AI Tool Has Potential to Flag Mammograms for Supplement Breast MRI
Images
Artificial intelligence (AI) effectively identified women at higher breast cancer risk in a select Dutch population, according to a study published in Radiology. Applying the AI tool to mammograms has the potential to improve breast cancer detection by identifying the patients that may benefit the most from breast MRI scans, this study indicates.
To achieve optimal detection accuracy, international recommendations suggest combined mammography and MRI screening for women with a lifetime risk of 20% or higher based on family history. However, in the Netherlands, women with a breast cancer risk between 20% and 50% do not typically have access to supplemental MRI screening due to limited MRI capacity, high implementation costs, and inconsistent application of eligibility criteria in clinical practice.
"Evidence demonstrating the benefits of MRI screening in this subgroup of women is accumulating," said the study's lead author, Suzanne van Winkel, RN, MSc, a PhD candidate at Radboud University Medical Center (Radboudumc) in Nijmegen, Netherlands. "MRI detects cancers that remain undetected by mammography and are smaller and more often lymph node negative."
Many recent studies have demonstrated the potential of AI for improving cancer detection on mammography screening, including cancers not visible on the mammogram according to radiologist interpretation. AI could, therefore, be used to triage mammograms and select women that could potentially benefit from supplemental MRI after a negative mammogram according to radiologist interpretation.
For the purposes of this retrospective study, women with a personal history of breast cancer, dense breasts or a history of high-risk lesions at biopsy, and women with an increased risk based upon family history but no genetic mutations were referred to as "intermediate risk."
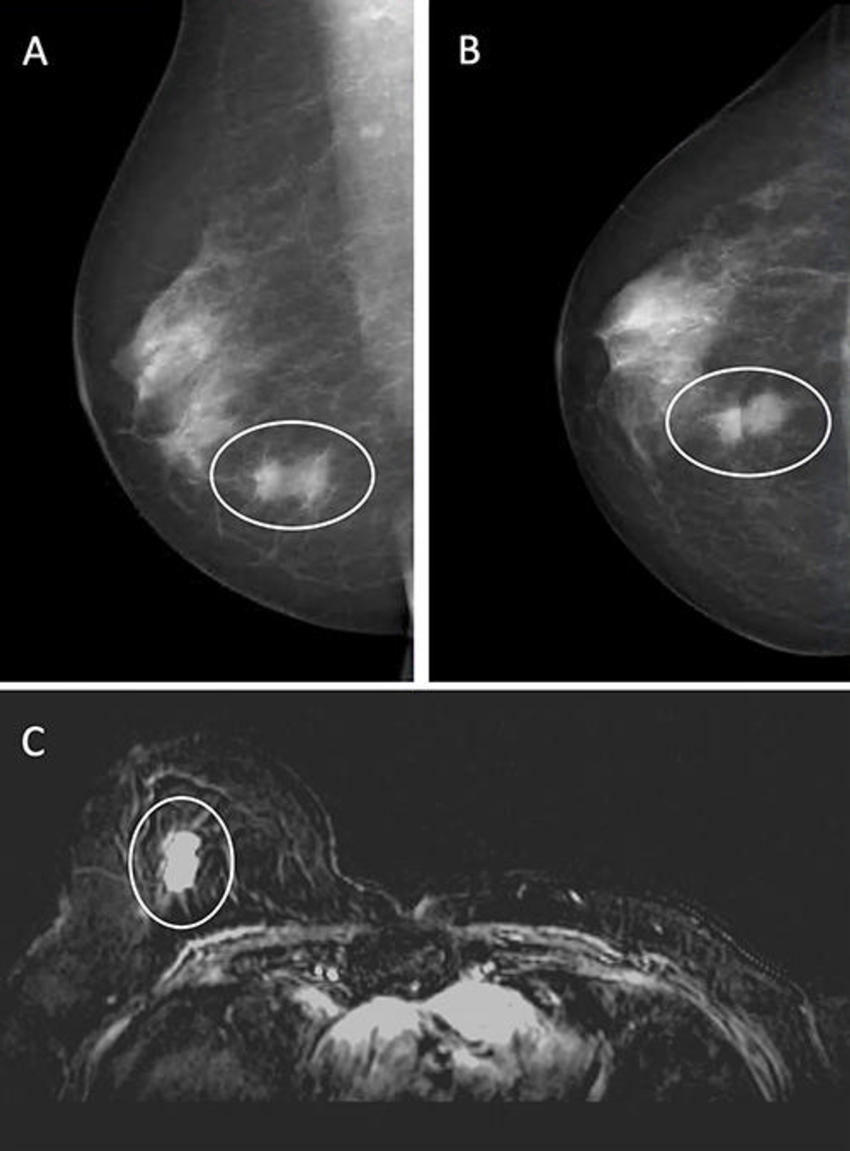
The researchers used a commercially available AI system to analyze the 2D screening mammograms of women they classified as intermediate risk to identify patients with the greatest likelihood of mammographically occult (not visible on mammography) cancer for supplemental MRI.
The researchers extracted a cohort of 1,833 consecutive women who had at least one screening MRI combined or alternated with a screening mammogram between 2003 and 2020 from the patient breast MRI database at Radboudumc. Women with a lifetime breast cancer risk greater than 50% were excluded.
A total of 3,358 mammography exams in 875 women were performed. Of those, 2,819 (84%) exams in 760 women (mean age 48.9 years) were processed by the AI system and assigned a case-based suspicion score (0-10) that ranked the likelihood of a malignancy.
The combined exams detected 37 (1.3%) breast cancers. In 19 (51%) of these cases, the cancer was not visible on mammography.
Using a threshold score of 5 (allowing supplemental MRI-screening in 50% of the women involved), AI selected 31 (84%) of the breast cancer-positive exams for supplemental MRI, including 68% of exams with occult breast cancer based on the radiologists' reading.
"AI could potentially triage mammograms performed in the subgroup and select women that could potentially benefit from supplemental MRI after a negative mammogram," said van Winkel. "Using AI to triage the mammograms of populations who are not yet eligible for MRI may improve screening results while simultaneously reducing unnecessary costs."
Stamatia Destounis, MD, a breast radiologist at Elizabeth Wende Breast Care, in Rochester, NY, added some important perspective on the findings.
"This is an interesting retrospective study that reveals by using AI a certain percentage of cancers not identifiable on mammography can be found on breast MRI," commented Dr Destounis, who is not affiliated with the study. "However, the AI doesn't predict every patient with cancer and some cancers—whether seen on the mammogram or not—are not detected by their AI model. In the U.S., the subgroup of patients considered intermediate risk by the study authors would likely fall in the high-risk category and would be recommended to undergo a high-risk MRI, allowing the radiologist to identify all cancers, even those occult on mammography."