Ollier Disease
Images


Case Summary
A child with no prior medical history presented for orthopedic evaluation after developing an increasing number of painless bumps over the right hand. The patient’s signs began with a single bump on the right fourth digit middle phalanx. The bumps did not affect range of motion. Focused exam of the right hand revealed palpable, nontender, osseous nodules involving the proximal and middle phalanges and metacarpal of the ring finger, as well as over the proximal phalanx of the small finger. There were no additional lesions.
Imaging Findings
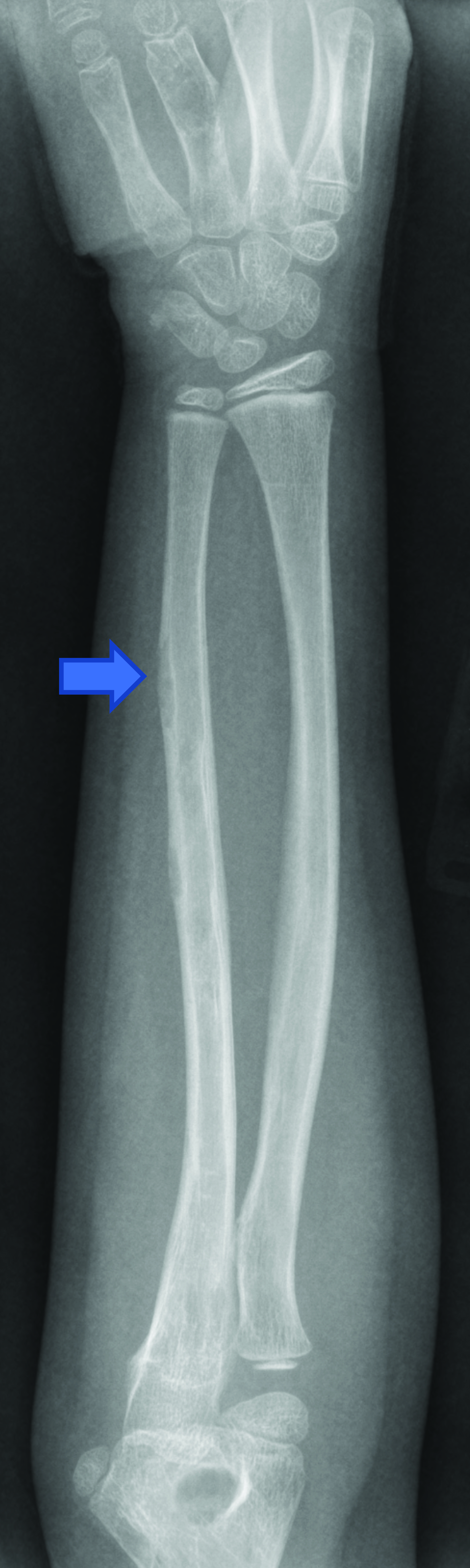
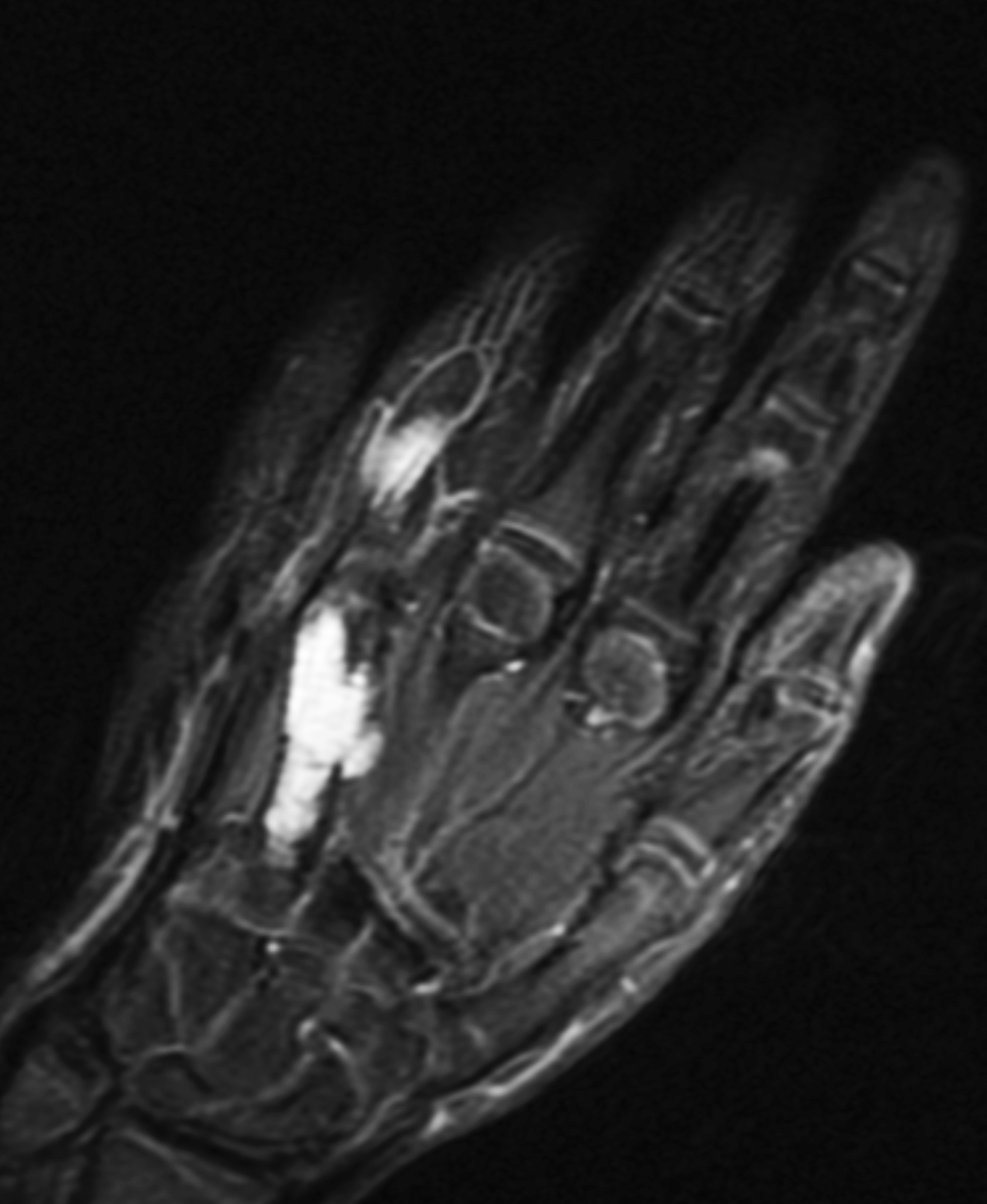
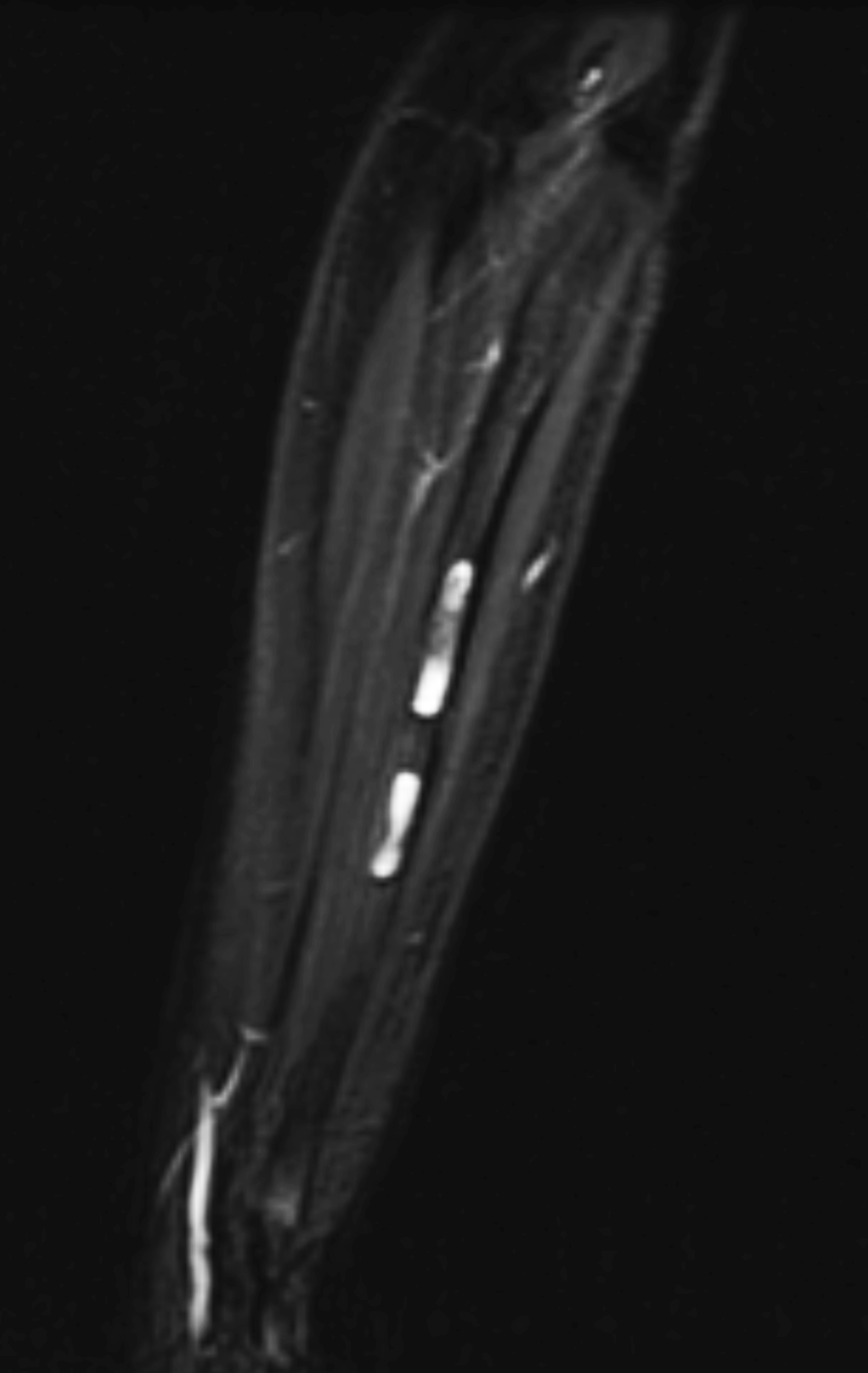
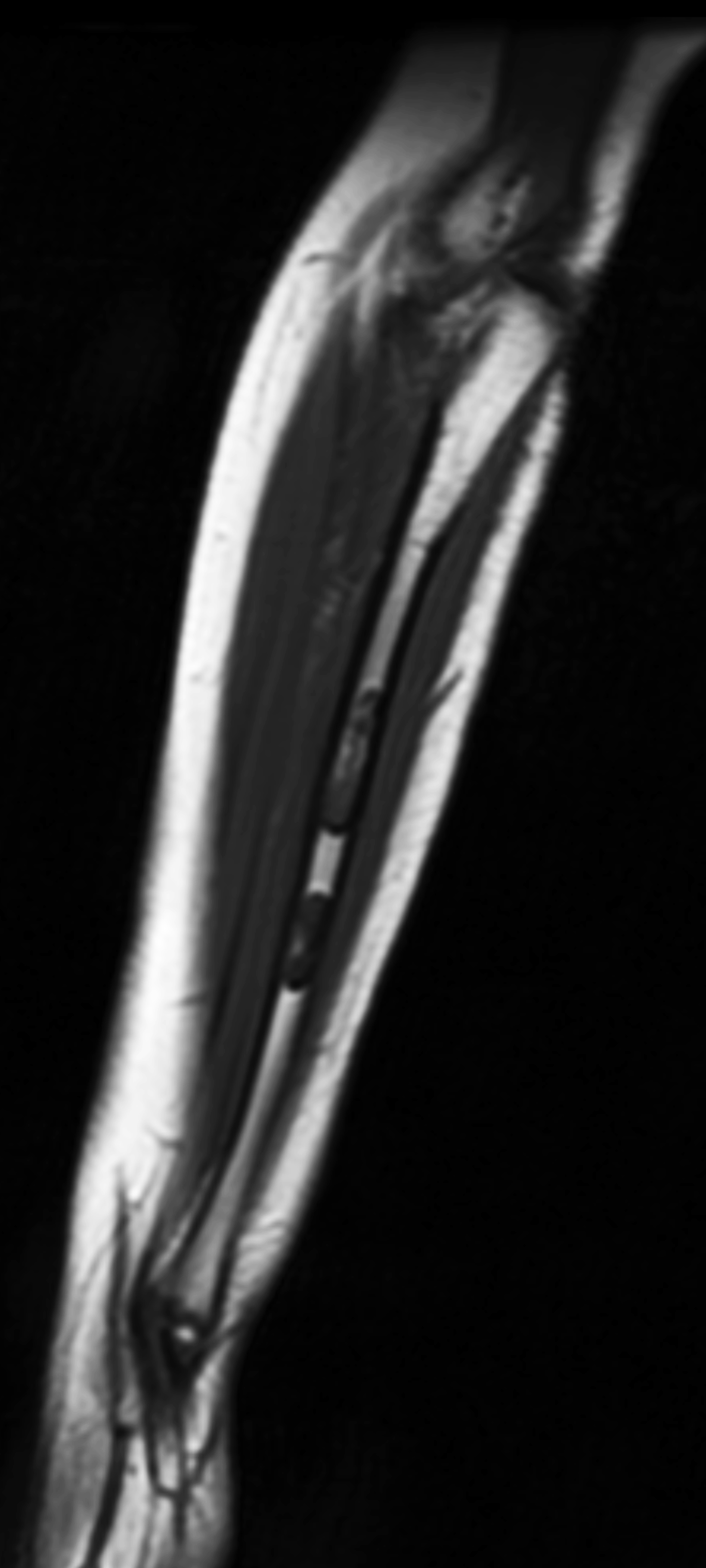
Radiography of the right hand (Figure 1) revealed numerous expansile lucent lesions within the bones of the right hand, most notably involving the proximal and middle phalanges of the fourth and fifth digits in addition to the metacarpal of the fourth digit. Each lesion demonstrated a ground-glass matrix and a narrow zone-of-transition. A skeletal survey revealed additional lucent lesions within the right ulna (Figure 2). Noncontrast MRI of the right hand and forearm (Figure 3) revealed multiple lobular, expansile masses that were homogeneously T2 hyperintense and T1 isointense to muscle within the metacarpal, proximal phalanx, and middle phalanx of the fourth digit, in addition to lesions within the proximal and middle phalanx of the fifth digit. Within the ulna mid-diaphysis, two centrally based lobular lesions displayed homogeneous T2 hyperintensity and T1 isointensity to muscle. All lesions were consistent with enchondromas.
