Review of inguinal region hernias on MDCT: A vascular roadmap
Images









Dr. Abdeen is a Radiologist at Children’s Hospital of Eastern Ontario, Ottawa, Ontario, Canada, and Dr. Shabana is a Radiologist in the Department of Diagnostic Imaging at the University of Ottawa, Ottawa, Canada.
The cross-sectional imaging of inguinal hernias poses a challenge to inexperienced observers due to the complex anatomy of the region. A hernia occurs as bulging of visceral content through a weak point in the abdominal wall. These weak points could be natural, anatomic,congenital, or iatrogenic — such as an incisional hernia. Inguinal and femoral hernias are common, with a lifetime prevalence of 5% or more in the general population. Inguinal hernias constitute approximately 75% of all hernias, of which two-thirds are indirect and one-third are direct. Femoral hernias comprise 3% of hernias with a 10:1 female to male ratio.1 Although both types may incarcerate and strangulate, the risk is higher for femoral (20%-25%) than for inguinal hernias (3%). Accurate radiologic diagnosis is therefore important.
Sonography can effectively differentiate between various groin hernias.2 While free of ionizing radiation, its use is operator dependent.Computed tomography (CT) is often the first line modality as many hernias may present as bowel obstruction or with nonspecific abdominal pain, particularly in the elderly. Thinly collimated multidetector CT (MDCT) with coronal and sagittal reformats have recently been reported to visualize the inguinal ligament and associated structures with a higher accuracy than in thickly collimated axial images.3 MDCT findings distinguishing between femoral and inguinal hernias have also been described.4,5
A comprehensive, easily applied approach to the differential diagnosis of groin hernias is required. The vascular anatomy of the groin, particularly the inferior epigastric and femoral vessels, provides a helpful guide. Here, we present a “vascular roadmap” approach to groin hernias incorporating these findings.
Inguinal anatomy
The inguinal region comprises the inguinal canal and the femoral triangle.6
Inguinal canal
The inguinal canal extends between the deep inguinal ring (defect in the transversalis fascia) and superficial inguinal ring (triangular defect in the medial portion of the external oblique aponeurosis). It contains the spermatic cord in males and the round ligament in females.7
The anterior wall is formed by the aponeurosis of the external oblique muscle. The floor of the inguinal canal is formed by the inguinal ligament (inferior edge of the external oblique aponeurosis, which attaches at the anterior superior iliac spine and the pubic tubercle) and its extension, the lacunar ligament. The superior border is formed by the internal oblique and transversus abdominis aponeuroses. The transversalis fascia and transverses abdominis aponeurosis form the posterior border.1
Several named tendons lie in the inguinal region. Cooper’s ligament, or the pectineal ligament, is formed from the fascia and periosteum along the superior pubic ramus.1 The conjoint tendon is formed by the fusion of the transversus abdominis aponeurosis with the internal oblique.
Femoral triangle
The femoral triangle is bounded superiorly by the inguinal ligament, medially by the adductor longus, laterally by the sartorius, and posteriorly by the iliopsoas, pectineus and adductor longus muscles. From lateral to medial, the femoral triangle contains the femoral nerve, artery, and vein. The femoral canal is the potential space medial to the femoral vein, which contains connective tissue and a small amount of fat tissue, through which femoral hernias pass. The femoral ring is that portion of the femoral canal bounded laterally by the femoral vein,medially by the lacunar ligament, anteriorly by the inguinal ligament, and posteriorly by the pectineal ligament. The latter 3 structures are relatively noncompressible, and any hernia passing through the ring will, therefore, preferentially compress the femoral vein.
Vascular landmarks
The inferior epigastric artery
The inferior epigastric artery (IEA) is an important landmark with respect to hernia localization. The IEA originates from the external iliac artery and lies immediately medial to the deep inguinal ring (Figure 1). It is therefore the radiologic landmark to identify indirect inguinal hernias, which pass through the internal inguinal ring with the hernia neck lateral to the artery. The IEA ascends medially to lie deep in the ipsilateral rectus abdominis muscle.
