Worrisome and Incidental Signs on Knee Radiographs in Clinical Practice: Traumatic and Degenerative Lesions
Images















SA-CME credits are available for this article here.
Editor’s note: This is the first part of a two-part series. The second part will appear in the March/April 2023 issue of Applied Radiology.
Most diagnostic errors by radiologists in clinical practice involve musculoskeletal findings on radiographs, and missed fractures represent more than 90% of malpractice claims.1,2
Knee radiography is one of the most common musculoskeletal studies interpreted by radiologists in daily clinical practice and is the standard of care for initial imaging of acute or chronic knee pathology.3-5 A variety of knee radiography protocols exist, but every study should at minimum contain frontal (anteroposterior [AP] or posteroanterior) and lateral views.4 Other common options in a knee radiograph series include weight-bearing, patellar tangential, oblique, and cross-table lateral views.4,6,7
In this article we describe worrisome imaging signs on knee radiographs to inform radiologists and radiologists-in-training how to identify a select group of difficult-to-diagnose traumatic pathologies and when to recommend additional imaging or clinical work up. We also discuss incidental signs of degenerative joint disease and a developmental anomaly on knee radiographs that mimics worrisome pathology, in order to allow definitive diagnosis and to bestow confidence that no further work up is required.
Traumatic Fractures
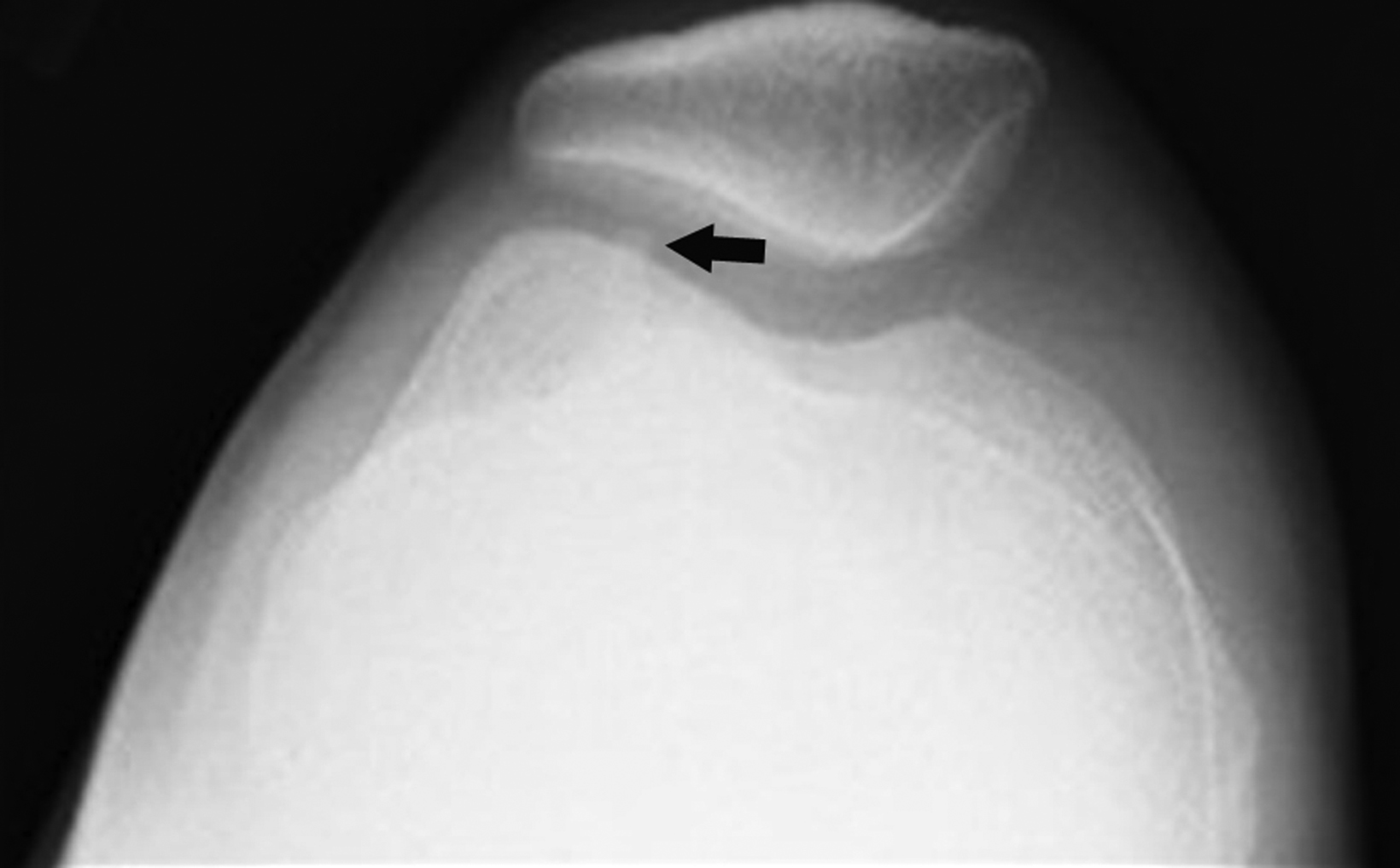
Segond Fracture
