New Guidelines Aim to Standardize Swallowing Fluoroscopy
 Despite widespread use, there has been no standard practice to guide the use of swallowing fluoroscopy for patients with swallowing problems caused by head and neck cancer, stroke, neurodegeneration or prolonged intubation in the US.
Despite widespread use, there has been no standard practice to guide the use of swallowing fluoroscopy for patients with swallowing problems caused by head and neck cancer, stroke, neurodegeneration or prolonged intubation in the US.
To address this gap, the American Broncho-Esophagological Association (ABEA) with input from a wide array of specialists, are providing the most detailed and comprehensive set of standards for swallowing fluoroscopy. Led by author Shumon Dhar, MD, Assistant Professor of Otolaryngology-Head and Neck Surgery at UT Southwestern, the standards are described in a recent article in The Laryngoscope.
“This work has immediate ramifications on patient care. Clinicians all over the country and internationally have requested copies of the position statement to advocate for changes to their local institution’s swallowing fluoroscopy protocols to better serve their patients,” said Dr Dhar, a fellowship-trained laryngologist and broncho-esophagologist at the UTSW Voice Center. He said the standardization of swallowing fluoroscopy will allow for the same level of high-quality testing for patients across institutions, leading to more accurate diagnoses and treatment recommendations.
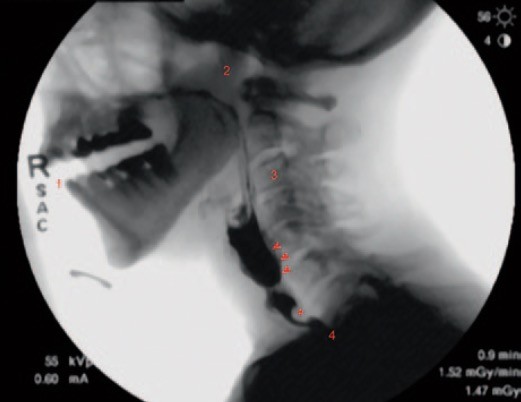
Swallowing fluoroscopy, which includes video fluoroscopic swallow studies (VFSS) and esophagrams, refers to noninvasive exams that allow physicians to examine the physiology of the throat and esophagus during swallowing to help identify what liquids and foods patients can tolerate and guide targeted treatment for patients with swallowing dysfunction.
In an effort to reduce practice variation and improve the quality of care for patients with swallowing dysfunction, an expert development group was formed to compose statements on swallowing fluoroscopy best practices. The group consisted of various specialists, including otolaryngologists, radiologists, and speech-language pathologists.
Forty statements reached full consensus following a thorough review of the literature and a blinded multistage voting protocol. The statements encompassed areas such as patient selection, fluoroscopic study choice, radiation safety, training requirements, videofluoroscopic swallow study and esophagram techniques, and interpretation of results.
In addition to making these evidence-based recommendations, the development team was tasked with identifying gaps in knowledge that require further research. Accordingly, they found a paucity of evidence to guide certain aspects of esophagram indication criteria and technique.
The development team concluded that VFSS and esophagrams are valuable tools for the comprehensive assessment of swallowing. These recommendations from the ABEA will empower health care institutions to standardize their protocols and encourage multidisciplinary collaboration, and as a result advance the safety, efficiency, and accuracy of swallowing fluoroscopy across the country.