Intraluminal Duodenal Diverticulum
Images



Case Summary
An adult presented to the emergency department with a 2-day history of postprandial cramping pain in the epigastric region, associated with intermittent nausea and vomiting. Antacid medication for presumptive gastritis had not resolved the patient’s symptoms. The patient’s physical examination and blood tests were unremarkable.
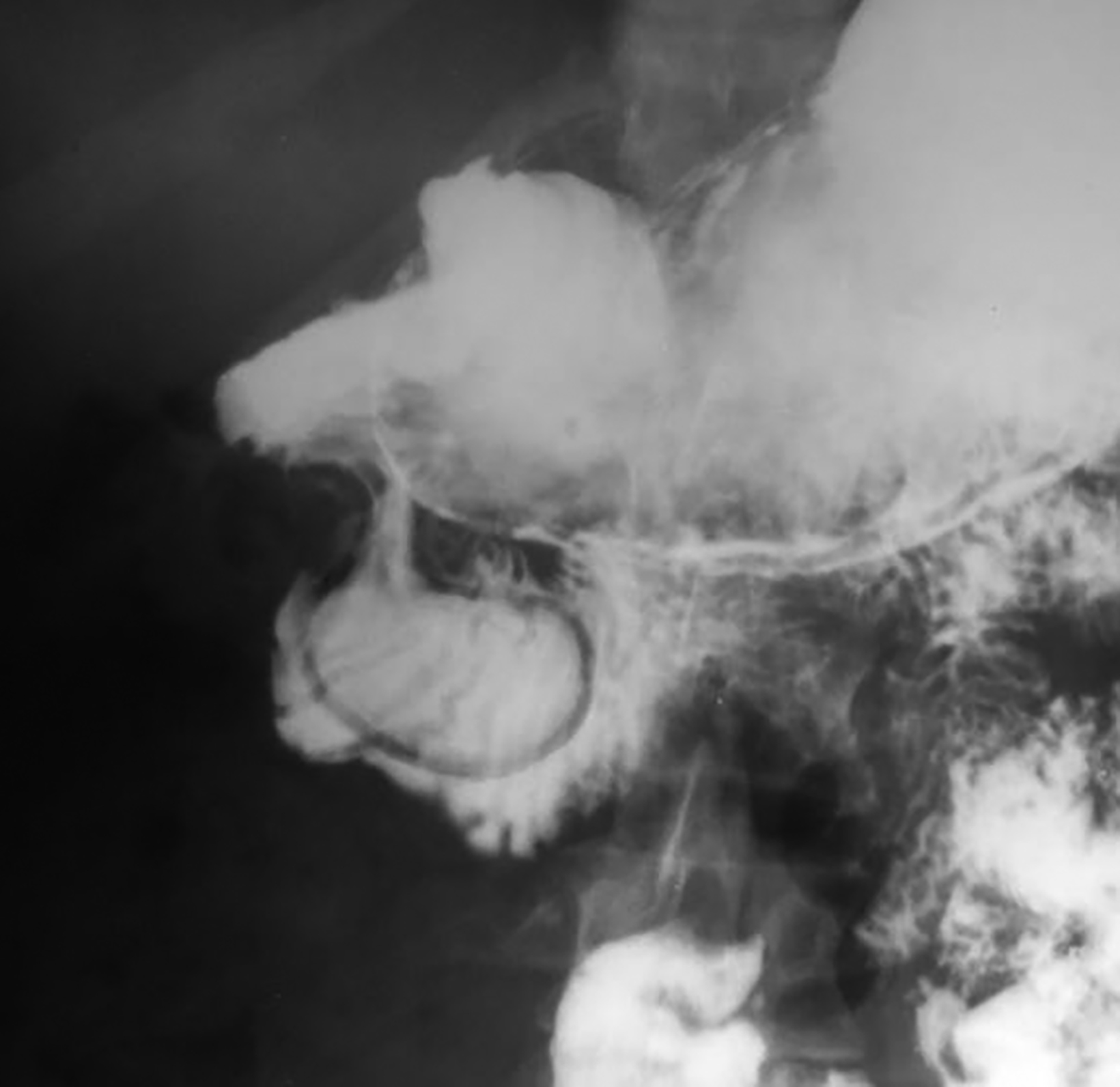
Computed tomography (CT) of the abdomen revealed a thin-walled saccular lesion protruding into the descending part of the duodenum. Upper gastrointestinal study showed a barium-filled mucosal pocket with elongated attachment to the periampullary area.