The Segond fracture is important to recognize due to its strong association with anterior cruciate ligament (ACL) and meniscal tears.8 The typical mechanism involves excessive internal rotation and varus stress, which cause a focal avulsion of bone from the lateral tibial plateau, commonly sustained as a sports-related injury. Patients commonly present with acute knee pain.9
On radiographs, the Segond fracture appears as a small, avulsed bone fragment from the lateral tibial plateau (Figure 1). Although the injury is subtle in appearance on radiographs, magnetic resonance imaging (MRI) demonstrates the strong association with ACL tear to greater detail).7 The primary emphasis is placed on surgical intervention for the underlying knee internal derangement.10
Tibial Spine Fracture
Tibial spine fractures most often occur in skeletally immature knees. This injury is considered equivalent to adult ACL tears, as children and adolescents have a greater propensity to suffer acute bone injury from ACL avulsion of the tibial spines rather than ligamentous tear of the ACL as compared to adults.11 Mechanisms for injury include abnormal knee rotation or blunt trauma near the anterior knee while the joint is flexed. Patients typically present with pain, swelling, and decreased range of motion.12
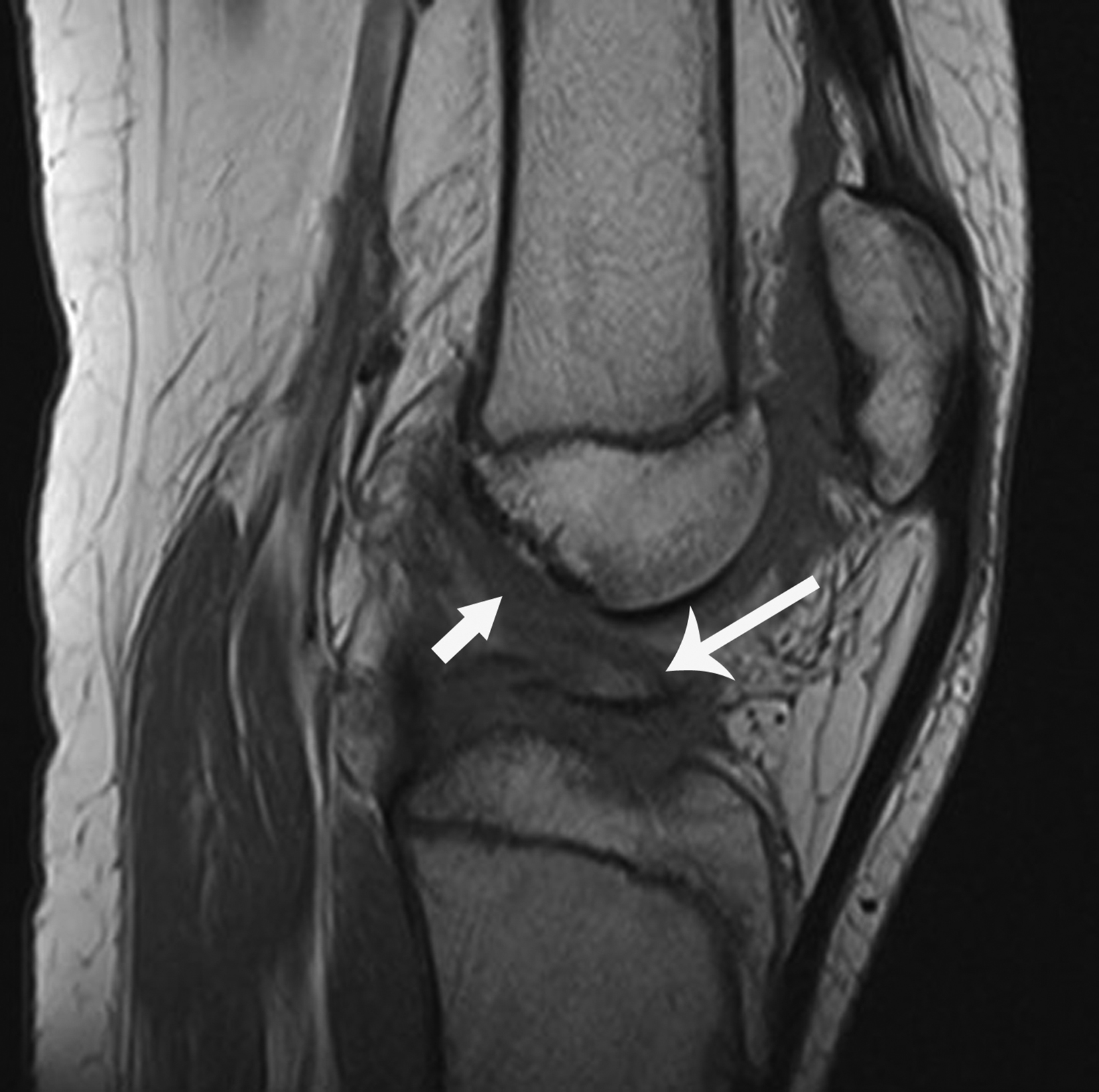
Tibial spine fractures appear through the central region of the proximal tibia epiphysis, often with an associated knee joint effusion (Figure 2). Computed tomography (CT) and MRI have greater sensitivity to delineate fracture characteristics, while MRI can also be used to diagnosis additional meniscal, ligamentous, and/or articular cartilage internal derangements relevant for preopera- tive planning.11 Treatment of these fractures with ACL avulsion typically consists of surgery or casting in the pediatric population.11
Lipohemarthrosis