The IEA forms the superolateral border of Hesselbach’s triangle with the rectus abdominis and the inguinal ligament forming the medialand inferior borders respectively (Figure 1). Direct inguinal hernias occur in Hesselbach’s triangle, and therefore, the hernia neck lies medialto the IEA.
Femoral vessels
The femoral artery and vein are easily identified distal to the inguinal ligament as continuations of the external iliac vessels (Figure 1). The pubic tubercle is a useful marker for the inguinal ligament, which is often not identified on axial images.3,8 Femoral hernias occupy the femoral ring lateral to the tough lacunar ligament and medialto the soft femoral vein (Figure 1). A decrease in the venous diameter by two-thirds relative to the contralateral side has been shown to be a reliable indicator of femoral hernia.4
The deep circumflex iliac artery
The deep circumflex iliac artery arises from the lateral external iliac artery nearly opposite to the IEA, for which it is a good landmark. It
passes superolaterally towards the anterior superior iliac spine.
Groin hernias
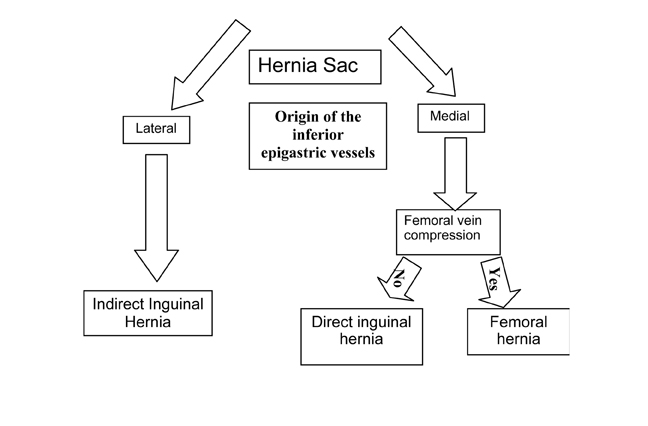
The vascular roadmap depends on two crucial vessels, namely the inferior epigastric artery and the femoral vein. A 3-step algorithm related to the IEA and femoral vein can simplify the diagnosis of groin hernias in most cases:
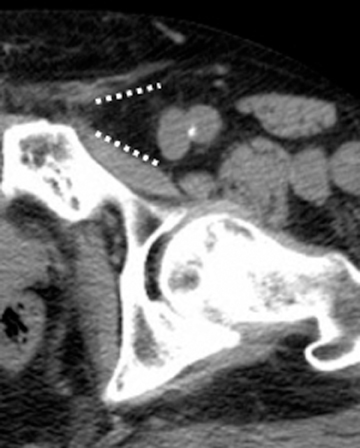
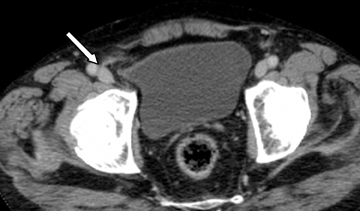
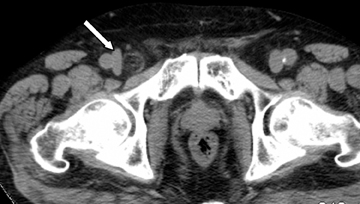
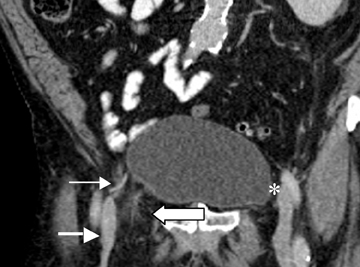
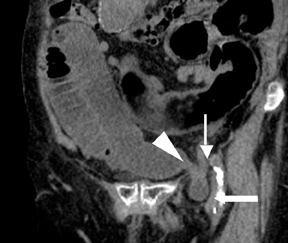
Step 1: If the hernia sac is located lateral to the origin of the inferior epigastric artery and vein, it is an indirect inguinal hernia (Figures 2-4).