Imaging Findings
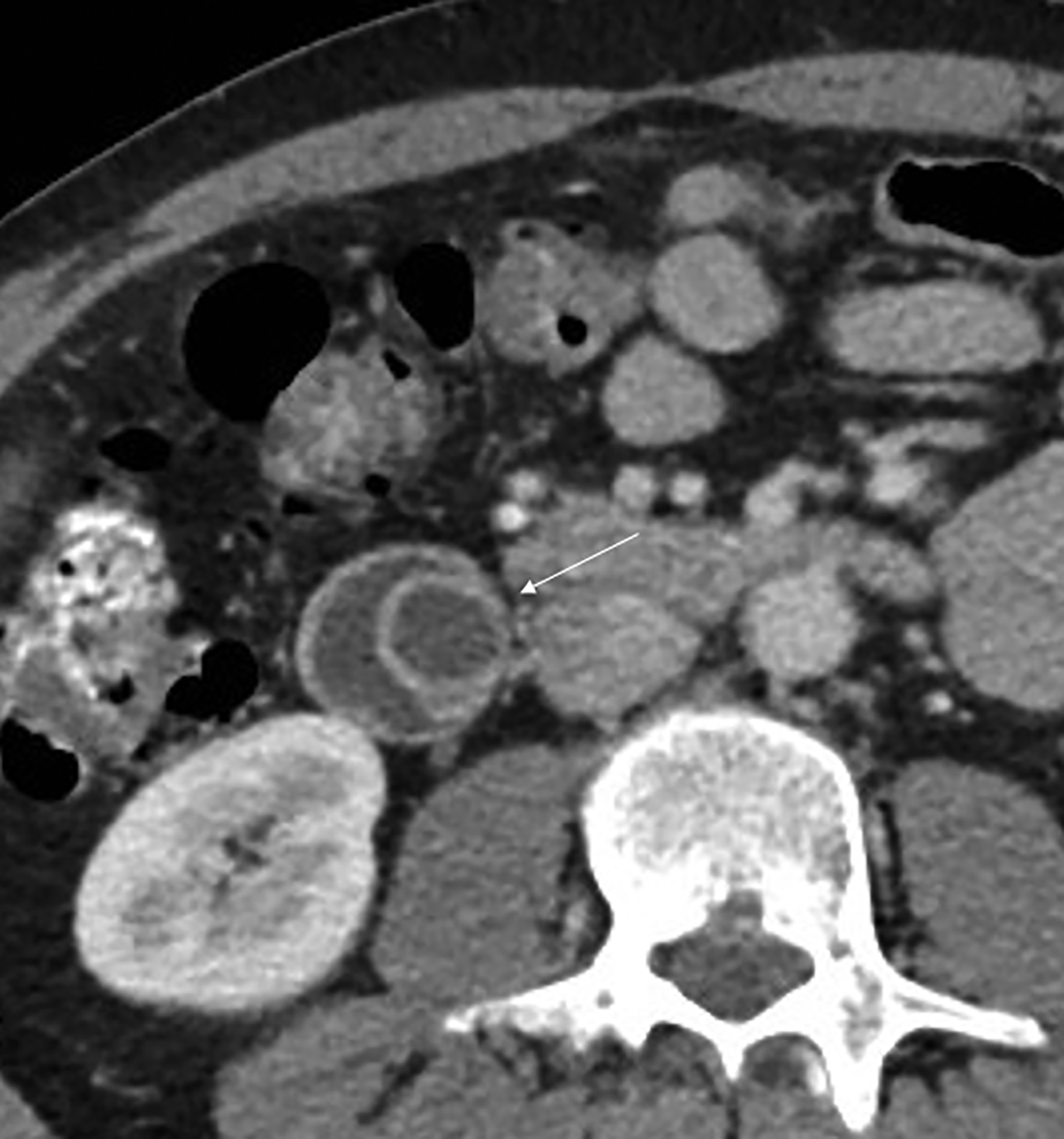
Axial images of contrast-enhanced CT of the abdomen demonstrated a 2 cm cystic structure within the second part of the duodenum. Its elongated attachment to the periampullary region was visible on the coronal image (Figure 1). Subsequent upper gastrointestinal examination revealed a barium-filled saccular structure with thin walls protruding into the duodenal loop (Figure 2).