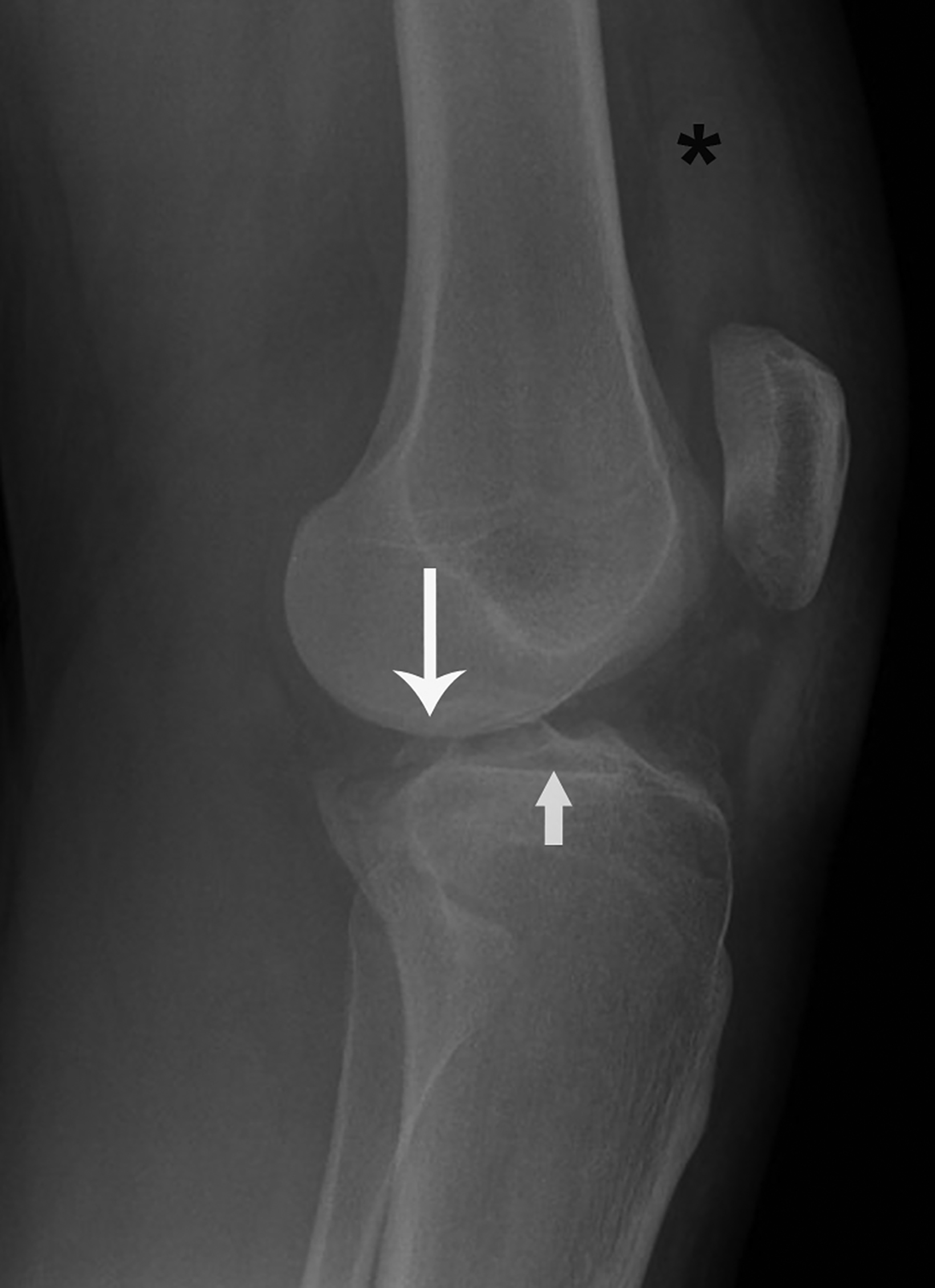
In the acutely traumatized knee, systematic evaluation of the soft tissues is required. Lipohemarthrosis, defined as intra-articular floating fat in a joint effusion, is an important clue for diagnosing radiographically-occult fractures.6,13 Traumatic intra-articular fracture is the primary mechanism for fatty marrow leakage into the joint space and lipohemarthrosis is pathognomonic for acute fracture.6,14 Acute pain and swelling are classic symptoms/signs.
Radiologists should consider cross-table lateral radiographs for all traumatic knee series, as standard frontal and lateral views are less likely to identify lipohemarthrosis.6,15 On cross-table lateral views, the key finding is a sharp linear interface between hydrophobic floating fat and hydrophilic hemarthrosis, most commonly seen at the suprapatellar pouch (Figure 3). Occasionally, lipohemarthrosis will present with three distinct layers when the hemarthrosis further separates into distinct serum and red blood cell layers.6,16 In the setting of lipohemarthrosis without a definite radiographically visible fracture, the radiologist should inform the exam requestor that additional cross-sectional imaging is indicated to detect and characterize the occult fracture.17 Treatment is typically driven by orthopedic management of the underlying fracture, with self-resolution of the lipohemarthrosis.
Traumatic Malalignment
Anterior tibial translation
Anterior tibial translation (ATT) is an important radiographic sign of knee instability.18 The ACL primarily resists ATT but when torn allows abnormal anterior subluxation of the tibia relative to the femur.19,20 In the acute clinical setting, severe pain and swelling are common. In cases of subacute clinical presentation, perceived instability may be the most pressing concern.21
