New PET Radiotracer Maps Fructose Metabolism to Detect Diseases
Images
A new PET radiotracer can differentiate diseased tissues from healthy tissues based on fructose metabolism, according to a study published in The Journal of Nuclear Medicine. Fructose metabolism—or fructolysis—is indicative of a variety of diseases, and by noninvasively mapping fructolysis physicians can more accurately detect diseases and treat them earlier.
Glucose is used as the primary biochemical fuel throughout the body, powering key processes like tissue function, growth, and repair. Glucose is also consumed extensively during inflammation and cancer growth and can be visualized with PET scans. Evidence continues to mount that disease processes can force cells to use alternative fuels, like fructose, to power the progression of various diseases, yet an accurate PET imaging dye to measure fructose metabolism is not currently available.
“The fundamental importance of fructolysis in metabolic, neurodegenerative, and cardiac disorders, as well as cancer, has encouraged the development of methods to noninvasively map fructose metabolism,” stated Adam Shuhendler, PhD, associate professor and Canada Research Chair at the University of Ottawa, and scientist at the University of Ottawa Heart Institute in Ottawa, Canada. “Our work focused on this diagnostic opportunity and revisited the design of an imaging dye capable of mapping fructose use with high reliability.”
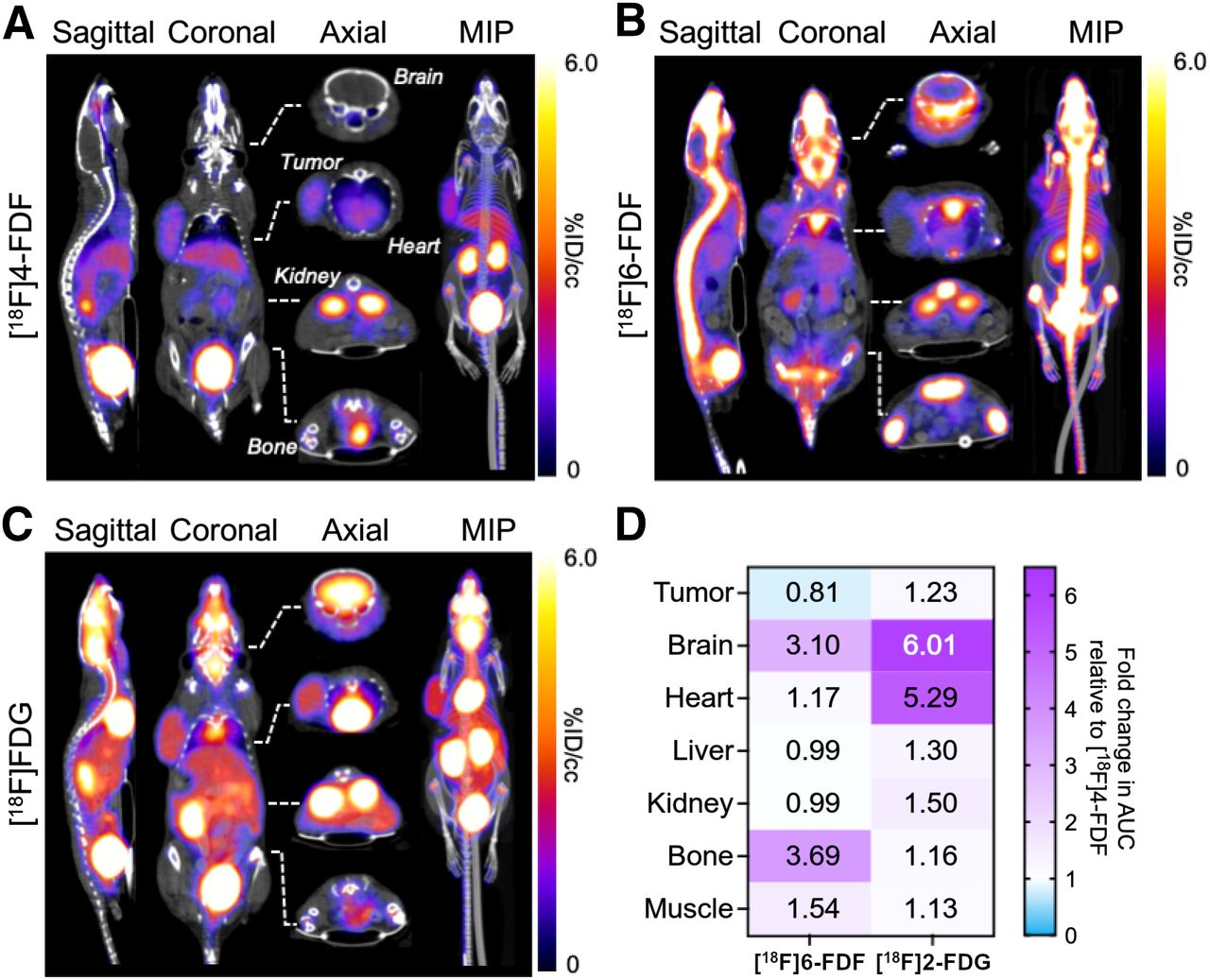
Previous approaches to fructose dye generation resulted in the non-specific accumulation of the PET imaging signal in bone tissue. In this study, researchers used the fructose metabolic pathway to inform where to modify fructose with an imaging label and created a new dye known as [18F]-4-fluorodeoxyfructose (4FDF). 4FDF resulted in the successful trapping of the labelled fructose in disease tissues and not in the bone.
With this new fructose-based imaging dye, researchers compared 4FDF to the clinical standard for glucose mapping, FDG, in a mouse model. Like FDG, 4FDF accumulated in tumor tissue, but unlike FDG, it did not accumulate in healthy brain or healthy heart, two organs with very high FDG uptake. When inflammation was induced in the brain and heart, both organs showed strong 4FDF signals. Bone uptake was minimized with 4FDF, further supporting the need for specific mapping of tissues that have undergone the glucose-to-fructose fuel switch that is a signature of heart and brain diseases.
“For the first time, fructose metabolism can be mapped sensitively with PET imaging, with the potential to open new applications for imaging-based diagnoses not possible with FDG,” said Shuhendler. “By widening the gap between the amount of 4FDF retained in healthy versus diseased heart and brain, disease of these organs can be more sensitively detected. The scope of precisely which diseases is still currently under investigation, but could include stroke, brain metastases, and heart attacks.”