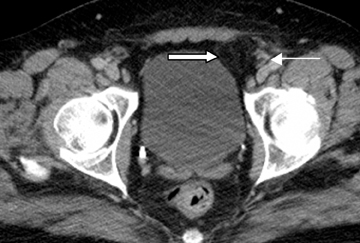
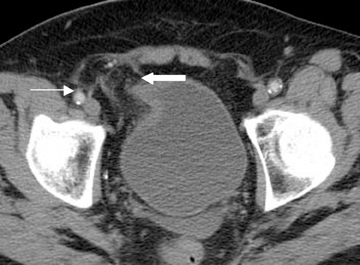
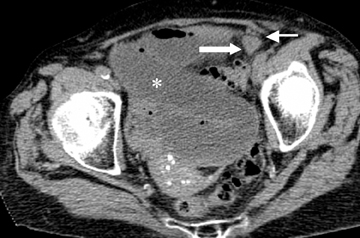
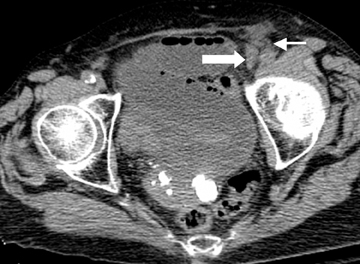
Step 2: If the hernia sac is located medial to the origin of the IEA, the femoral vein should be assessed. If the femoral vein is compressed by the hernia sac, a femoral hernia is present. If the femoral vein is not compressed, a direct inguinal hernia is expected. (Figures 2 and 5).
Step 3: Compression of the femoral vein, including an elliptic femoral vein with the short axis diameter measuring less than two-thirds the diameter of the contralateral femoral vein and oriented in the direction of the hernia sac,4 indicates a femoral hernia (Figures 2, 6-8). Femoral vein compression may be lacking in a small or Richter’s type femoral hernia.
While a large inguinal hernia could theoretically exert a mass effect on the femoral vein, the authors think this is unlikely, as the femoral ring is bounded by the relatively noncompliant inguinal and lacunar ligaments. Furthermore, indirect and direct inguinal hernias occur in amore anterior plane than do femoral hernias.
The advantage to this algorithm is that it can be applied to axial and unenhanced CT images. Coronal reformats are useful, and contrast makes the vascular structures more evident, but neither is essential. Identification of the inferior epigastric vein and artery on axial images is easier when the vessels are identified deep to the rectus abdominis above the pelvis and followed caudally to their origin from the external iliac vessels. A subsidiary clue to the location is the deep circumflex iliac artery, which originates from the external iliac artery on the lateral side at about the same level as the medial origin of the IEA.
Conclusion
The use of a vascular roadmap and a 3-step algorithm using the IEA and the femoral vein provides rapid and accurate diagnosis of femoral and inguinal hernias on MDCT (Figure 9). The method enables accurate diagnosis on axial images and applies equally to contrast and nonenhanced CT.
References
- Malangoni MA, Rosen MJ. Hernias. In: Townsend CM, Beauchamp RD, Evers BM,
- Mattox KL, eds. Sabiston Textbook of Surgery. Pa: Saunders Elsevier; 2008:chap 44.
- Jamadar DA, Jacobson JA, Morag Y, et al. Sonography of inguinal region hernias. AJR Am J Roentgenol. 2006;187:185-190.
- Cherian PT, Parnell AP. Radiologic anatomy of the inguinofemoral region: Insights from MDCT. AJR Am J Roentgenol. 2007;189:W177-183.
- Suzuki S, Furui S, Okinaga K, Sakamoto T, et al. Differentiation of femoral versus inguinal hernia: CT findings. AJR Am J Roentgenol. 2007;189:W78-83.
- Cherian PT, Parnell AP. The diagnosis and classification of inguinal and femoral hernia on multisection spiral CT. Clin Radiol. 2008;63:184-192.
- Shadbolt CL, Heinze SBJ, Dietrich RB. Imaging of groin masses: Inguinal anatomy and pathological conditions revisited. Radiographics. 2001;21:S261-S271.
- Van den Berg JC, De Valois JC, Go PM, Rosenbusch G. Radiological anatomy of the groin region. Eur Radiol. 2000;10:661-670.
- Delabrousse E, Denue PO, Aubry S, et al. The pubic tubercle: CT landmark in groin hernia. Abdom Imaging. 2007;32:803-806.