On a lateral knee radiograph, ATT appears as the central region of the femoral condyles articulating with the posterior third of the proximal tibial plateau (Figure 4). In this setting, MRI may be considered to definitively characterize the ACL tear and identify other potential injuries. Treatment is based on orthopedic management of the tear and any other associated internal derangements.
Patella Alta
Patella alta is a “high-riding” patella that rests in a more proximal position than expected relative to the tibiofemoral articulation. Most cases represent a developmental anomaly, but acquired patella alta is suspicious for a ruptured patellar tendon. Acutely acquired patella alta typically presents with new-onset knee pain, swelling, and decreased range of motion.22,23 Chronic patella alta presents with a more insidious onset of patellofemoral pain and recurrent patellar subluxation or dislocation.24,25
Patella alta is most commonly evaluated on the lateral knee radiograph using the Insall-Salvati method (Figure 5). Patella alta is diagnosed when the distance from the inferior pole of the patella to tibial tuberosity is more than 20% of the maximum oblique distance across the patella.26 Thus, a ratio of more than 1.2 indicates patella alta on a lateral knee radiograph. The condition is managed orthopedically on a case-by-case basis, depending on the underlying cause and presenting symptoms.27
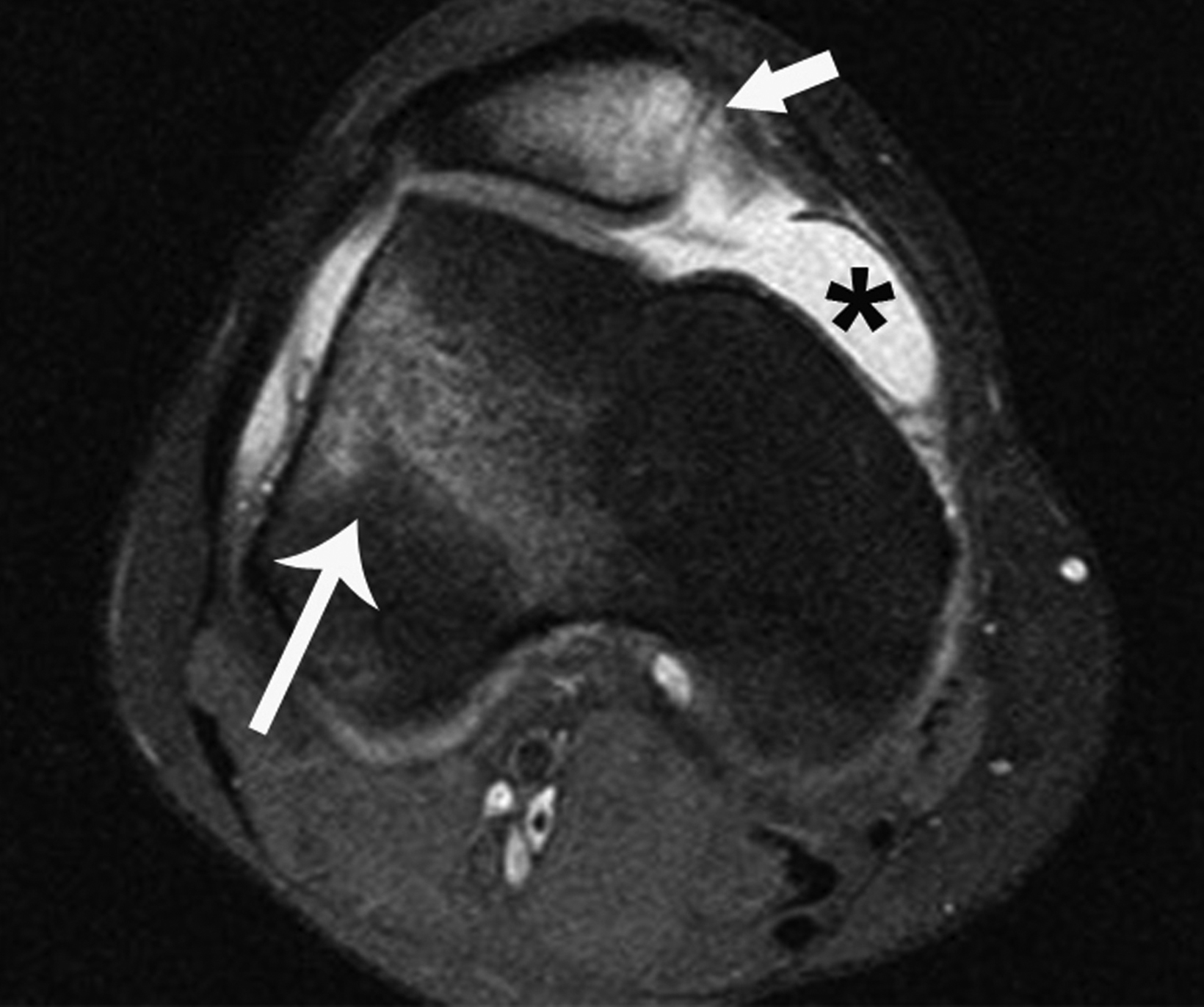
Transient Patellar Dislocation
