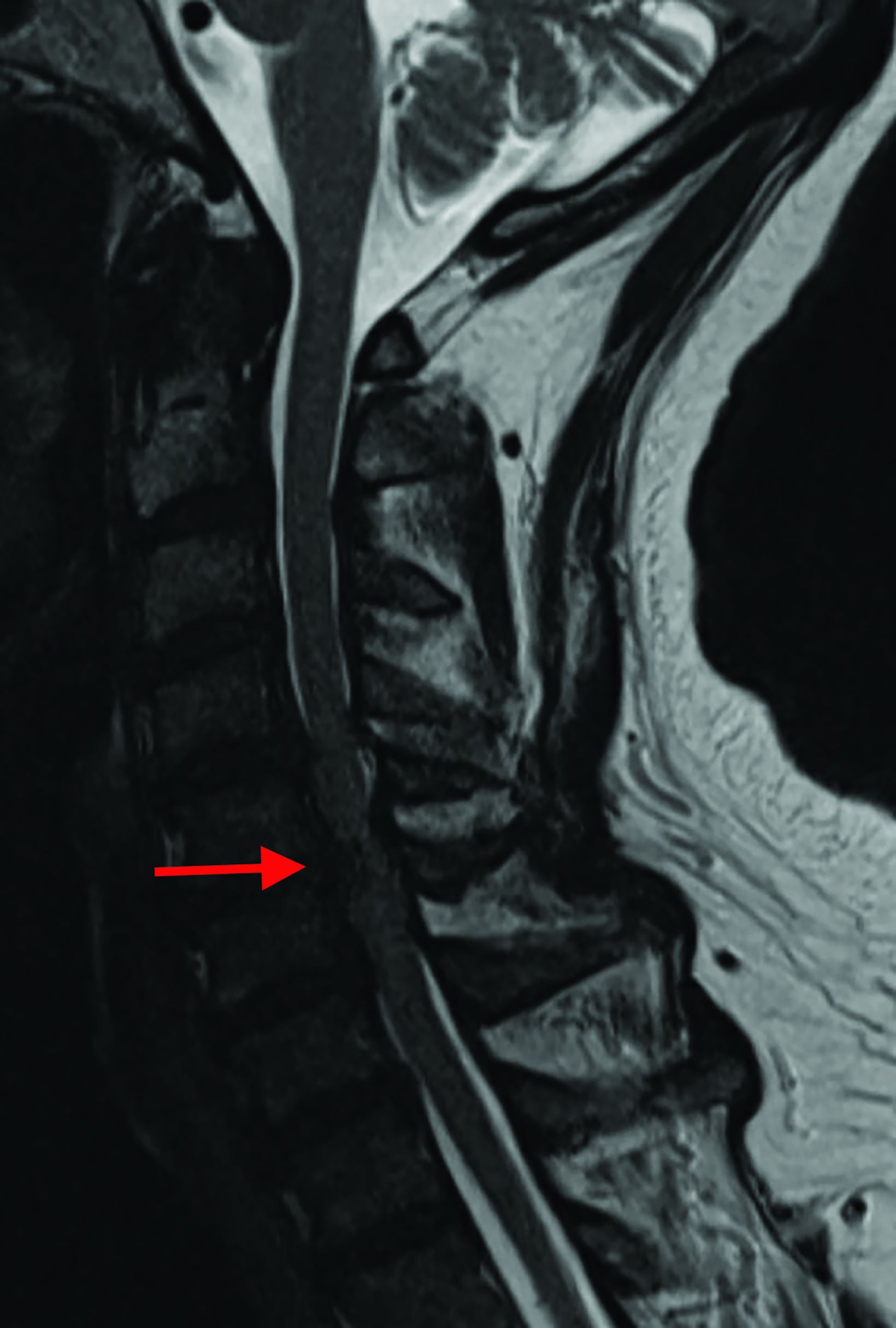
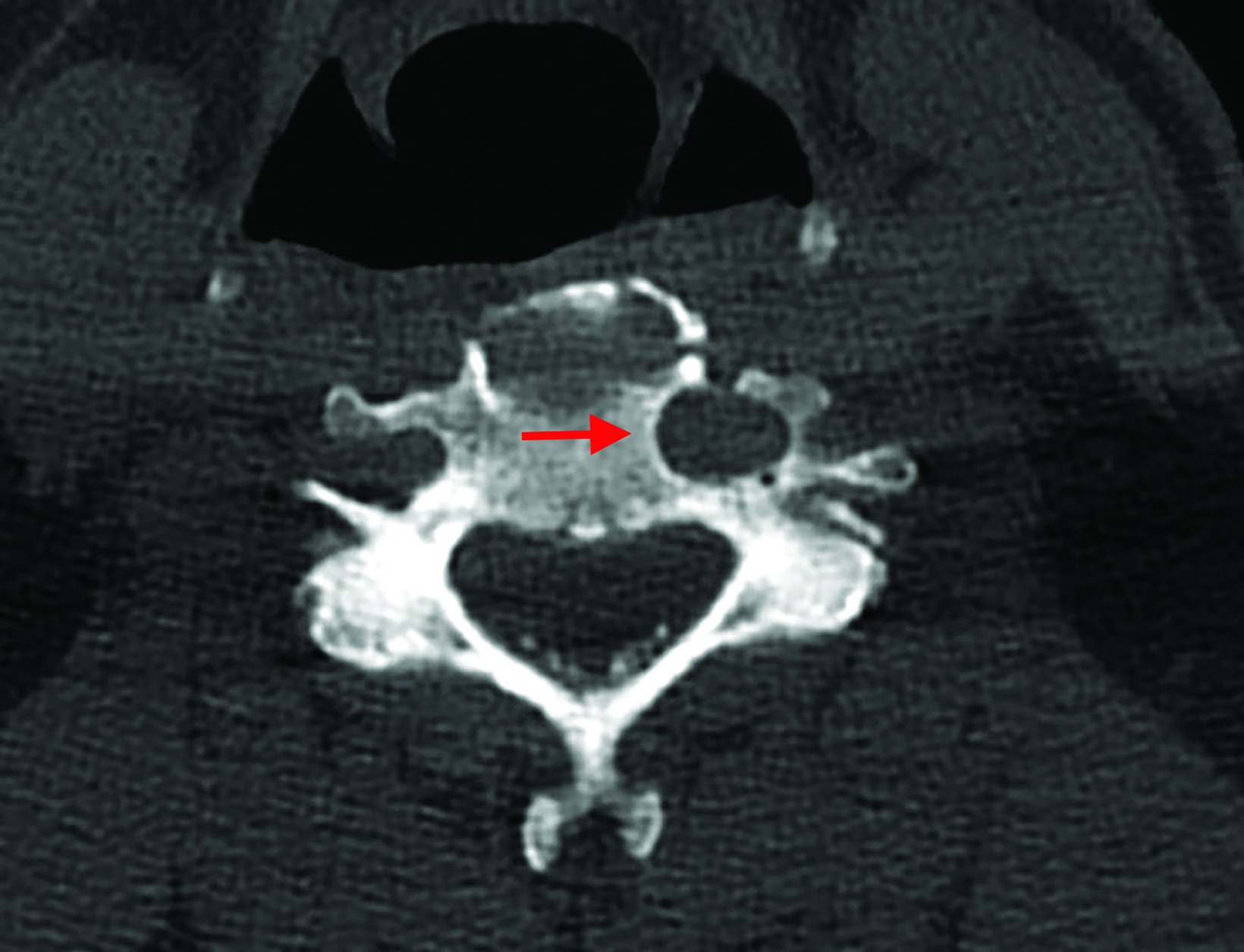
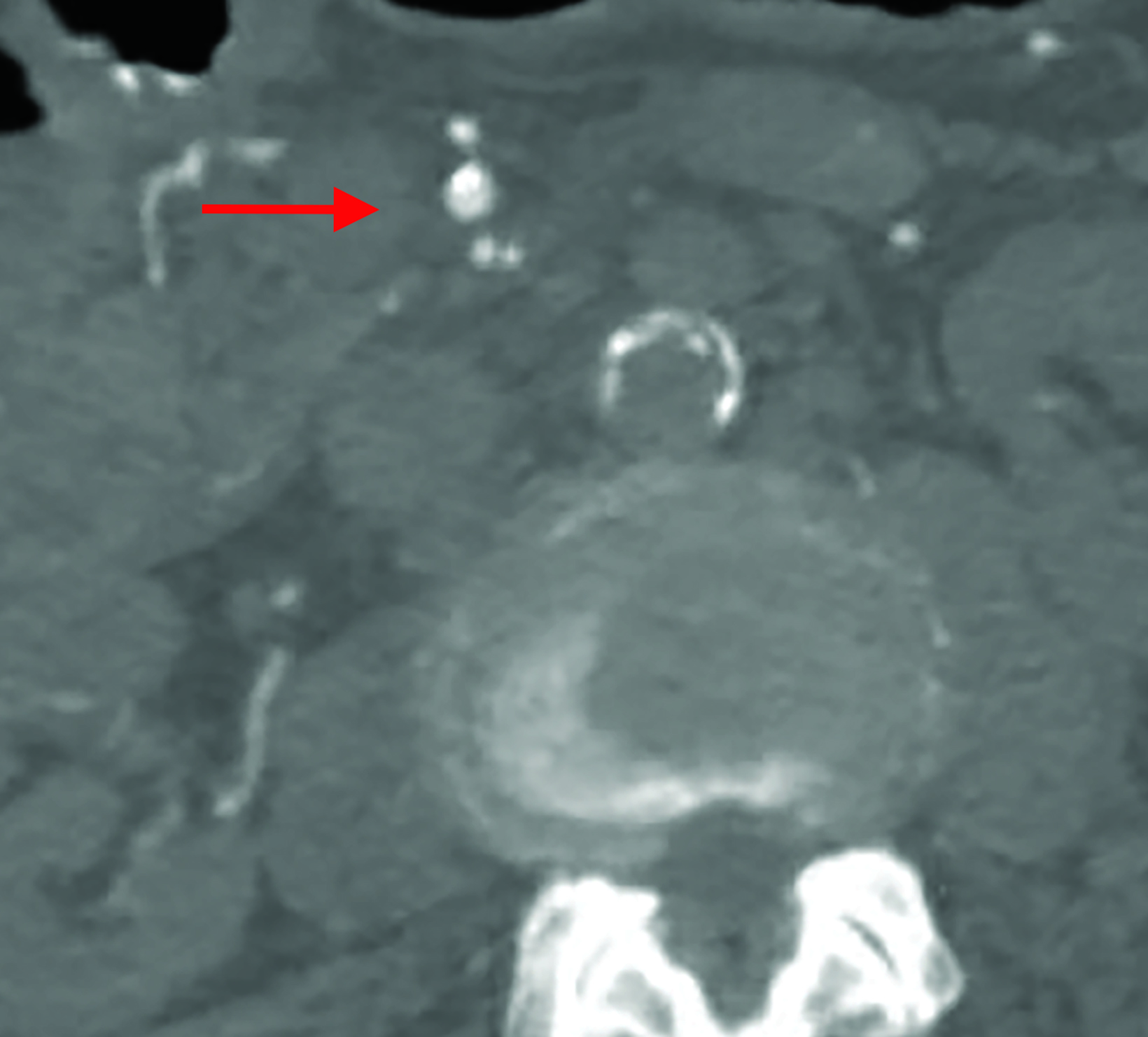
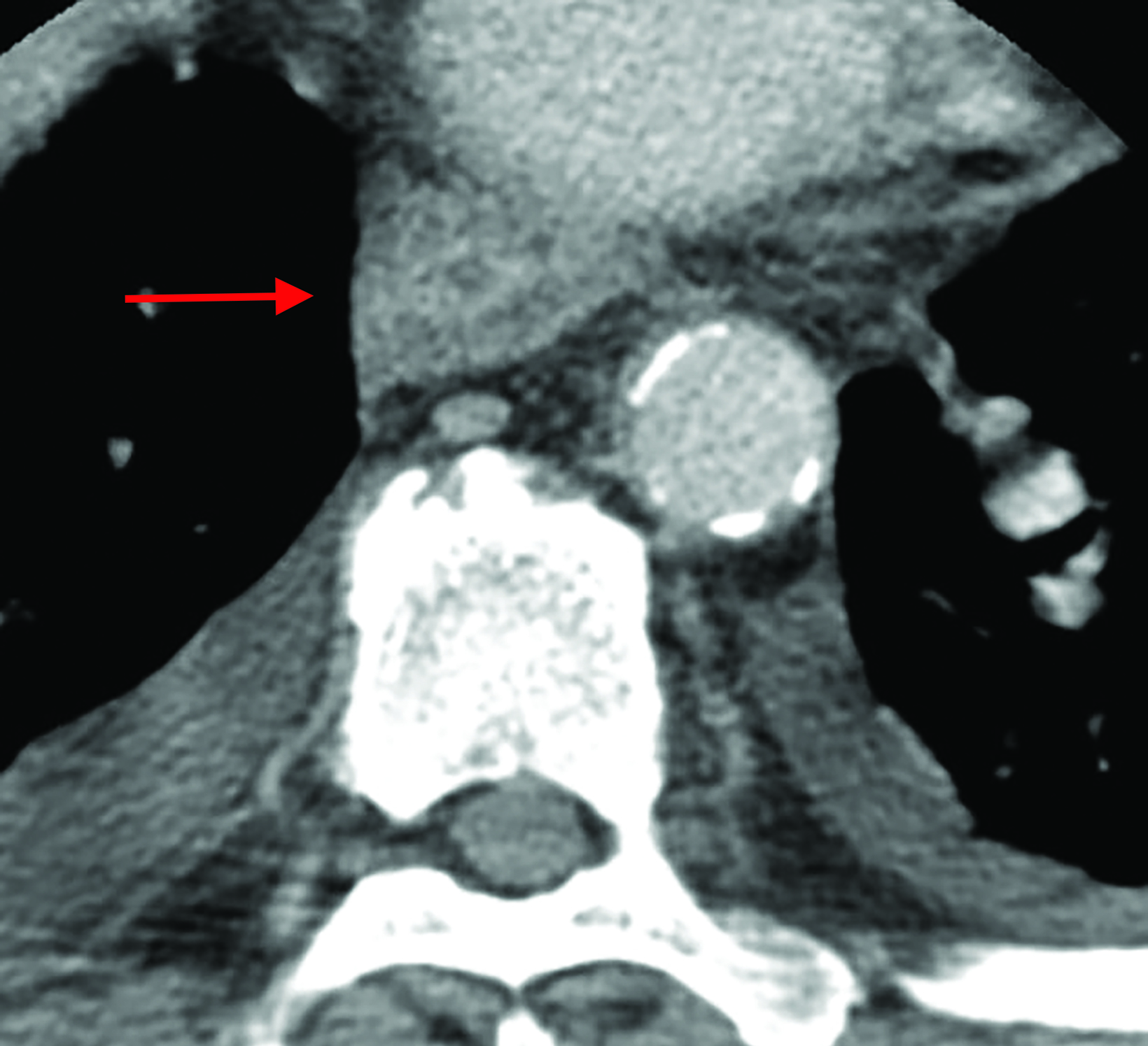
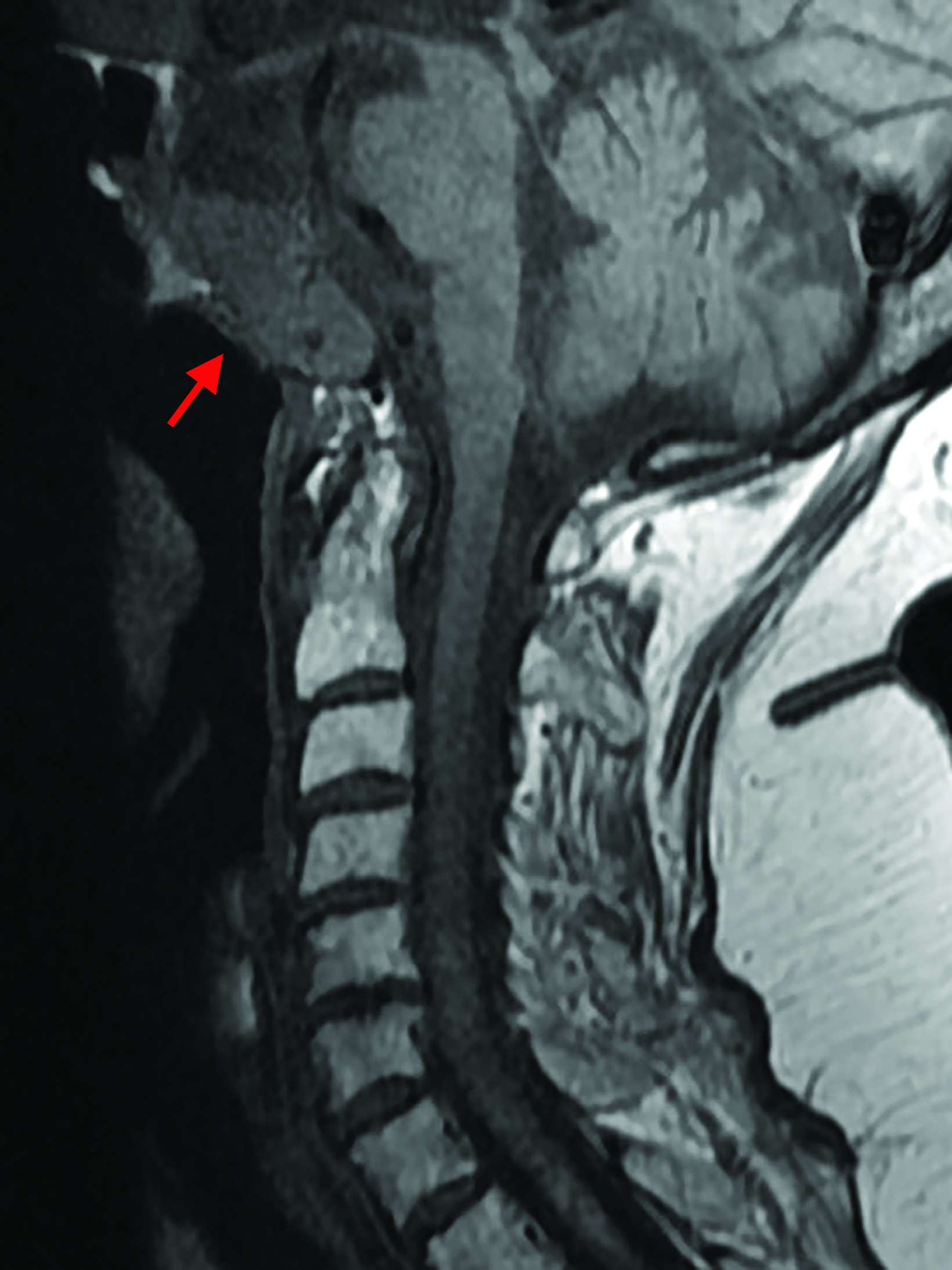
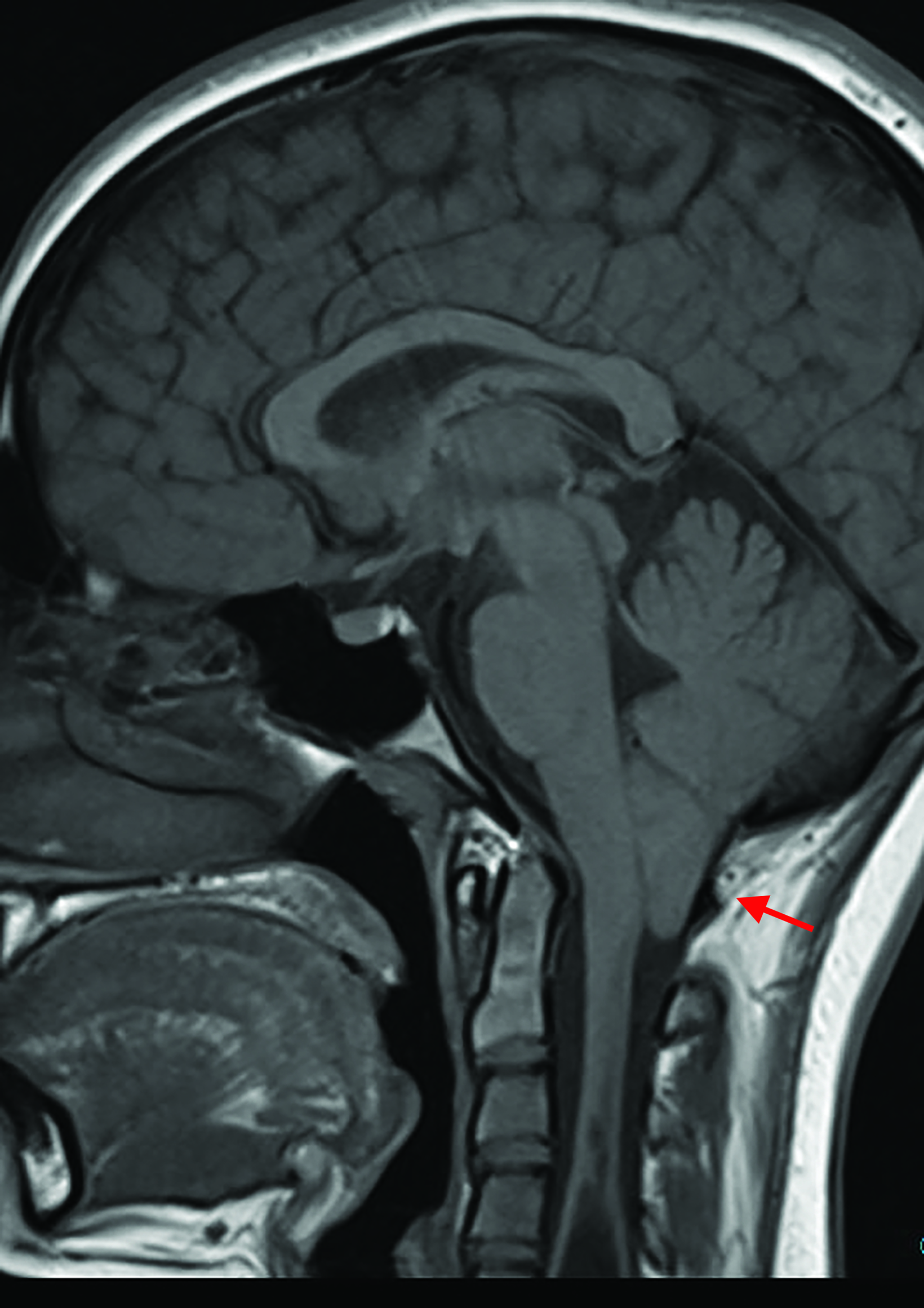
Abnormal vertebral artery flow void on MRI can be a clue to, but not diagnostic of, a vertebral artery dissection (Figure 3), as the artery may be congenitally small or chronically occluded. Posterior circulation infarctions seen at the edge of the field of view on sagittal T2 images of the cervical spine increase the likelihood that the vertebral artery abnormality is real. Protocols with T1 images may also show hyperintense T1 signal from subacute intraluminal thrombus. Vertebral artery dissections are an important cause of neck pain, particularly in younger patients.11 Early treatment with antithrombotic therapy may promote healing and prevent thromboembolism and posterior circulation ischemia/ infarction. Anatomic variants that are not inherently dangerous may become important to recognize prior to surgery or other intervention that may place the artery at risk for injury (Figure 4).