Diagnosis
Ollier disease (multiple enchondromatosis). Differential diagnosis includes Maffucci syndrome.
Discussion
Ollier disease is a rare, nonhereditary disease of the appendicular skeleton that manifests as multiple enchondromas. The short, tubular bones of the hand are most commonly involved, followed by the femur, tibia, fibula, humerus, radius, and ulna. The prevalence of Ollier disease is about 1:100,000. It usually manifests within the first decade of life and has an equal incidence in males and females.1
In Ollier disease, the multiple enchondromas are often unilateral and may be associated with concomitant limb deformities and shortening. Pathological fractures are common sequelae of long-standing disease.
The assessment for Ollier disease begins with the physical exam, which will often reveal multiple, hard, palpable nodules within the bones of the hand. A hand radiograph should be the first imaging study; it characteristically reveals multiple, expansile, lucent lesions within the metaphyses of the short tubular bones. Bones may exhibit erosion and endosteal scalloping without significant periosteal reaction. Pathological fractures can be seen in up to 60% of patients at initial presentation.2 An MRI exam typically reveals multiple lobulated bone lesions with intermediate T1 and intermediate-to-high T2 signal intensity.3
Definitive diagnosis, if required, is obtained through direct tissue sampling via bone biopsy. The pathological samples in this study revealed multiple fragments of hypercellular hyaline cartilage with focal perichondrium lining, bony trabeculae, and fragments of detached hypocellular bone marrow, consistent with enchondroma.
Different theories have been proposed regarding the pathogenesis of Ollier disease. One is that somatic mosaic mutations in the IDH1 and IDH2 genes, which code for isocitrate dehydrogenase (a digestive enzyme used in the citric acid cycle) and the PTHR1 (parathyroid hormone 1 receptor) play a role.4 Depending on the patient’s family history, gene sequencing may be performed at the time of diagnosis.
Similar to Ollier disease, Maffucci syndrome is a separate, nonhereditary syndrome characterized by multiple enchondromas. However, Maffucci syndrome also involves the coexisting presence of multiple soft-tissue hemangiomas and/or lymphangiomas, which are absent in Ollier disease.5 These disorders share many overlapping themes, including the propensity for enchondromas to undergo malignant transformation to chondrosarcoma.
Pain in an apparent enchondroma or an abrupt increase in lesion size should prompt evaluation for malignant transformation. As the imaging modality of choice, MRI can distinguish between enchondroma and chondrosarcoma; the presence of new soft-tissue invasion or high T2 signal intensity (edema) surrounding the osseous lesion are suspicious for malignancy. Both conditions are also associated with an increased risk for the development of additional systemic malignancies, most commonly juvenile granulosa cell tumor of the ovary and gliomas.5
Ollier disease has no pharmacological treatment. Patients without significant deformities or functional impairment can begin with conservative “watchful waiting” and long-term follow-up. Patients with early-onset disease or complications such as limb deformities, pathological fractures, or malignant transformation require surgical treatment;6 options include lesion resection/curettage, internal fixation of fractures with bone grafts, and/or amputation in the most advanced cases.6
The patient in this study was treated with right fourth digit proximal phalanx enchondroma curettage with distal radius bone grafting. Patients with corresponding limb deformities can benefit from bone lengthening techniques, but they often require multiple procedures owing to a high rate of recurrence and angular deformities.7
Conclusion
Ollier disease is a rare disease of the appendicular skeleton characterized by multiple enchondromas, most often in the small tubular bones of the hand. Common sequelae include limb deformities, pathological fractures, and malignant transformation of enchondromas to chondrosarcomas. The physical exam and radiological imaging remain paramount to proper diagnosis. Treatment options should be considered on a patient-to-patient basis, with the most invasive interventions (resection/curettage, internal fixation with bone grafts, limb amputation) reserved for patients with advanced or transformed malignant disease.
References
Citation
D M, RB T, AJ T. Ollier Disease. Appl Radiol. 2023;(4):36-40.
June 23, 2023