Transient patellar dislocation (TPD) is a knee instability syndrome affecting the patellofemoral compartment. The term “transient” implies brief events of lateral patellar subluxation or dislocation followed by spontaneous reduction.28,29 Although TPD may occur at any age, adolescents and young adults classically are most affected. Patients often present with knee pain and a history of patellar dislocation with spontaneous reduction. Clinically, TPD is elusive, and more than 50% of cases are initially clinically misdiagnosed.28
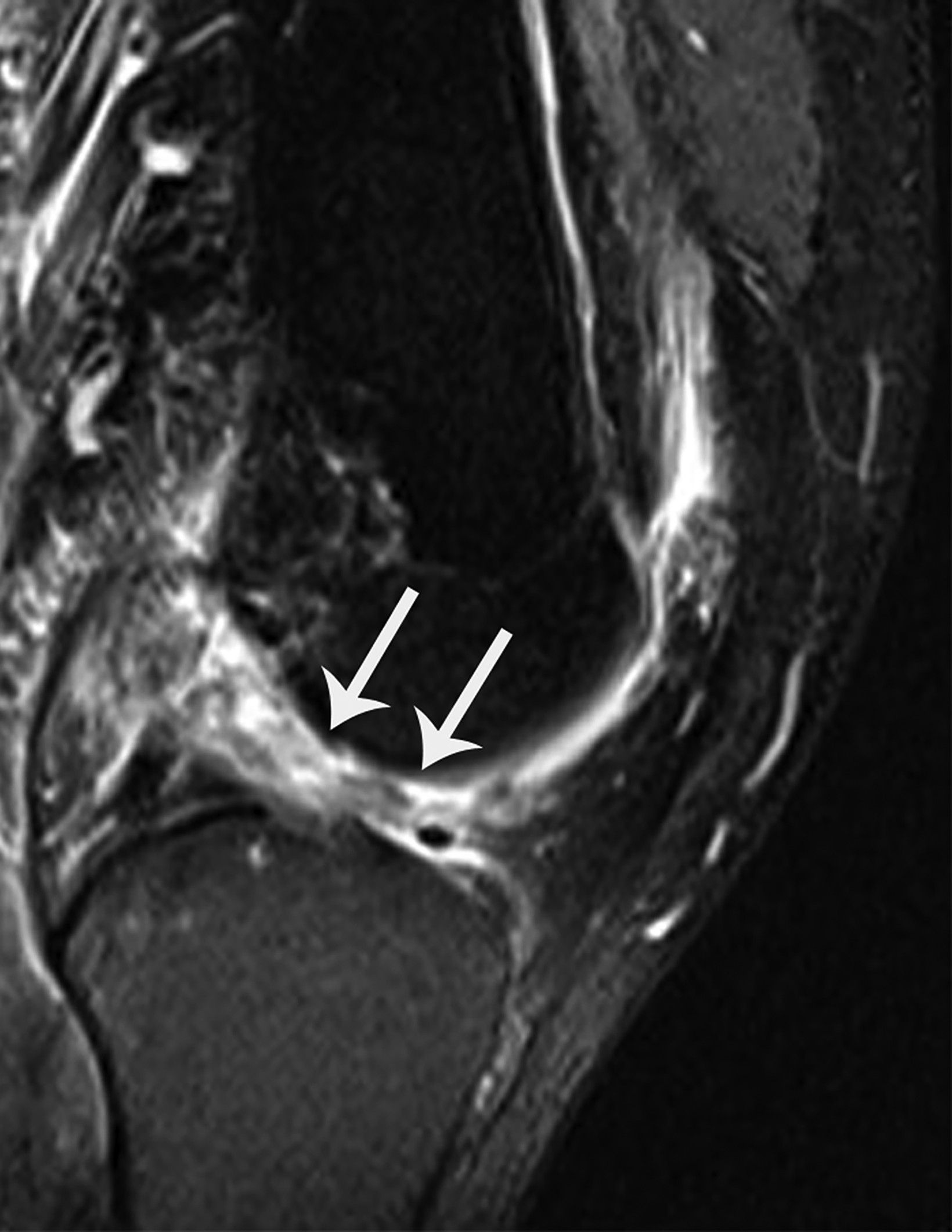
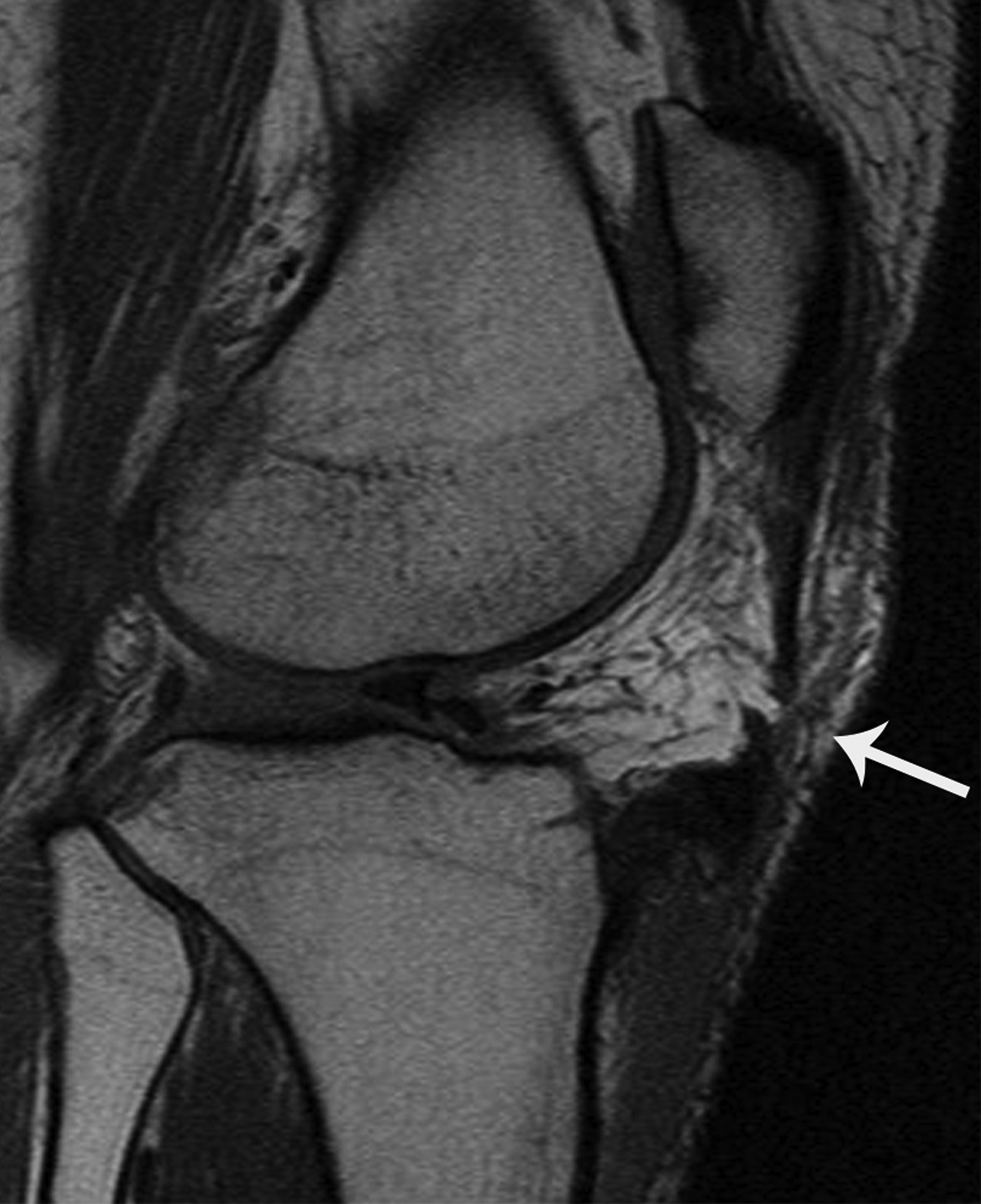
Radiographic diagnosis of TPD may be challenging, since most spontaneously reduce prior to imaging. A high clinical suspicion and correlation with clinical history increase the probability of diagnosing this abnormality. Detecting an osseous fragment in the suprapatellar joint space may provide the only perceptible clue (Figure 6). Most cases often present with a nonspecific joint effusion.30 MRI evaluation can “rule in” TPD, since the modality allows for identification of the classic “kissing contusion” bone marrow edema pattern located at the medial patellar pole and lateral femoral condyle (Figure 6). Corrective surgery to address predisposing ligamentous and osseous abnormalities is performed in knees deemed unstable.28,31
Miscellaneous Worrisome Mimics
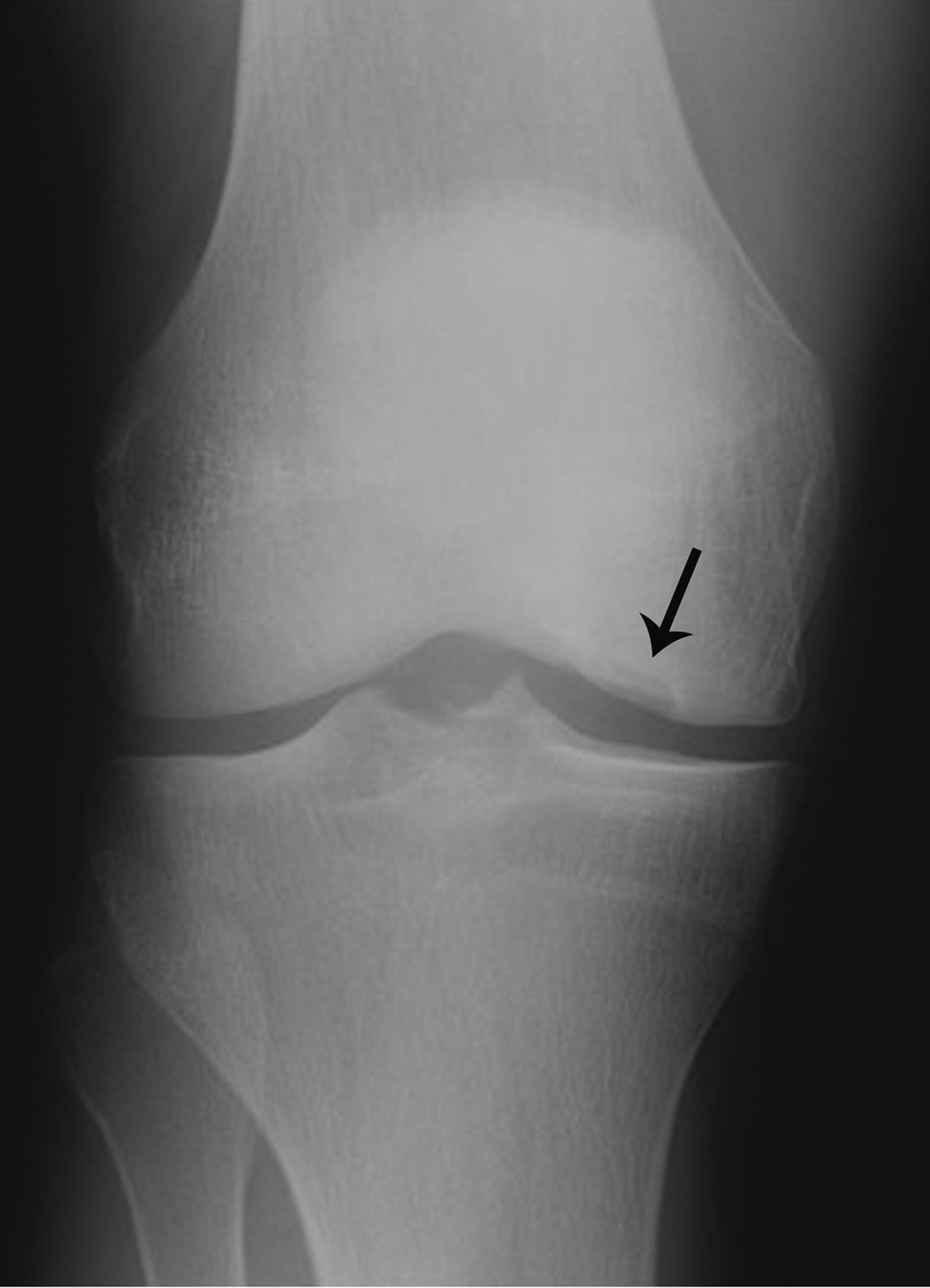
Osteochondritis dissecans
Osteochondritis dissecans (OD) is a chronic disease of subchondral bone that can mimic signs of fracture on knee radiographs, most commonly in the lateral region of the medial femoral condyle. Adolescents and young adults are the most likely to manifest OD, often presenting with knee pain, swelling, and locking.32 Identifying advanced-stage OD before the in-situ bone fragment dis- places into the joint space improves long-term prognosis.