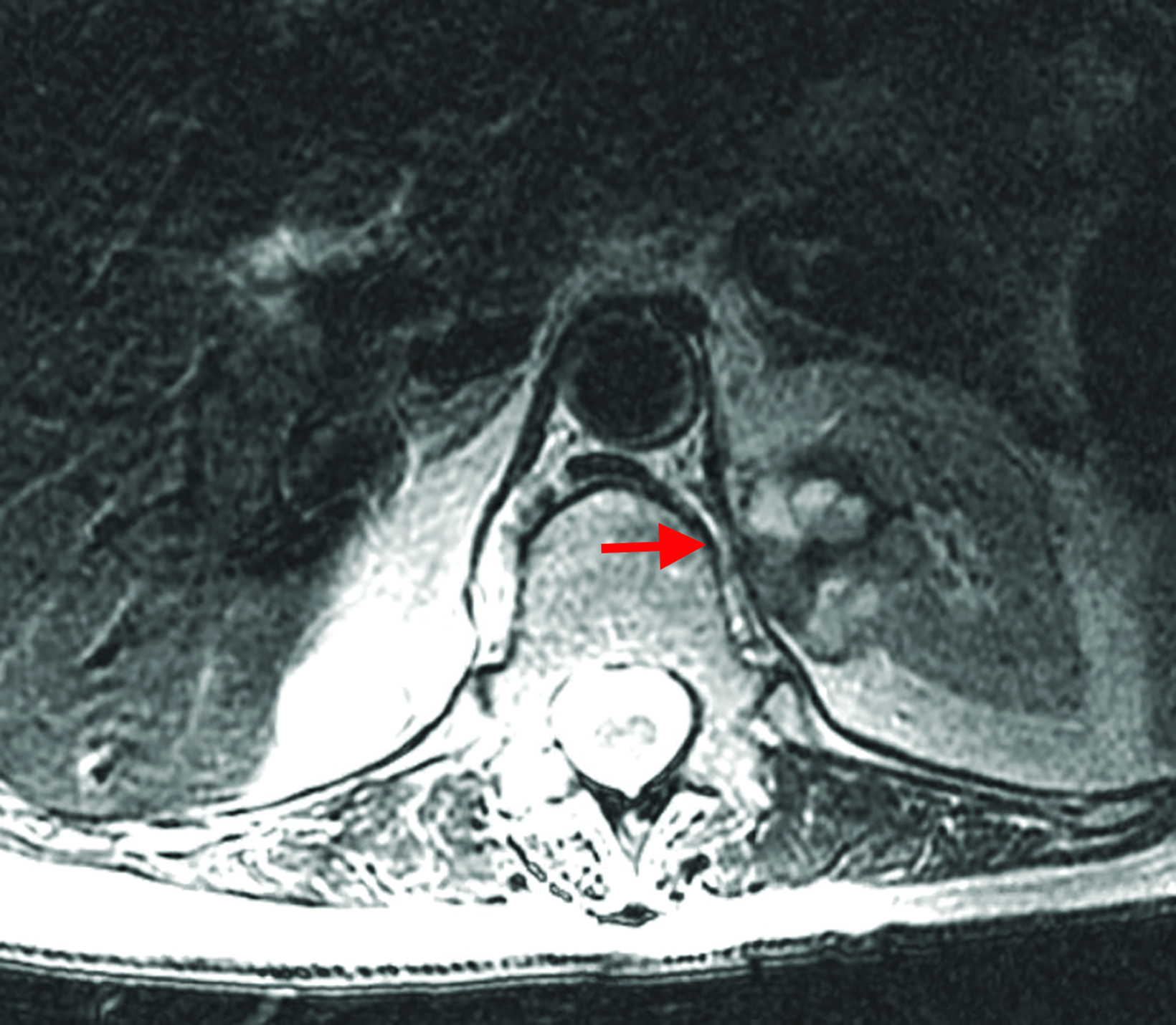
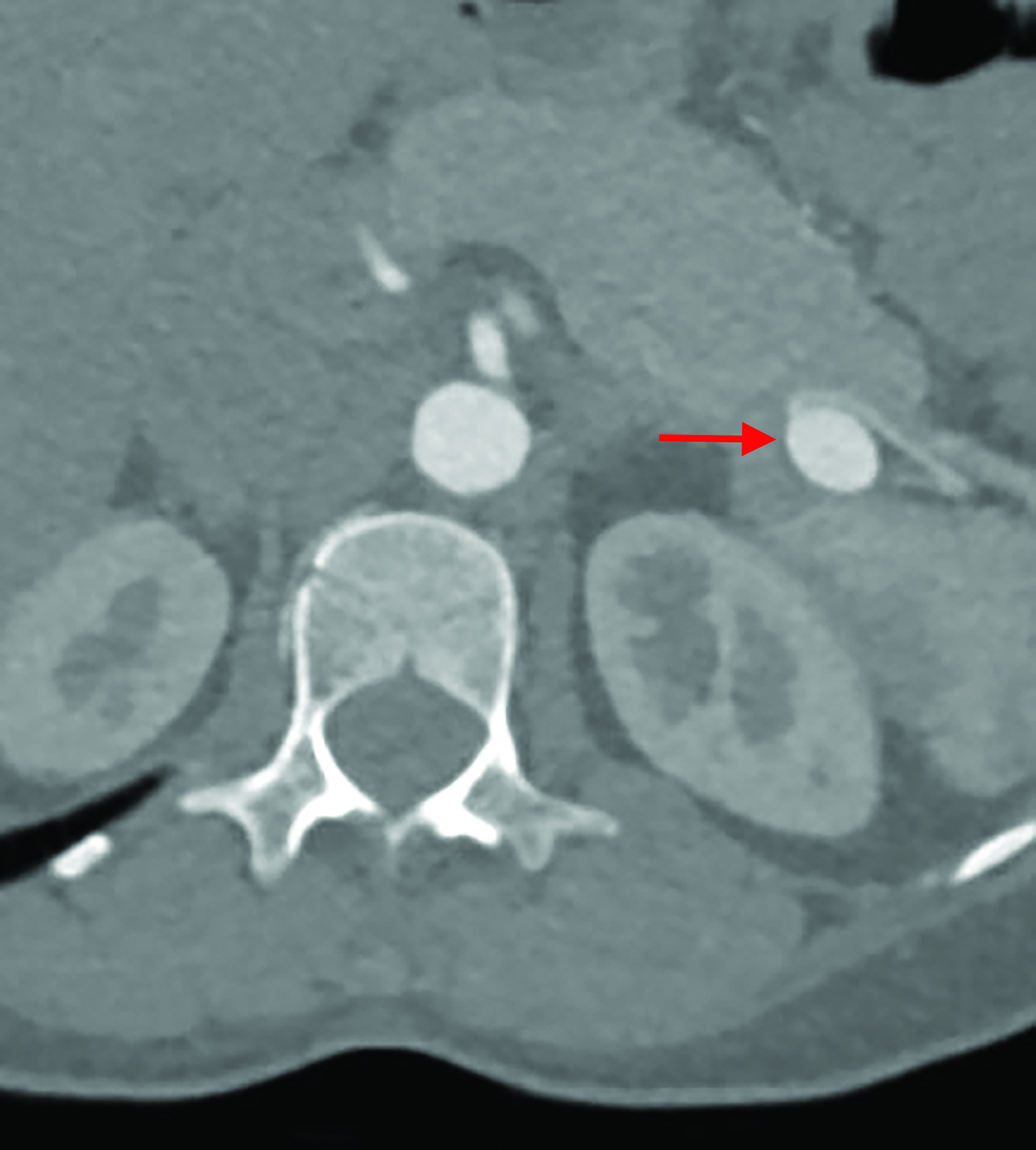
Abnormalities of the aorta are a primary concern when imaging the thoracolumbar spine. Mycotic aneurysms and thoracic aorta dissections may coexist where destructive discitis-osteomyelitis dominates clinical and imaging findings (Figure 5). Abdominal aortic and aorto-iliac aneurysms and stenoses are not uncommon in patients over age 65, particularly those with a smoking history, and they may be first discovered at spine imaging.11 Aorto-iliac occlusion or insufficiency may also present with lower-extremity weakness and urinary incontinence and/or retention, clinically mimicking a compressive myelopathy (Figure 6). Owing to the substantial morbidity associated with undiagnosed abnormalities of the vessel, the thoracoabdominal aorta should be included on the checklist of all spine studies and considered equal in importance to any spondylosis (Figure 7).
