PET Scans of Heart May Identify People at Risk for Parkinson Disease and Lewy Body Dementia
Images
Researchers at the National Institutes of Health have found that positron emission tomography (PET) scans of the heart may identify people who will go on to develop Parkinson disease or Lewy body dementia among those at-risk for these diseases. The findings of the small study, published in the Journal of Clinical Investigation and led by scientists at the National Institute of Neurological Disorders and Stroke (NINDS), part of NIH, may advance efforts to detect the earliest changes that years later lead to Parkinson disease and Lewy body dementia.
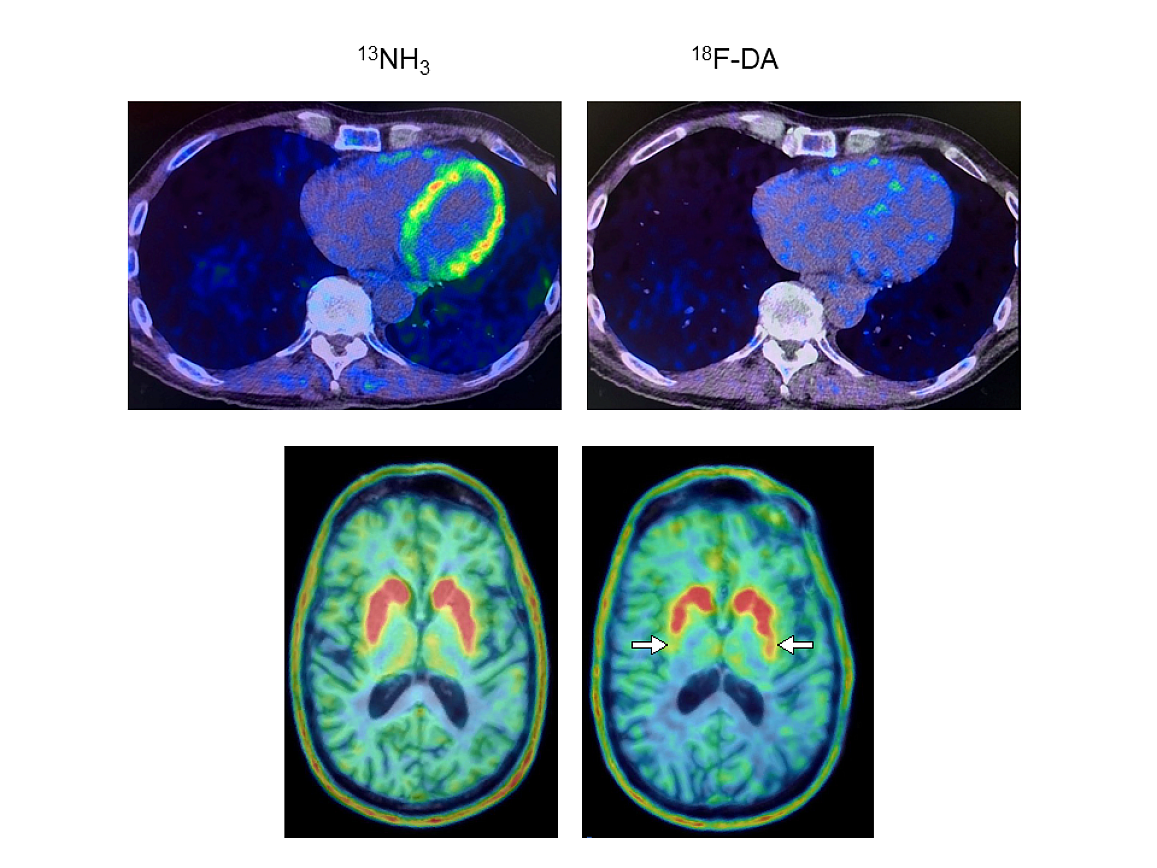
In 34 people with Parkinson disease risk factors, researchers conducted PET scans of the heart to gain insight into levels of the neurotransmitter norepinephrine. They found that the scans could distinguish individuals who would later be diagnosed with Parkinson or Lewy body dementia—both are brain diseases caused by abnormal deposits of the protein alpha-synuclein that form clumps known as Lewy bodies. The research was conducted at the NIH Clinical Center, currently the only location for 18F-dopamine PET scanning.
Norepinephrine is derived from dopamine, which is deficient in the brains of people with Parkinson’s disease. Earlier work from David S Goldstein, MD, PhD, NINDS Principal Investigator, demonstrated that people with Lewy body diseases had severe depletion of cardiac norepinephrine, which is normally released by the nerves that supply the heart.
In the present study, the research team led by Dr Goldstein found that at-risk individuals with low 18F-dopamine-derived radioactivity in the heart were highly likely to develop Parkinson or Lewy body dementia during long-term follow-up, compared to individuals with the same risk factors but with normal radioactivity. PET scans work by using a radioactive tracer to visualize metabolic or biochemical processes in body organs.
“Imagine the scans are frames of a movie,” Dr Goldstein said. “The frame at 8 minutes during the first evaluation is already enough to identify the people who are likely to go on to develop a central Lewy body disease years later.”
In the study, 34 people at risk for Parkinson had cardiac F-dopamine PET scans every 18 months for up to about 7.5 years or until they were diagnosed with the disease. Participants had three or more Parkinson risk factors, which included a family history of the disease; loss of sense of smell, which occurs commonly in Parkinson; a sleep disorder in which people act out their dreams, known as dream enactment behavior; and symptoms of orthostatic intolerance, such as light-headedness upon standing.
Of the nine individuals with low cardiac F-dopamine-derived radioactivity at their first scan, eight were diagnosed later with Parkinson or Lewy body dementia. Only 1 of 11 participants with normal initial radioactivity developed a central Lewy body disease. All nine participants who developed a Lewy body disease had low radioactivity before or at the time of diagnosis.
The study supports the view that synuclein disorders such as Parkinson disease and Lewy body dementia affect the nerves of the autonomic nervous system, which regulates automatic body processes like heart rate and blood pressure. Work by Dr Goldstein and others has shown synuclein aggregation occurs in nerves to the gastrointestinal organs, skin, and glands in both these disorders.
“We think that in many cases of Parkinson and dementia with Lewy bodies the disease processes don’t actually begin in the brain. Through autonomic abnormalities the processes eventually make their way to the brain,” Dr Goldstein said. “The loss of norepinephrine in the heart predicts and precedes the loss of dopamine in the brain in Lewy body diseases.”
Finding biomarkers that could help detect diseases before symptoms begin, known as the preclinical period, is critical for testing early interventions. The visible motor symptoms of Parkinson occur only after substantial damage or loss of dopamine-producing neurons in regions of the brain that control movement.
“Once symptoms begin, most of the damage has already been done,” said Dr Goldstein. “You want to be able to detect the disease early on. If you could salvage the dopamine terminals that are sick but not yet dead, then you might be able to prolong the time before the person shows symptoms.”
Using the PET scans to identify people with preclinical Lewy body diseases could enable testing of preventative approaches such as lifestyle modifications, dietary supplements, or medications.