Radiographic findings of advanced OD with an in-situ fragment demonstrates an ossific fragment at the articular surface, separated from the adjacent bone by a curvilinear lucency (Figure 7). Its location at the lateral region of the medial femoral condyle and relative smooth margins of the curvilinear lucency help to differentiate OD from an acute fracture. MRI can confirm the diagnosis and provide staging information critical for treatment. Patients with unstable in-situ fragments are candidates for surgery.32,33
Incidental Signs
Degenerative Joint Disease
Geode
A geode is a subchondral cyst typically associated with full-thickness articular cartilage loss. Geodes are not true “cysts” but instead represent cyst-like changes. Most cases do not represent a diagnostic dilemma for the radiologist, since they typically present with other findings related to osteoarthritis — including osteophytes, joint space loss, and/or subchondral sclerosis.34-36 Symptomatic patients often present with complaints emblematic of osteoarthritis — knee pain, stiffness, and swelling, among others.
However, geodes presenting on radiographs in isolation without other definitive signs of osteoarthritis may be confused with more worrisome diagnoses such as malignancy.
Radiography demonstrates geodes as classically round, well-defined, lytic lesions with a thin, sclerotic, narrow zone of transition at an articular surface (Figure 8). Their location at the subchondral bone of an articular surface and appearance should allow for confident radiographic diagnosis of a benign, degenerative geode requiring no additional follow-up.
Central Osteophyte
Osteoarthritis is commonly diagnosed in patients who present clinically with variable complaints of knee pain, swelling, locking, and stiffness. The osteophyte is a basic feature in establishing the radiographic diagnosis, with osteophyte formation typically occurring at the joint margins. The precise pathogenesis of osteophytes is still unclear but is thought to represent a response to altered biomechanics.37 Osteophytes that occur at the center, rather than at the margin, of the joint are much less common.38,39 Radiologists should not confuse central osteophytes with truly worrisome bone conditions.
On radiographs central osteophytes appear as well-defined focal osseous protuberances in continuity with the subchondral bone at the articular surface (Figure 9). Associated signs of osteoarthritis – marginal osteophytes, joint-space narrowing, and/or geodes — should increase diagnostic confidence for a degenerative central osteophyte requiring no additional work up.
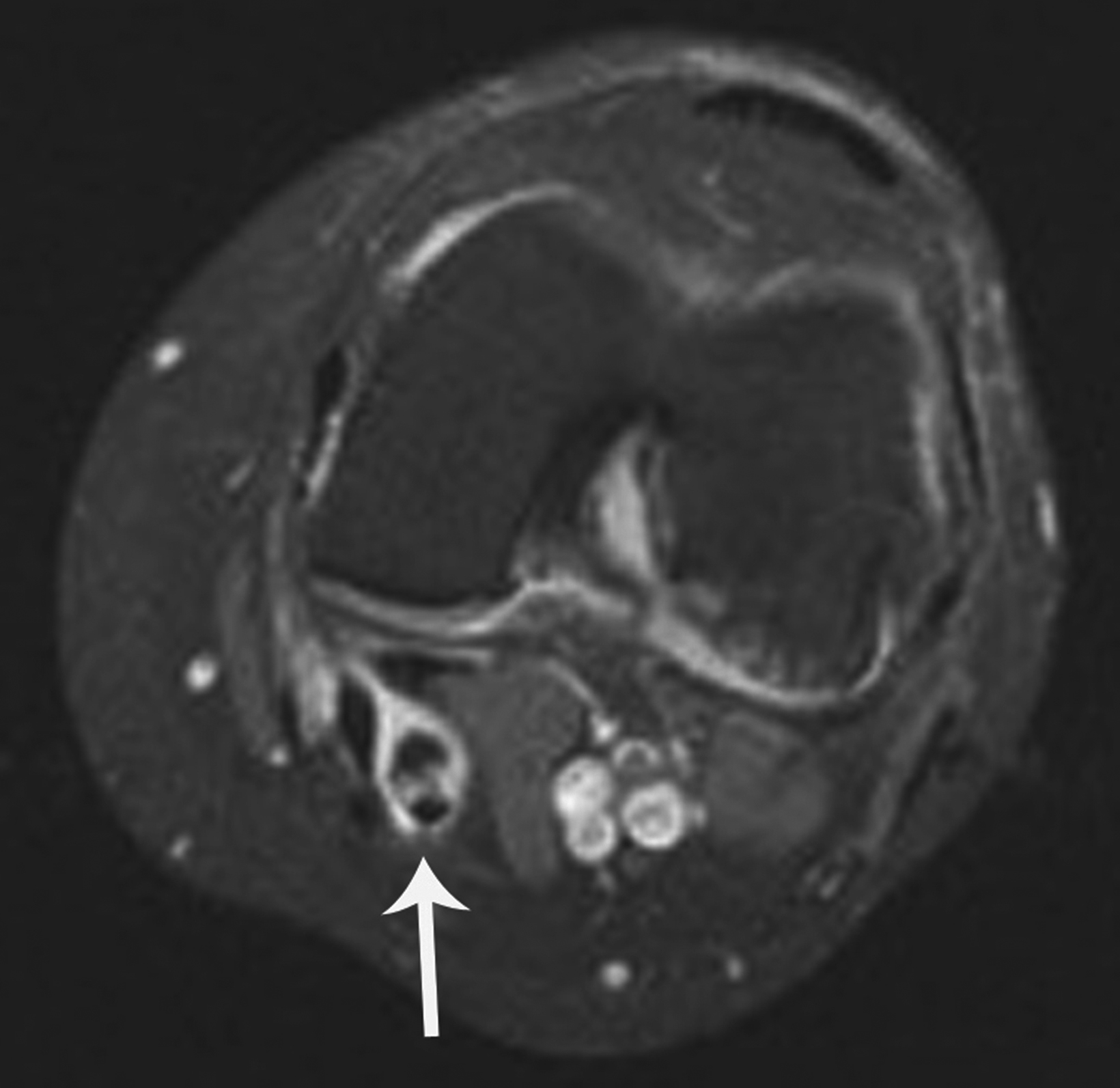
Baker Cyst Osteochondral Body
Degenerative intra-articular osteochondral bodies (“loose bodies”) are a well-known condition in patients with knee osteoarthritis. On radiographs, a mineralized mass centered in the soft tissues rather than in the knee joint raises potential suspicion for malignancy. Baker cysts are synovial cysts created by a region of the posterior knee joint capsule that anatomically has displaced in a posterior direction between the semimembranosus and medial head of the gastrocnemius tendons. Typically, joint contents travel into the Baker cyst through a mechanism resembling a one-way valve.35 Displaced osteochondral bodies, and even meniscal fragments, are known to collect in Baker cysts.
Radiographically, single or multiple well-defined osteochondral bodies appear as one or more mineralized masses in the soft tissues behind the knee (Figure 10). Identifying additional findings associated with osteoarthritis — osteophytes, joint space loss, geodes, and/or subchondral sclerosis — should allow more confident diagnosis of degenerative osteochondral bodies in a Baker cyst without the need for follow up. Radiographs that lack any other signs of osteoarthritis, have an ill-defined or stippled pattern of mineralization, or show an unexplained mineralized soft-tissue mass in a location not consistent with a Baker cyst should undergo cross-sectional imaging to exclude malignancy or other worrisome conditions.35,40