Soft-tissue Lesions
Aside from the spinal cord and canal, other critical structures such as the nasopharynx, oropharynx, and cervical lymph nodes are frequently visualized in cervical spine imaging, even in the presence of saturation bands (Figure 8). Most mildly enlarged lymph nodes in younger patients are reactive, but they assume greater importance in patients over age 40. Sagittal MRI may also reveal portions of the posterior fossa and even the sella turcica and cavernous sinuses. Thyroid nodules and masses are also commonly demonstrated. When reviewing thoracolumbar images, radiologists should look out for lung tumors and nodules. Small layering pleural effusions are common, as are esophageal abnormalities that may be a source of pain (Figure 9).
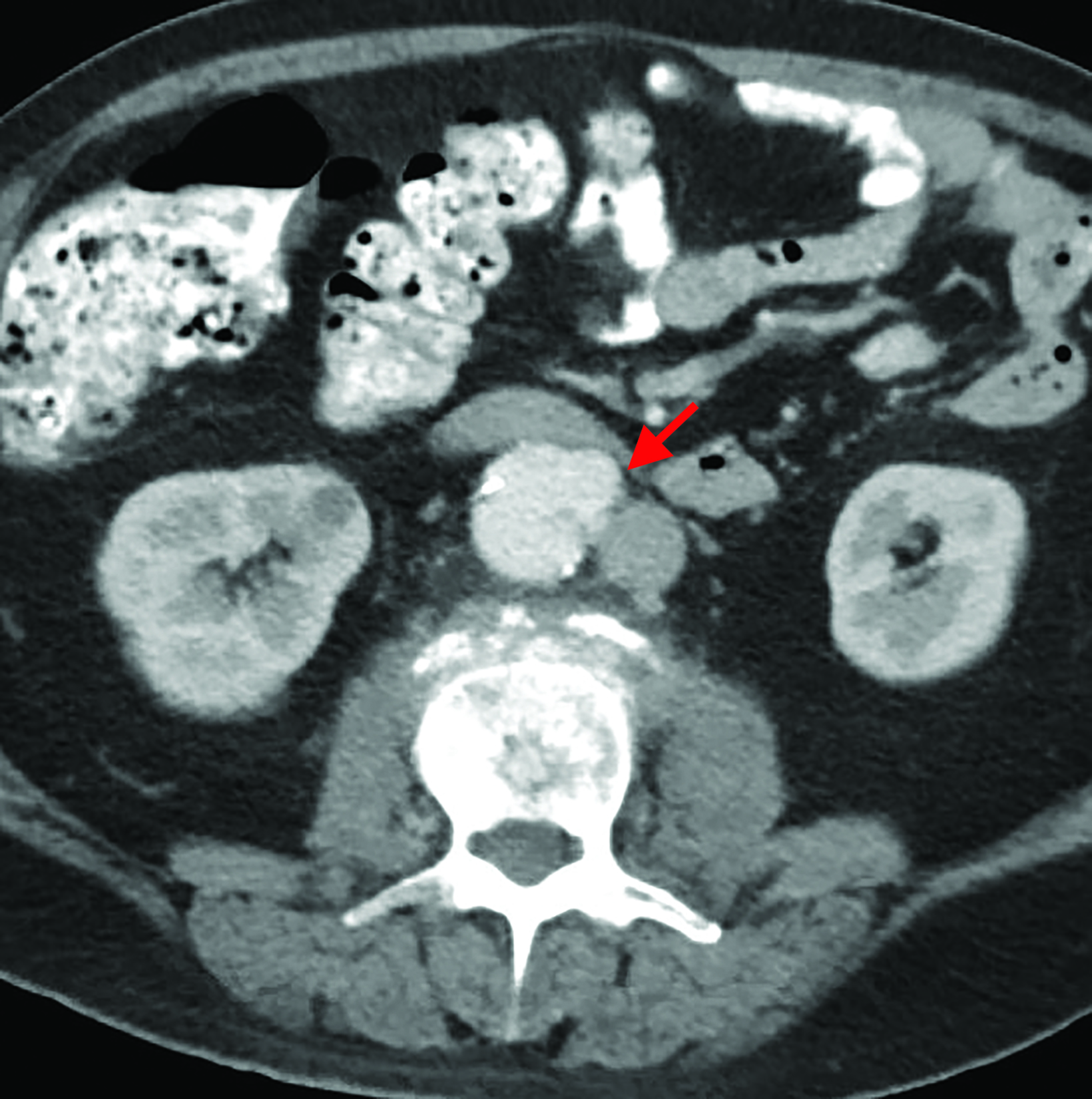
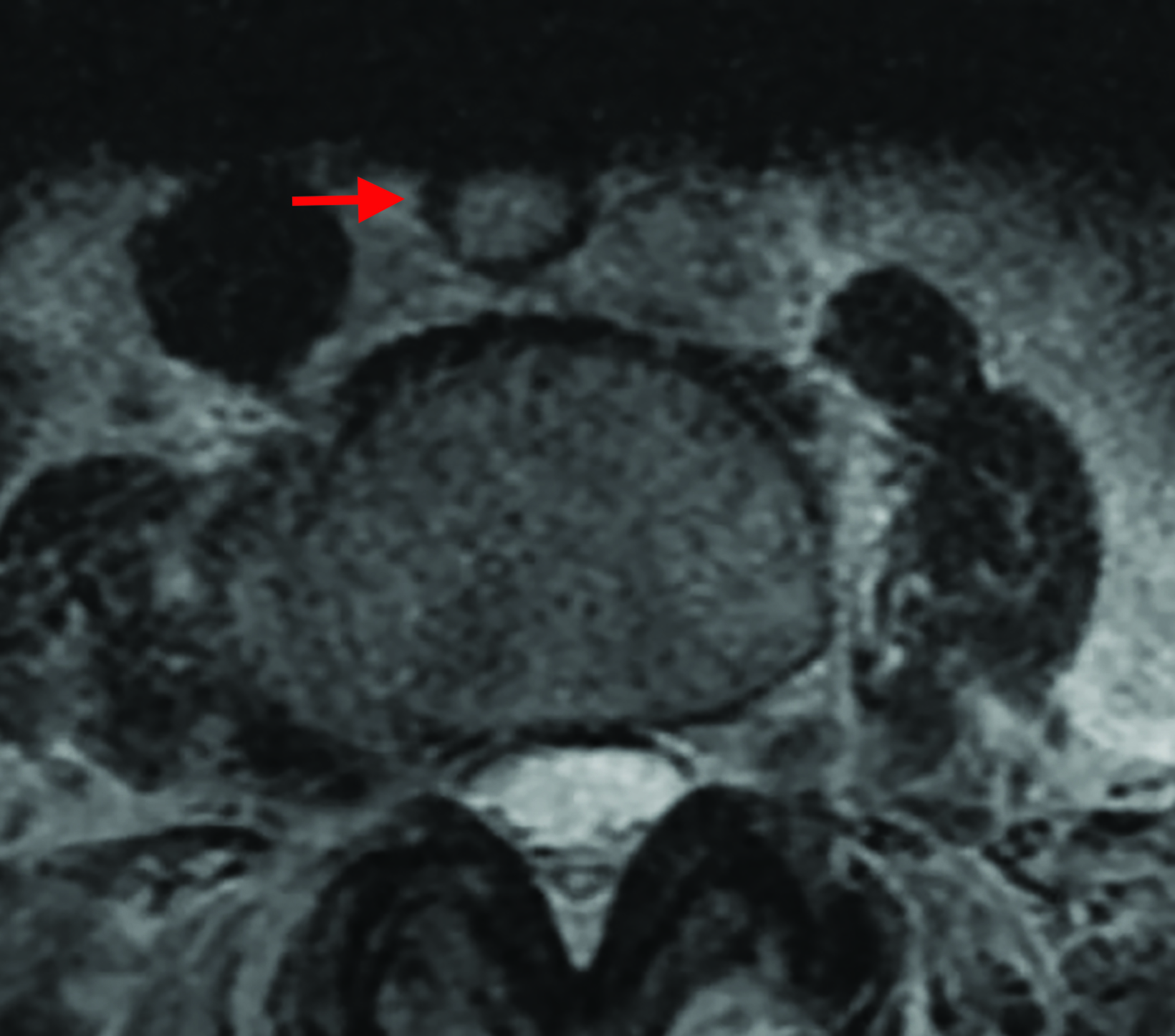
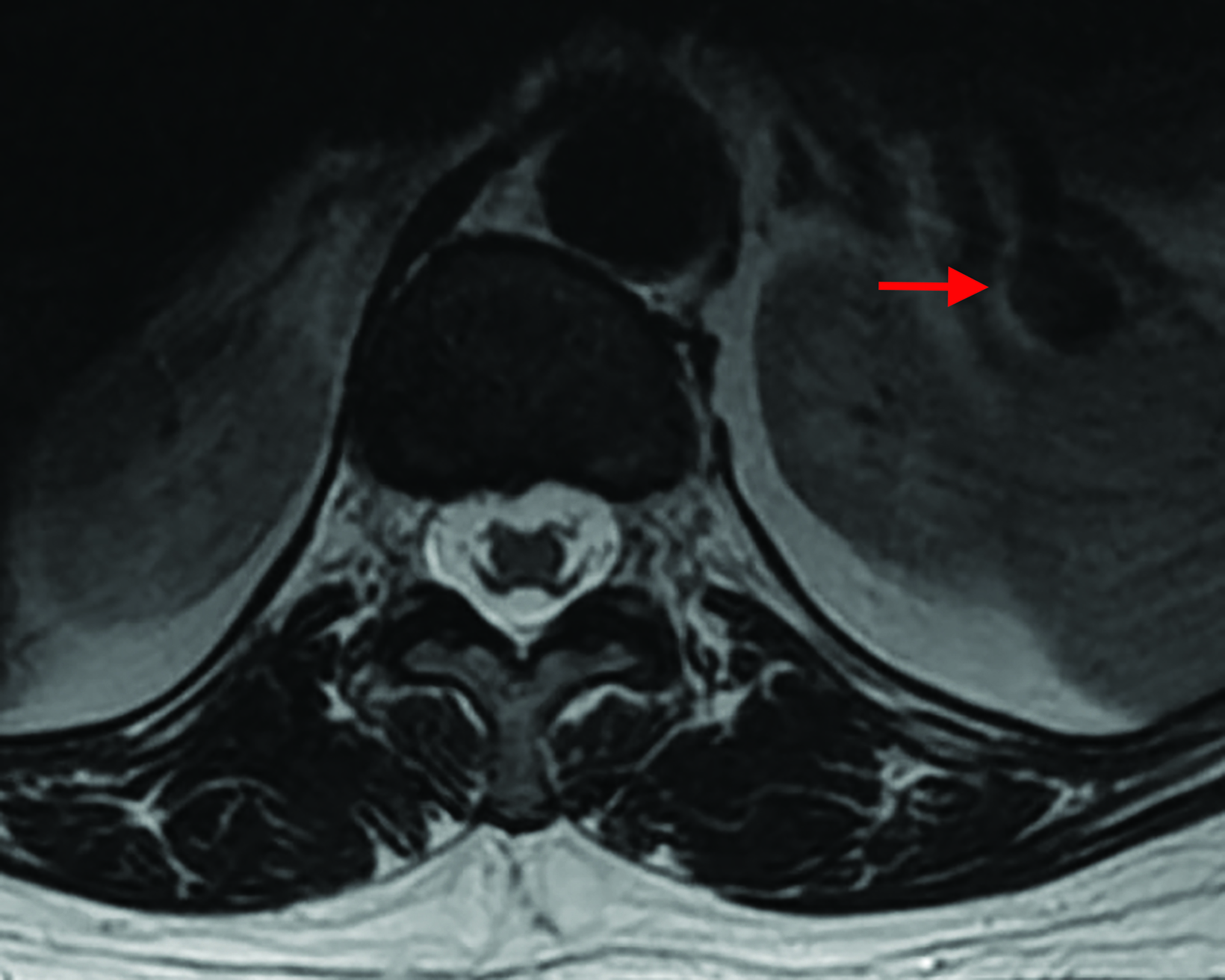
Lumbar spine imaging is often performed to evaluate for low back pain; a careful, level-by-level review of the images for spinal canal and bilateral foraminal and subarticular and lateral recess stenoses can