Embryonal Rhabdomyosarcoma of the Bladder
Images

Case Summary
A male toddler presented with recent onset of straining during voiding and bowel movements. Ultrasound detected a large mass in the bladder lumen. Ultrasound-guided biopsy revealed an embryonal rhabdomyosarcoma (RMS) of the bladder and prostate.
There was no evidence of metastases. The tumor was classified as stage III, group II. Subsequent mass excision was performed, followed by cystoscopically guided bilateral ureter reimplantation and bladder neck reconstruction.
Imaging Findings
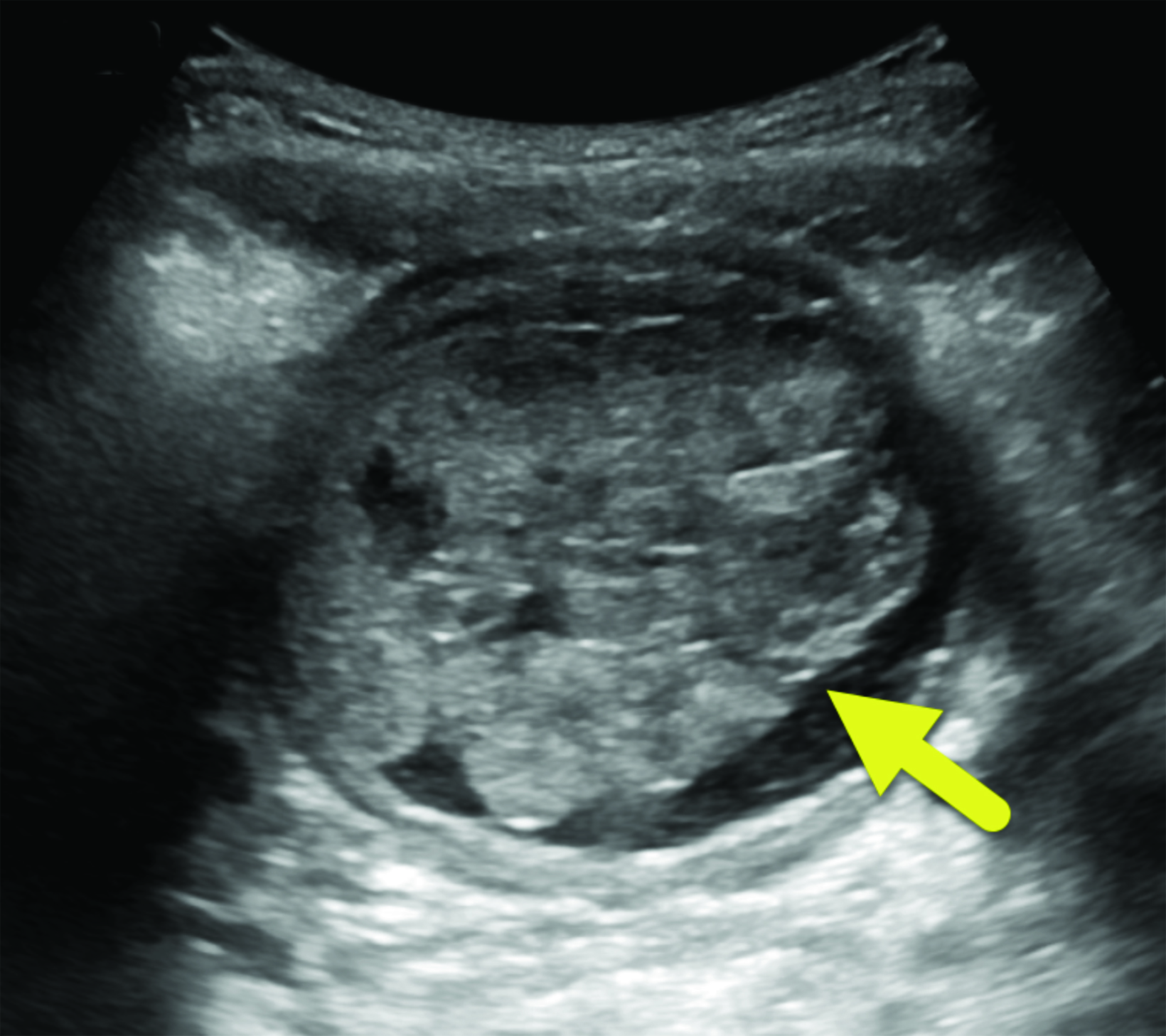
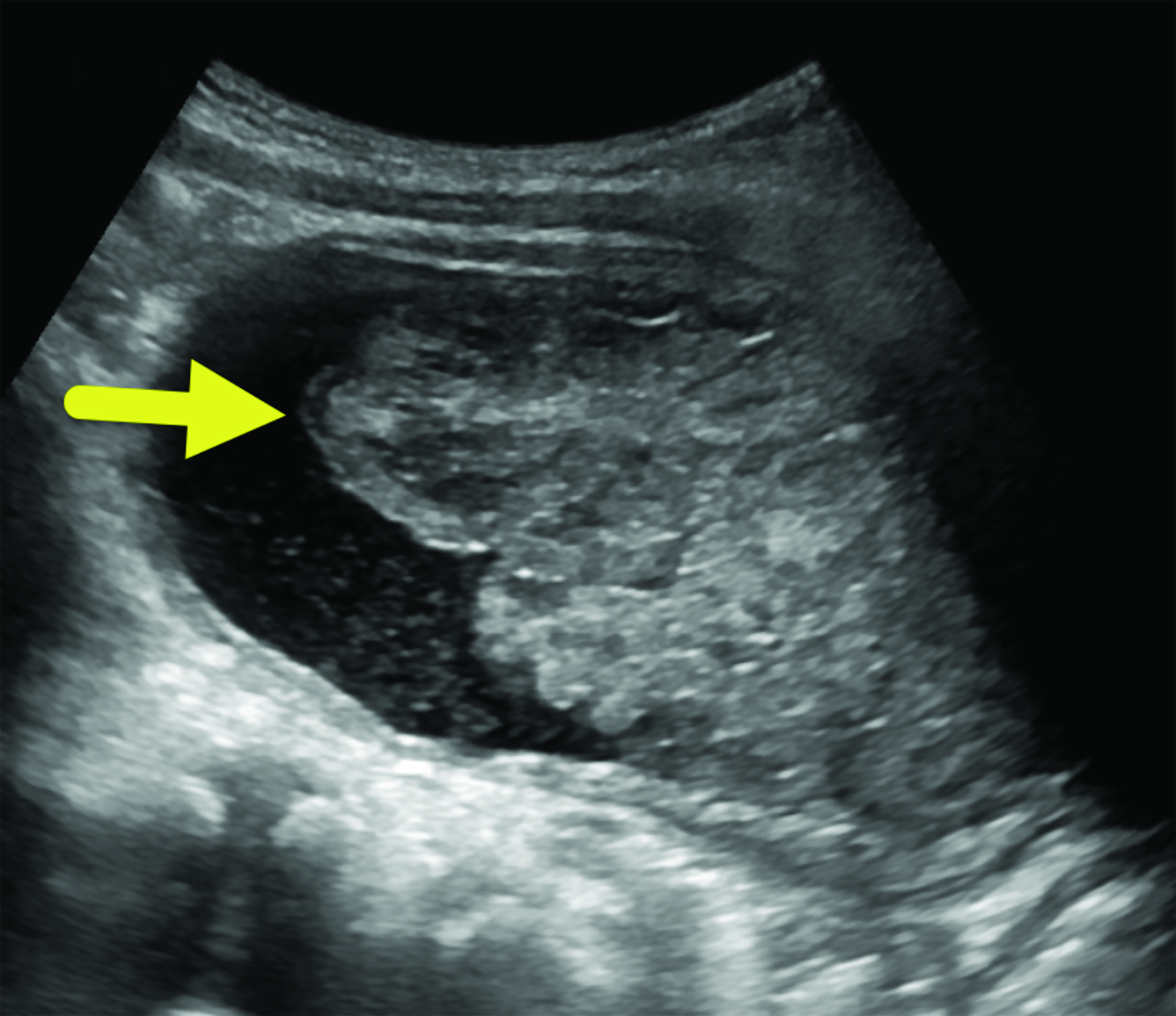
Ultrasound (Figure 1) detected a large, lobulated mass in the bladder lumen. Contrast-enhanced CT of the abdomen and pelvis (Figure 2) identified a lobulated mass at the base of the bladder extending into the proximal urethra.
