Pairing AI with Breast Density Algorithms Helps Predict Long-Term Cancer Risk
Images
Researchers from the Mayo Clinic and University of California, San Francisco report that pairing artificial intelligence (AI) imaging and volumetric breast density algorithms can assist in predicting long-term risk of breast cancer, in particular invasive disease. The study, published in the Journal of Clinical Oncology, featured the combination of Transpara Exam Score with Volpara TruDensity.
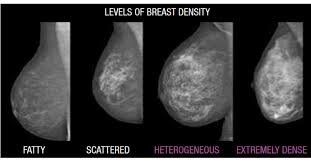
The study was designed to determine if an AI algorithm could contribute to long-term risk prediction for advanced and interval cancers. Researchers used images from 2,412 women with invasive breast cancer and 4,995 matched controls who had digital mammograms performed 2-5.5 years before cancer diagnosis. The performance of conventional assessment measures (traditional radiologist interpretation and BI-RADS® density categories) were compared to the ability of newer AI-powered techniques (precise volumetric density measures and image-based malignancy risk scores) for long-term risk prediction of advanced and interval cancers.
The research found that Transpara AI score improves long-term risk prediction when combined with clinical risk factors including breast density for overall invasive cancers, screen-detected, advanced, and nonadvanced cancers. For interval cancers, the TruDensity measures remained of greatest importance for discrimination, even years before the cancer.
The Transpara Exam Score is an image-based risk tool that categorizes exams using a 10-point scale and is used for concurrent reading of mammograms. The higher the score, the higher the risk of cancer in the mammogram. Clinical research conducted with Transpara shows that scores between 1 - 7 (Low Risk) have a 99.97% negative predictive value. The Volpara TruDensity AI algorithm uses a combination of x-ray physics and machine learning to generate an accurate volumetric measure of breast composition to eliminate variability that can arise from human interpretation.
"While we have known for decades that density and breast cancer risk are correlated, recent research has really pushed forward our ability to better understand the effects of density combined with image-based risk to drive personalized medicine for women," said Professor Nico Karssemeijer, PhD, Chief Scientific Officer at Screenpoint Medical, and faculty member at Radboud University.
"Breast density is a critical factor in assessing breast cancer risk, and an objective, volumetric measurement of density is pivotal. Through the power of AI, we can uncover valuable insights that help clinicians identify individuals at risk for cancer and tailor personalized screening and prevention strategies," said Ralph Highnam, PhD, Chief Science and Innovation Officer, Volpara Health.
Volpara's software is used to assess breast density for more than 6 million women annually. TruDensity is proven to reduce reader variability. Radiologists agree with Volpara's assessment of non-dense (a or b) or dense (c or d) 96% of the time.
"Early identification of image-based risk can give a more effective screening and care pathway for high-risk women. This approach should not only save lives but enable women to experience the least disruption in their lives when care is required. Screening today requires this type of focused, personalized approach. We hope that the work we are doing empowers women and their providers to deliver the right care in the right way at the right times," added Prof Karssemeijer.