be tedious. However, after a detailed review and report of degenerative changes, an equally careful review for extraspinal findings can be fruitful, especially in older patients. Renal tumors may present with back pain (Figure 10), as may pancreatic, peri-pancreatic (Figure 11), and gall bladder abnormalities. Simple hepatic and renal cysts are common, and they must be reported when they demonstrate concerning features.
Edge-of-Film Findings
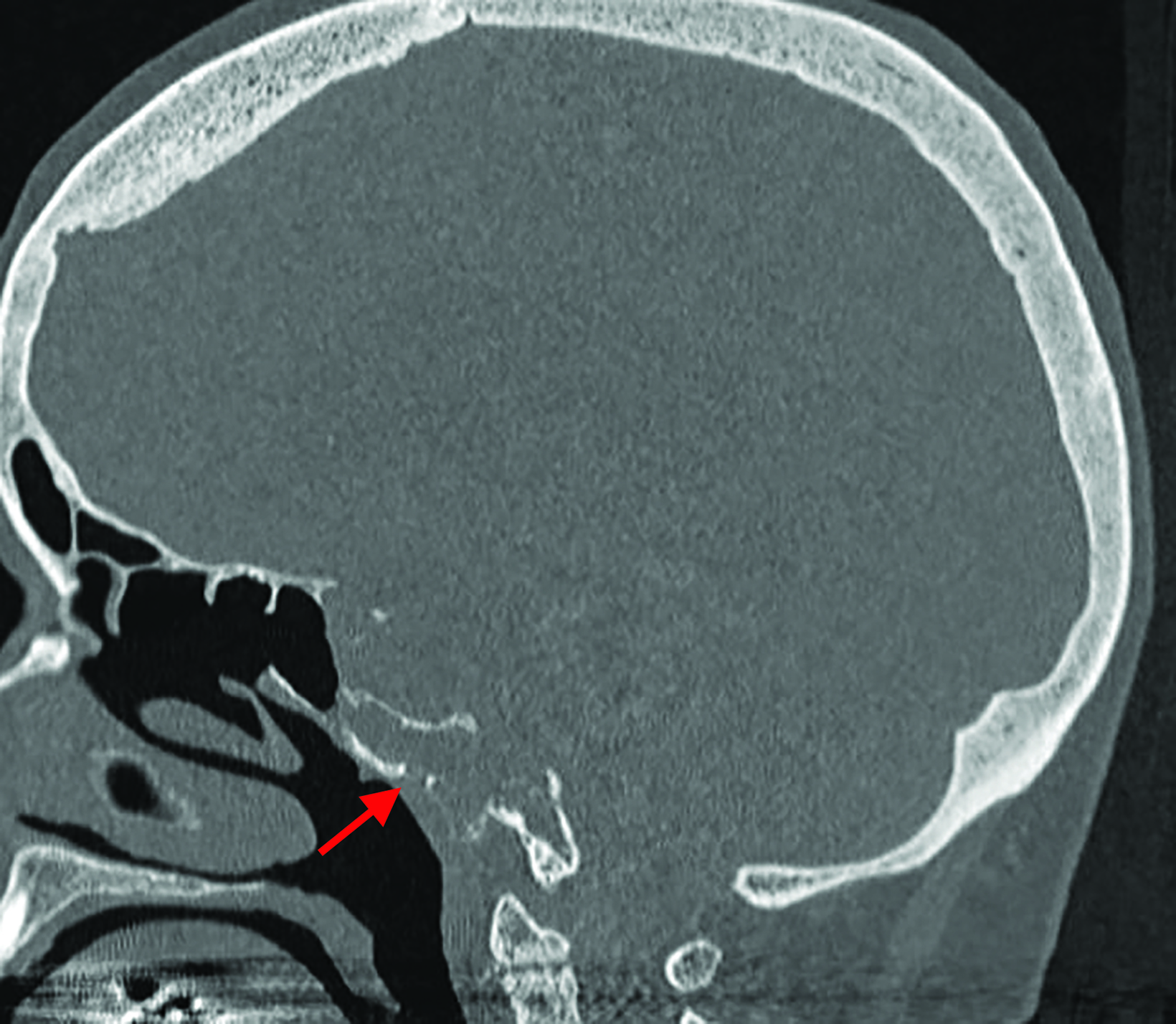
A common subtype of perceptive radiologic error is the so-called “edge-of-film” finding, which has persisted long enough to generate a category of its own. Abnormalities at the edges of the film are more likely to be missed than those at the center. The brain and skull base are at the superior edge of cervical spine films, while the great neck vessels and airway course along the anterior margin (Figure 12). In the lumbar spine, the conus medullaris appears at the superior edge, with the sacrum appearing inferiorly and the lower gastrointestinal tract or genitourinary structures appearing anteriorly.
