Tumoral Calcinosis
Images


CASE SUMMARY
A 10-year-old African-American female was admitted to the hospital with a palpable soft-tissue mass posterior to the elbow joint with no history of trauma. Diagnostic imaging included: elbow radiography and elbow MRI. A percutaneous biopsy was performed to confirm diagnosis.
IMAGING FINDINGS
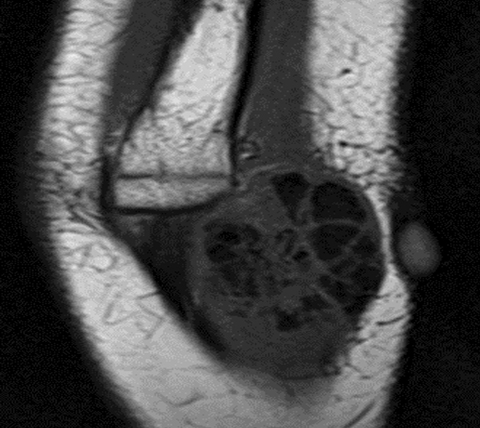
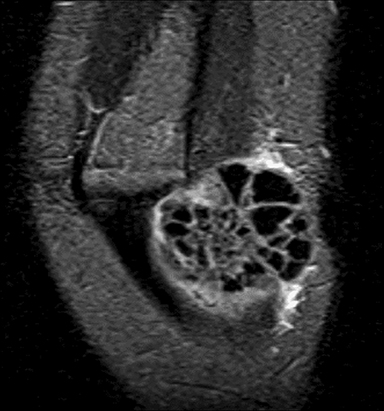
Lateral radiograph of the elbow shows a soft-tissue mass juxtaposed to the posterior aspect of the distal humerus (Figure 1). The lesion is composed of amorphous and multi-lobulated calcification without bone destruction. Coronal T1- and T2-weighted MRI sequences (Figure 2) show an extra-articular soft tissue lesion with smooth margins.1 T1-weighted sequence shows predominantly heterogeneous low signal intensity, while the T2-weighted sequence shows a heterogeneous mixed intensity lesion. Ultrasound (Figure 3) shows a well-circumscribed echogenic mass splaying soft tissues planes.
DIAGNOSIS
Tumoral calcinosis.
The differential diagnosis of soft tissue calcification without bone destruction includes myositis ossificans, metabolic calcification and dystrophic calcification often secondary to trauma, parasitic infection, and autoimmune (dermatomyositis, scleroderma) conditions.
DISCUSSION
Tumoral calcinosis is caused by abnormal phosphate regulation associated with massive peri-articular calcinosis.1 This is a rare, inherited condition, usually found in African-American females and commonly presenting in childhood or early adolescence.2 Tumoral calcinosis is most often seen in the soft tissues around the hip, shoulder, and elbow, but it has been found localized to the foot, wrist, and knee.2
Most patients with tumoral calcinosis present with swelling, lumps, or masses near or around a joint, sometimes followed by tenderness or pain. Radiography will demonstrate a cloud-like soft-tissue mass. Computed tomography or MRI may also be useful to assess for associated bone or joint changes.2 The lack of bone or joint involvement supports the diagnosis of tumoral calcinosis. Laboratory tests and histology may also be performed to assess renal and parathyroid function, as well as test calcium, phosphorus, uric acid, and alkaline phosphate levels. If percutaneous aspiration is performed, the specimen is usually whitish in color and the consistency of toothpaste as in this case. Histologic analysis will demonstrate calcium phosphate, calcium carbonate, or calcium hydroxyapatite.1
The other primary diagnostic consideration is myositis ossificans, which presents as a secondary soft-tissue mass from injury, cerebrospinal disorder, or burn. Location is commonly within muscle, but can also form around ligaments, tendons, and joint capsules. The composition of these masses is of heterotopic bone and cartilage.4 Diagnosis includes plain radiography to reveal calcification in as early as 2 weeks, with circumscribed ossification presenting at 6 or more weeks after injury as calcification evolves into cartilage and bone.
Several other diseases mimic the radiological features of tumoral calcinosis due to their size, distribution, and morphology, making diagnosis of tumoral calcinosis from imaging alone very difficult. Metabolic calcification presents with mineral deposits in visceral organs, resulting in abnormal calcium and/or phosphate levels. Dystrophic calcification is a reaction to tissue damage and is associated with normal serum chemistry levels. Calcium deposition can be local or general. Since children with dystrophic calcification have normal serum chemistry levels, antibody screening may be performed if a rheumatologic disease is suspected.
Treating tumoral calcinosis depends on the lesion’s site and size, as well as the presenting symptoms. The most common treatment is surgical excision; however, there is a high rate of recurrence.3 Overall prognosis of this disease is very good, with a mortality rate of zero.
CONCLUSION
Tumoral calcinosis is a hereditary condition typically seen in young African American females during childhood or early adolescence. Though a well understood condition, it can be easily mistaken for another lesion or disease. In addition, diagnosis is difficult with imaging alone. Tumor calcinosis is typically located within the soft tissues around joints like the hip, shoulder, or elbow due to abnormal phosphate and calcium levels in the body. Commonly, patients present with little to no pain, and treatment consists of surgical removal.
REFERENCES
- Gaillard F and Weerakkody Y. Tumoral calcinosis. 2018 Accessed July 5, 2018, from https://radiopaedia.org/articles/tumoral-calcinosis.
- Woon, C. Tumoral calcinosis. Accessed July 3, 2018, from https://www.orthobullets.com/pathology/8077/tumoral-calcinosis.
- Fathi I and Sakr M. Review of Tumoral Calcinosis: A Rare Clinico-Pathological Entity. 2014. Accessed July 5, 2018, from https://www.ncbi.nlm.gov/pmc/articles/PMC4163761/.
Citation
A A, D A, C S, R K, SA J, T A, R T. Tumoral Calcinosis. Appl Radiol. 2020;(2):48A-48C.
March 17, 2020