Miscellaneous (Incidental)
Multi-partite Patella
Developmental anomalies of the patella are common. The patella is the largest sesamoid bone in the body with variable fusion patterns of secondary ossification centers. The most common location is the superolateral pole.41,42 Particularly in the setting of trauma, multi-partite patella can create diagnostic uncertainty on radiographs by mimicking the appearance of acute fracture.
Multi-partite patella can be differentiated from a comminuted fracture by identifying two or more smooth, well-defined, and non-united round or ovoid secondary ossification centers located at the superolateral pole and separated from each other and the larger patellar body by well-defined curvilinear lucencies (Figure 11).41-43 In the absence of associated bony tenderness with direct palpation at the site of a classically-appearing multi-partite patella on physical examination, no follow up is necessary.
Conclusion
Knee radiography is common in daily clinical practice. Knowledge of worrisome signs related to difficult-to-detect traumatic knee pathology informs radiologists when to expeditiously recommend additional imaging and/or clinical evaluation.
Familiarity with less-common incidental signs of degenerative joint disease and developmental anomaly allow for definitive diagnosis and confidence that no further evaluation is required.
References
- Kim YW, Mansfield LT. Fool me twice: delayed diagnoses in radiology with emphasis on perpetuated errors. AJR Am J Roentgenol. 2014;202(3):465-470.
- Fileni A, Fileni G, Mirk P, Magnavita G, Nicoli M, Magnavita N. Malpractice claims related to musculoskeletal imaging. Incidence and anatomical location of lesions. Radiol Med. 2013;118(8):1388-1396.
- Lo LY, Faddoul D, Almardawi R, Davis DL. Quality of Clinical History for Musculoskeletal Radiographs at Outpatient Imaging Centers: One Institution’s Expe- rience. Colu J Cas Repo. 2021; 2:18. https://columbuspublishers.com/uploads/reviews/CJCR-2021-18.pdf. Accessed May 27, 2022.
- Expert Panel on Musculoskeletal Imaging; Fox MG, Chang EY, et al. ACR Appropriateness Criteria(R) Chronic Knee Pain. J Am Coll Radiol. 2018;15(11S):S302-S312.
- Expert Panel on Musculoskeletal Imaging; Taljanovic MS, Chang EY, et al. ACR Appropriateness Criteria(R) Acute Trauma to the Knee. J Am Coll Radiol. 2020;17(5S):S12-S25.
- Davis DL, Vachhani P. Traumatic Extra-capsular and Intra-capsular Floating Fat: Fat-fluid Levels of the Knee Revisited. J Clin Imaging Sci. 2015;5:60.
- Beckett R, Le P, Rheinboldt M, Petraszko A. Avulsion fractures of the knee: a review of the pathophysiology, radiographic, and cross-sectional imaging features. Emer Radiol. 2019;26(6):683-689.
- Campos JC, Chung CB, Lektrakul N, et al. Pathogenesis of the Segond fracture: anatomic and MR imaging evidence of an iliotibial tract or anterior oblique band avulsion. Radiology. 2001;219(2):381-386.
- Goldman AB, Pavlov H, Rubenstein D. The Segond fracture of the proximal tibia: a small avulsion that reflects major ligamentous damage. AJR Am J Roentgenol. 1988;151(6):1163-1167.
- Slagstad I, Parkar AP, Strand T, Inderhaug E. Incidence and Prognostic Significance of the Segond Fracture in Patients Undergoing Anterior Cruciate Ligament Reconstruction. Am J Sports Med. 2020;48(5):1063-1068.
- Edmonds EW, Fornari ED, Dashe J, Roocroft JH, King MM, Pennock AT. Results of Displaced Pediatric Tibial Spine Fractures: A Comparison Between Open, Arthroscopic, and Closed Management. J Pediatr Orthop. 2015;35(7):651-656.