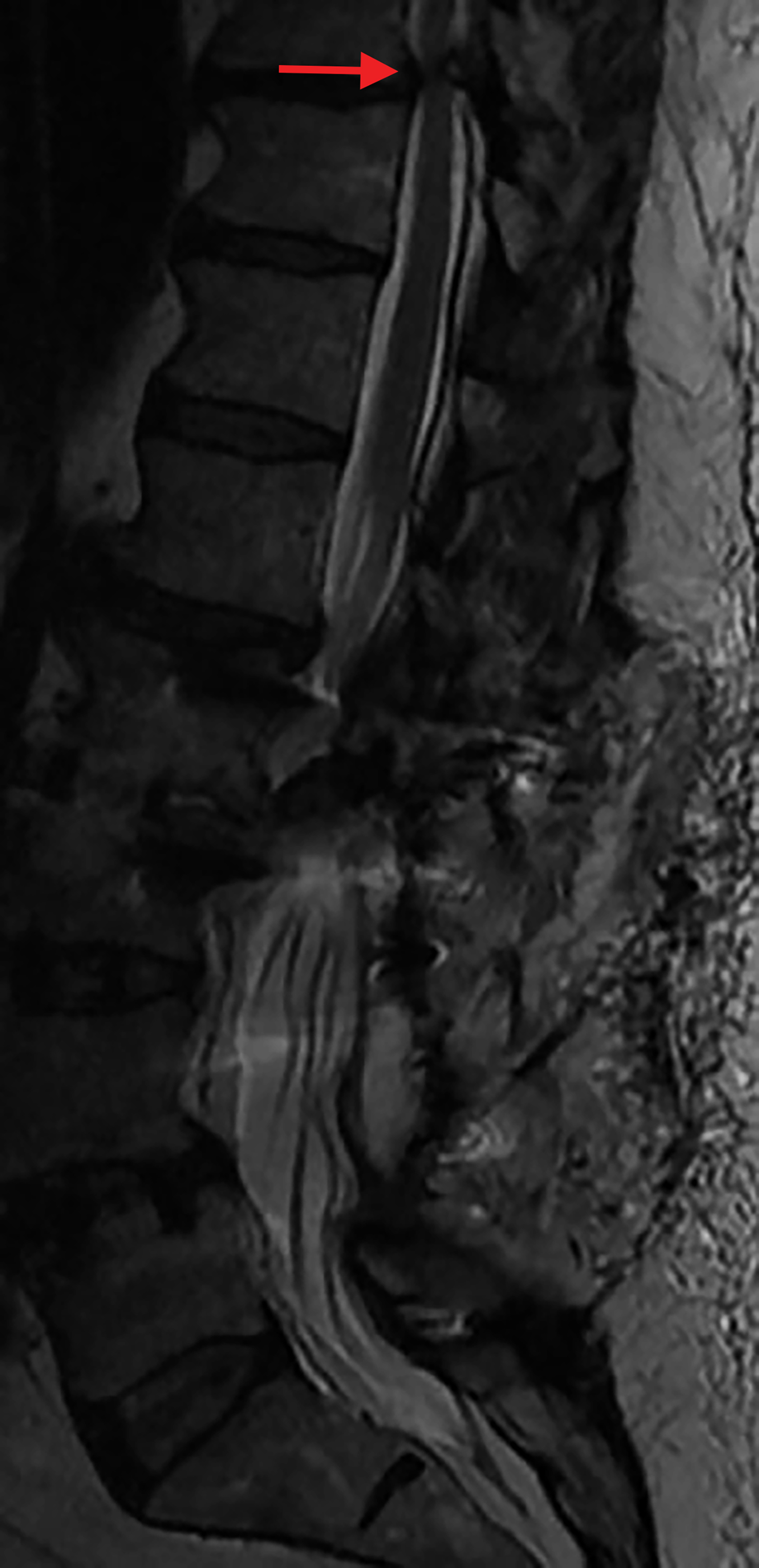
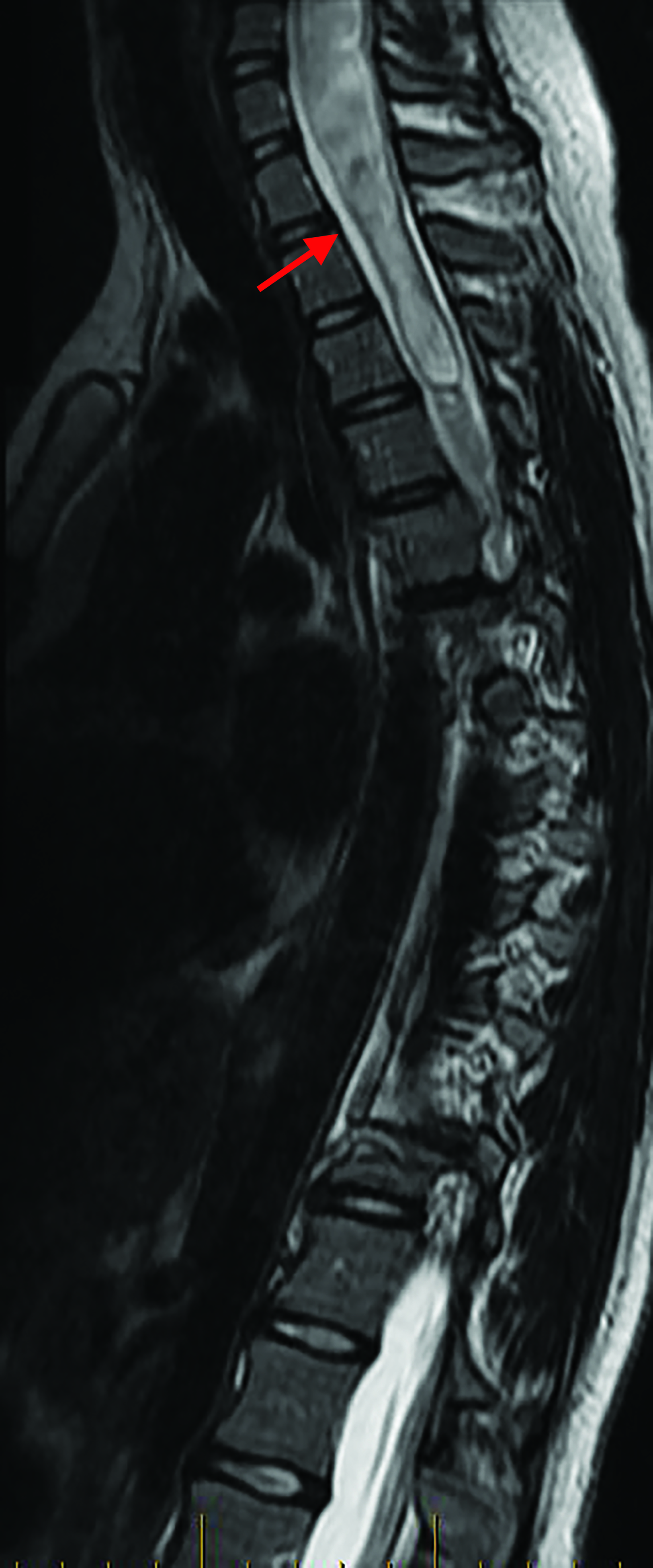
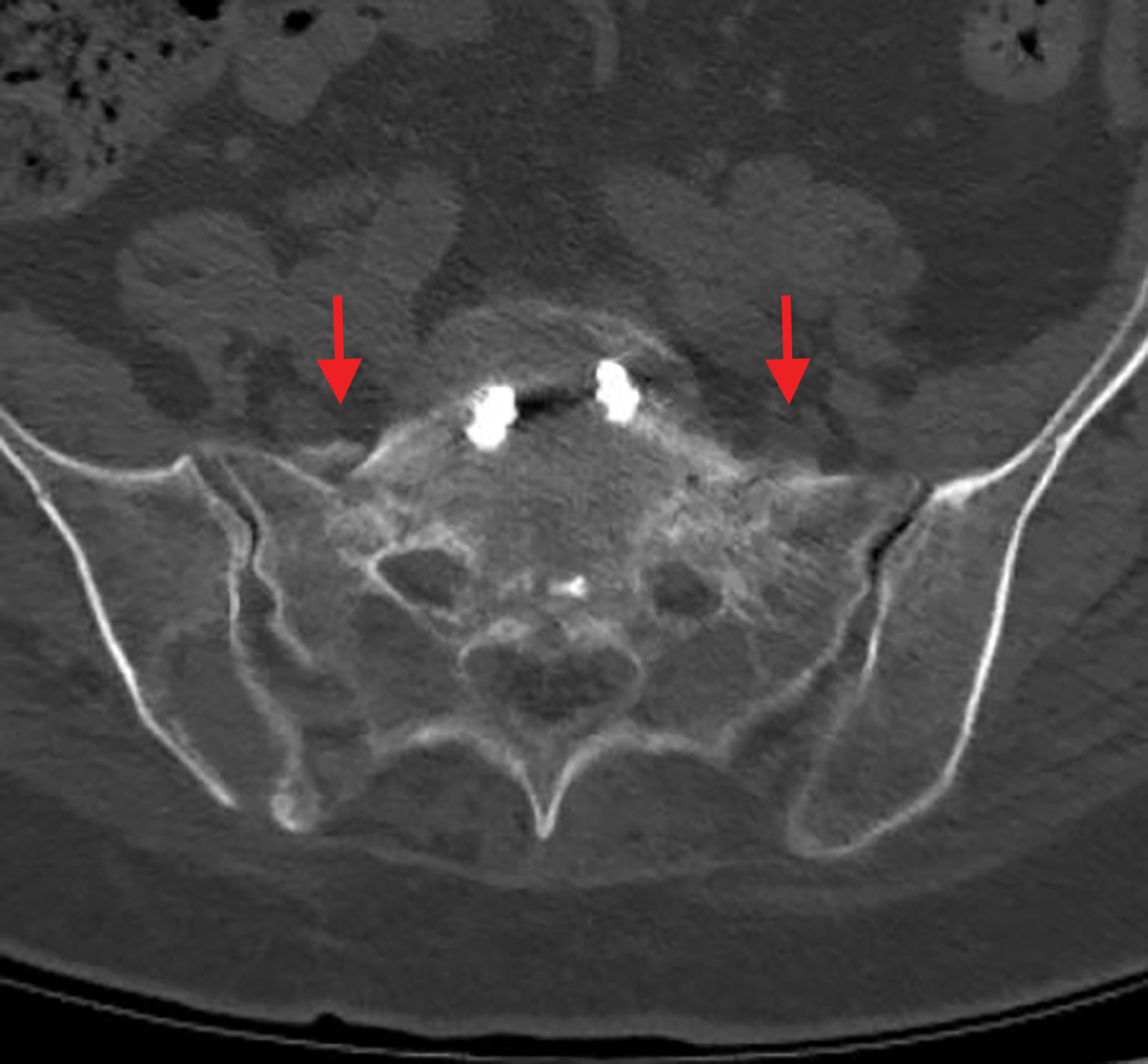
While not extraspinal, abnormal signal intensity in the conus medullaris sometimes goes undetected on lumbar spine studies, resulting in callbacks for additional contrast imaging of the cervical and thoracic spine (Figures 13-15). Other subtle findings may include prominent vessels in cases of dural arteriovenous fistulae (Figure 13). The most common important sacral abnormalities that may be missed are nondisplaced fractures (Figure 16), which can be subtle in older and osteopenic patients.
Conclusion
Extraspinal abnormalities are common in spine imaging, particularly in older patients. Thoroughly searching scout/localizer sequences, vascular structures, extraspinal soft tissues, and edges of the film for these potentially serious entities is important for both trainees and the seasoned radiologists as they interpret cross-sectional spine images to provide optimal patient care.
References
- Freburger JK, Holmes GM, Agans RP, et al. The rising prevalence of chronic low back pain. Arch Intern Med. 2009;169(3):251-258. doi:10.1001/archinternmed.2008.543.
- Chou D, Samartzis D, Bellabarba C, et al. Degenerative magnetic resonance imaging changes in patients with chronic low back pain: a systematic review. Spine (Phila Pa 1976). 2011;36(21 Suppl):S43-S53. doi:10.1097/BRS.0b013e31822ef700.
- Ruutiainen AT, Durand DJ, Scanlon MH, Itri JN. Increased error rates in preliminary reports issued by radiology residents working more than 10 consecutive hours overnight. Acad Radiol. 2013;20(3):305-311. doi:10.1016/j.acra.2012.09.028.
- Itri JN, Tappouni RR, McEachern RO, Pesch AJ, Patel SH. Fundamentals of diagnostic error in imaging. Radiographics. 2018;38(6):1845-1865. doi:10.1148/rg.2018180021.
