Tau PET Imaging Predicts Alzheimer Disease-Related Cognitive Decline
Images
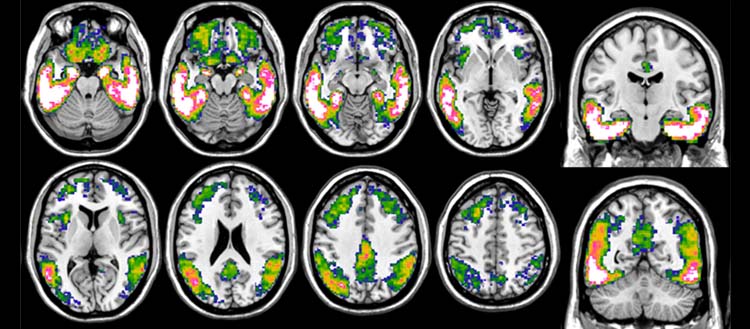
A team from the University of Geneva (UNIGE) and the Geneva University Hospitals (HUG) has demonstrated that tau PET - a novel imaging technique for visualizing the tau protein - can predict cognitive decline in patients much better than the imaging techniques normally used. These results, published in Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association, argue in favor of the rapid introduction of tau PET into the clinical routine to provide patients with early and individualized solutions.
Today, one of the main diagnostic tools for Alzheimer disease is positron emission tomography (PET), an imaging technique in which tracers are injected to visualize specific pathological processes in the brain. "PET involves injecting patients with low-level radioactive tracers that disappear within a few hours. They are designed to bind to the human molecules that we want to detect, making them visible with the PET tomographs," explains Valentina Garibotto, Associate Professor in the Department of Radiology and Medical Informatics at UNIGE Faculty of Medicine and Head Physician in the Division of Nuclear Medicine and Molecular Imaging at the HUG, who directed this research.
"Specific tracers for amyloid exist since two decades, and tracers to monitor glucose metabolism, which indicates the brain’s ability to use its energy resources correctly, have long existed. However, Alzheimer disease is complex and these two techniques are not enough to provide all the answers."
Flortaucipir is a radiotracer that binds to the tau protein. It was developed by a pharmaceutical company and approved by the Food and Drug Administration (FDA) in 2020. It allows the detection of tau accumulation as well as its distribution in the brain to precisely assess its role in the clinical manifestation of the disease. Scientists from the UNIGE and the HUG wanted to determine which imaging modality -amyloid PET, glucose metabolism PET, or tau PET - would best predict future cognitive decline due to Alzheimer disease. Around 90 participants were recruited at the HUG Memory Centre.
"Our results show that while the various PET measures were all associated with the presence of cognitive symptoms, confirming their role as strong indicators of Alzheimer disease, tau PET was the best to predict the rate of cognitive decline, even in individuals with minimal symptoms," summarizes Cecilia Boccalini, a PhD student in Professor Garibotto’s team and first author of this study.
Amyloid plaques are not necessarily accompanied by cognitive or memory loss. However, the presence of tau goes hand in hand with clinical symptoms. Its absence or presence is the main determinant of whether a patient’s condition remains stable or deteriorates rapidly. It has been more difficult to develop imaging techniques to visualize tau, mainly because of its lower concentration and particularly complex structure.
"This breakthrough is crucial for better management of Alzheimer disease. Recently, drugs targeting amyloid have shown positive results. New drugs targeting the tau protein also look promising. By detecting the pathology as early as possible, before the brain is further damaged, and thanks to new treatments, we hope to be able to make a greater impact on patients’ future and quality of life," Valentina Garibotto points out. "Similarly, we are beginning to map the distribution of tau in order to understand how its location in the different regions of the brain influences symptoms." Indeed, the causes and different stages of the disease are proving to be much less uniform than previously thought, and individual susceptibility to the same phenomena needs to be better understood.
These results are a strong argument in favor of incorporating tau PET into the routine clinical evaluation to assess individual prognosis and select the most appropriate therapeutic strategy for each patient.
Related Articles
Citation
Tau PET Imaging Predicts Alzheimer Disease-Related Cognitive Decline. Appl Radiol.
August 11, 2023