- Nichols JN, Tehranzadeh J. A review of tibial spine fractures in bicycle injury. Am J Sports Med. 1987;15(2):172-174.
- Kim ME, Stead TS, Ganti L. Compartment Syndrome Secondary to Knee Lipohemarthrosis. Cureus. 2021;13(8):e16946.
- Colletti P, Greenberg H, Terk MR. MR findings in patients with acute tibial plateau fractures. Comput Med Imaging Graph. 1996;20(5):389-394.
- Lee JH, Weissman BN, Nikpoor N, Aliabadi P, Sosman JL. Lipohemarthrosis of the knee: a review of recent experiences. Radiology. 1989;173(1):189-191.
- Ryu KN, Jaovisidha S, De Maeseneer M, Jacobson J, Sartoris DJ, Resnick D. Evolving stages of lipohemarthrosis of the knee. Sequential magnetic resonance imaging findings in cadavers with clinical correlation. Invest Radiol. 1997;32(1):7-11.
- Le Corroller T, Parratte S, Zink JV, Argenson JN, Champsaur P. Floating fat in the wrist joint and in the tendon sheaths. Skeletal Radiol. 2010;39(9):931-933.
- Chiu SS. The anterior tibial translocation sign. Radiology. 2006;239(3):914-915.
- Dienst M, Burks RT, Greis PE. Anatomy and biomechanics of the anterior cruciate ligament. Orthop Clin North Am. 2002;33(4):605-620.
- Frank JM, Moatshe G, Brady AW, et al. Lateral Meniscus Posterior Root and Meniscofemoral Ligaments as Stabilizing Structures in the ACL-Deficient Knee: A Biomechanical Study. Orthop J Sports Med. 2017;5(6):2325967117695756.
- Logerstedt DS, Snyder-Mackler L, Ritter RC, Axe MJ, Godges JJ, Orthopaedic Section of the American Physical Therapist A. Knee stability and movement coordination impairments: knee ligament sprain. J Orthop Sports Phys Ther. 2010;40(4):A1-A37.
- Ali SA, Helmer R, Terk MR. Patella alta: lack of correlation between patellotrochlear cartilage congruence and commonly used patellar height ratios. AJR Am J Roentgenol. 2009;193(5):1361-1366.
- Steele R, Hayden SR, Ward N, Macias M. Patellar Tendon Rupture Bedside Diagnosis. J Emerg Med. 2021;60(3):384-386.
- Kannus PA. Long patellar tendon: radiographic sign of patellofemoral pain syndrome—a prospective study. Radiology. 1992;185(3):859-863.
- Insall J, Goldberg V, Salvati E. Recurrent dislocation and the high-riding patella. Clin Orthop Relat Res. 1972;88:67-69.
- Insall J, Salvati E. Patella position in the normal knee joint. Radiology. 1971;101(1):101-104.
- Core M, Anract P, Raffin J, Biau DJ. Traumatic Patellar Tendon Rupture Repair Using Synthetic Ligament Augmentation. J Knee Surg. 2020;33(8):804-809.
- Earhart C, Patel DB, White EA, Gottsegen CJ, Forrester DM, Matcuk GR, Jr. Transient lateral patellar dislocation: review of imaging findings, patellofemoral anatomy, and treatment options. Emerg Radiol. 2013;20(1):11-23.
- Senavongse W, Amis AA. The effects of articular, retinacular, or muscular deficiencies on patellofemoral joint stability: a biomechanical study in vitro. J Bone Joint Surg Br. 2005;87(4):577-582.
- Haas JP, Collins MS, Stuart MJ. The “sliver sign”: a specific radiographic sign of acute lateral patellar dislocation. Skeletal Radiol. 2012;41(5):595-601.
- Purohit N, Hancock N, Saifuddin A. Surgical management of patellofemoral instability. I. Imaging considerations. Skeletal Radiol. 2019;48(6):859-869.
- Accadbled F, Vial J, Sales de Gauzy J. Osteochondritis dissecans of the knee. Orthop Traumatol Surg Res. 2018;104(1S):S97-S105.
- Matthews JR, Sonnier JH, Paul RW, et al. A systematic review of cartilage procedures for unstable osteochondritis dissecans. Phys Sportsmed. 2022:1-9.
- Pouders C, De Maeseneer M, Van Roy P, Gielen J, Goossens A, Shahabpour M. Prevalence and MRI-anatomic correlation of bone cysts in osteoarthritic knees. AJR Am J Roentgenol. 2008;190(1):17-21.
- Perdikakis E, Skiadas V. MRI characteristics of cysts and “cyst-like” lesions in and around the knee: what the radiologist needs to know. Insights Imaging. 2013;4(3):257-272.
- Zeng GJ, Foong WS, Lie TTD. Knee subchondroplasty for management of subchondral bone cysts: a novel treatment method. Singapore Med J. 2021;62(9):492-496.
- Markhardt BK, Li G, Kijowski R. The Clinical Significance of Osteophytes in Compartments of the Knee Joint With Normal Articular Cartilage. AJR Am J Roentgenol. 2018;210(4):W164-W171.
- McCauley TR, Kornaat PR, Jee WH. Central osteophytes in the knee: prevalence and association with cartilage defects on MR imaging. AJR Am J Roentgenol. 2001;176(2):359-364.
- Kretzschmar M, Heilmeier U, Foreman SC, et al. Central osteophytes develop in cartilage with abnormal structure and composition: data from the Osteoarthritis Initiative cohort. Skeletal Radiol. 2019;48(9):1357-1365.
- Dhillon M, Prasad P, Goel A, Kar A. Giant osteochondral body in a popliteal cyst. Indian J Orthop. 2009;43(1):93-96.
- Faizan M, Jilani LZ, Bin Sabir A, Abbas M. Unusual cause of anterior knee pain. Saudi Med J. 2016;37(8):910-912.
- Oohashi Y, Koshino T, Oohashi Y. Clinical features and classification of bipartite or tripartite patella. Knee Surg Sports Traumatol Arthrosc. 2010;18(11):1465-1469.
- Ozdemir ZM, Gormeli CA, Kahraman AS, Demirtas G, Gormeli G. Unusual Symptomatic Multipartite Patella Associated with Quadriceps Fat Pad Edema. J Belg Soc Radiol. 2016;100(1):49.
Citation
K K, G M, M W, DL D. Worrisome and Incidental Signs on Knee Radiographs in Clinical Practice: Traumatic and Degenerative Lesions. Appl Radiol. 2023;(1):8-16.
February 1, 2023