Diagnosis
Embryonal rhabdomyosarcoma of the bladder. The differential diagnosis includes other subtypes of RMS, papillary urothelial neoplasm of low malignant potential, and fibroepithelial polyp.
Discussion
Rhabdomyosarcomas are the most common malignant, soft-tissue sarcomas in children and are divided into 4 subtypes: embryonal, alveolar, pleomorphic, and spindle cell/sclerosing.1 Embryonal is the most common, accounting for approximately 60% of all cases. It predominantly occurs in children under 5 years of age, although a smaller peak has also been noted in adolescence.2 This subtype usually occurs in the head, neck, and genitourinary regions and has a male-to-female ratio of 1.5:1.2
While the etiology of RMS is still unknown, an increased prevalence is associated with genetic syndromes such as Li-Fraumeni, Gardner, Beckwith-Wiedemann, and neurofibromatosis type 1.3 Embryonal RMS is characterized by a loss of heterozygosity at 11p15.5 and whole or partial gains of chromosomes 2, 8, 12, 13, and/or 20.2 Mutations in the FGFR4/RAS/AKT pathway and increased PTEN hypermethylation has also been detected in this subtype.2
Patients often present with signs and symptoms resulting from mass effect, such as urinary retention for tumors in the genitourinary region.2 Ultrasound should be used initially to confirm the presence of a tumor. Computed tomography or MRI can be performed to further assess the tumor, as well as to identify potential complications and potential sites of metastasis.4
Biopsy is necessary for diagnosis. On histology, embryonal RMS is characterized by rhabdomyoblasts at variable stages of differentiation in sheets and nests within a myxoid matrix.3 Tumors are commonly classified by pre-treatment tumor, nodes, metastasis (TNM) staging and the postoperative Intergroup Rhabdomyosarcoma Study grouping system.5 It is estimated that 15% of pediatric RMS patients present with metastasis. The outcome for these patients is poor.5
Tumors of the bladder and prostate region must be classified at least stage II owing to their unfavorable location.7 The tumor group is based on histology results. Group I tumors constitute completely resected localized disease.7 Group II tumors make up com- pletely resected masses with evidence of regional spread. Group III comprises incompletely resected tumors, and group IV masses are accompanied by distant metastases. Clinical risk is determined by tumor stage, group, and histology.
There are 3 risk categories: low, intermediate, and high.7 Low risk consists of stage II and III, groups I and II embryonal tumors; these have an 88% 3-year, failure-free survival rate. Intermediate-risk tumors (stages II and III, group III) have a 55-76% 3-year, failure-free survival rate, and high-risk tumors (stage IV, group IV) have < 30% 3-year, failure-free survival rate.7
Treatment of RMS takes a multimodal approach involving surgery, chemotherapy, and radiotherapy.5 Two main treatment protocols exist for pediatric bladder and prostate RMS: the North American approach, developed by the Children’s Oncology Group, and the European approach, developed by the International Society of Pediatric Urology. While both protocols involve chemotherapy following histological diagnosis, the North American approach recommends radiotherapy to better establish local control for organ preservation.6 In most cases, surgery consists of partial resection with the goal of bladder preservation.6
Multimodal therapy offers good outcomes, with estimated 5-year overall survival for bladder/prostate RMS as high as 86% and 5-year, event-free survival as high as 79%.7 However, treatment may result in abnormal lower urinary tract function (ie, incontinence, infection, decreased renal function, and chronic hematuria) in up to 60% of patients and sexual dysfunction, with the proportion of each increasing with longer follow-up time.6 The true frequency of sexual dysfunction is uncertain in survivors but is noted in older patients.
Conclusion
Embryonal rhabdomyosarcomas are the most common subtype of RMS. They usually present in the head, neck, and genitourinary regions of males under age 5 years. Their etiology is not yet known, but RMSs have been associated with genetic syndromes. Pelvic RMS can present with urinary retention and other signs of mass effect. Multimodal treatment involving chemotherapy, surgery, and radiotherapy can be effective.
References
Citation
R Z, RB T, CM S, AJ T. Embryonal Rhabdomyosarcoma of the Bladder. Appl Radiol. 2023; (6):40-42.
November 3, 2023