- Bruno MA, Walker EA, Abujudeh HH. Understanding and Confronting Our Mistakes: The epidemiology of error in radiology and strategies for error reduction. Radiographics. 2015;35(6):1668-1676. doi:10.1148/rg.2015150023.
- Patel SH, Stanton CL, Miller SG, Patrie JT, Itri JN, Shepherd TM. Risk factors for perceptual-versus-interpretative errors in diagnostic neuroradiology. AJNR Am J Neuroradiol. 2019;40(8):1252-1256. doi:10.3174/ajnr.A6125.
- Johnson PT, Scott WW, Gayler BW, Lewin JS, Fishman EK. The CT scout view: does it need to be routinely reviewed as part of the CT interpretation? AJR Am J Roentgenol. 2014;202(6):1256-1263. doi:10.2214/AJR.13.10545.
- Daffner RH. Reviewing CT scout images: Observations of an expert witness. AJR Am J Roentgenol. 2015;205(3):589-591. doi:10.2214/AJR.15.14405.
- Berlin L. Reviewing the CT scout view: medicolegal and ethical considerations. AJR Am J Roentgenol. 2014;202(6):1264-1266. doi:10.2214/AJR.12.10444.
- Smith WS, Johnston SC, Skalabrin EJ, Weaver M, Azari P, Albers GW, Gress DR. Spinal manipulative therapy is an independent risk factor for vertebral artery dissection. 2003 May 13;60(9):1424-8.
- Silbert PL, Mokri B, Schievink WI. Headache and neck pain in spontaneous internal carotid and vertebral artery dissections. Neurology. 1995;45(8):1517-1522. doi:10.1212/wnl.45.8.1517.
- Brinjikji W, Nasr DM, Morris JM, Rabinstein AA, Lanzino G. Clinical outcomes of patients with delayed diagnosis of spinal dural arteriovenous fistulas. AJNR Am J Neuroradiol. 2016;37(2):380-386. doi:10.3174/ajnr.A4504.
References
Citation
M C, L B, J P, ThatcherJ, ThackerI, C G, K L.Blind Spots in Spine Imaging. Appl Radiol. 2022; (2):15-23.
March 4, 2022