During endoscopy this mucosal pocket had a 4-5 mm, slit-like aperture at its posterior wall near its tip, but it did not allow passage of the endoscope. This outflow opening was then enlarged to about 10mm by transection of its margin with biopsy forceps and thermal cauterization. The patient’s symptoms abated after this procedure. Abdomen CT was performed 2 years later because of left lower abdominal pain, fever, and leukocytosis due to sigmoid diverticulitis. This examination showed a partially collapsed and smaller mucosal pocket in the duodenal loop (Figure 3). It had not caused any recurrence of obstructive symptoms.
Diagnosis
Intraluminal duodenal diverticulum.
Differential diagnoses include choledochocele, duplication cyst, and pedunculated duodenal lipoma.
Discussion
Intraluminal duodenal diverticulum (IDD) is a rare developmental anomaly, but it is usually first recognized in adult patients. It represents delayed manifestation of a congenital duodenal web or diaphragm, which results from incomplete recanalization of midgut during the 6th-8th weeks of embryologic life.1,2 This duodenal diaphragm with its small central orifice will gradually protrude distally into the duodenal lumen as a mucosal pocket, like a windsock, because of the peristaltic pressure and intraluminal content. The outlet of IDD can be blocked by food particles, undigested vegetables, or ingested foreign bodies. This would result in distention of the IDD and intermittent duodenal blockage, as in this patient and other reported cases.2-5
About 75 cases of this entity have been recorded in the medical literature. The majority of these patients have been adults in their third or fourth decades of life.2-6 It is noteworthy that despite the congenital nature of this lesion, only a few of these cases had manifested during childhood and were often associated with foreign body retention in the IDD.5
The diagnosis of IDD is usually made by its distinct appearance on the upper gastrointestinal barium study or abdominal CT examination.2,3,6 There have been 2 recent reports of this lesion being demonstrated on MR imaging.7 Differential diagnostic considerations include choledochocele, Wirsungocele, duodenal duplication cyst, and an inverted diverticulum or other periampullary lesions.8
Several complications have been associated with IDD. These include duodenal obstruction, gastrointestinal bleeding, and acute pancreatitis.4,5
Some patients may be asymptomatic and IDD may become apparent as an incidental finding of radiological studies performed for unrelated reasons. However, symptomatic cases would require prompt treatment. Surgical resection through open duodenotomy has been used, but it may carry the risk of inadvertent injury to the ampulla and pancreaticobiliary ducts.9 Endoscopic removal of IDD and transection or enlargement of its outflow aperture has been successfully performed in several patients.2,10 In this case, the intervention relieved the patient’s obstructive symptoms.
Conclusion
Intraluminal duodenal diverticulum represents delayed manifestation of a congenital duodenal diaphragm. It is an unusual finding in adults, who may present with upper gastrointestinal symptoms caused by blockage of diverticular outflow orifice by food or foreign body. This lesion appears as a thin-walled saccular structure within the duodenal lumen on CT and barium examinations, and endo- scopic intervention can relieve its obstructive symptoms.
References
Citation
GG G, DR N. Intraluminal Duodenal Diverticulum. Appl Radiol. 2023;(2):45-47.
March 7, 2023