Chondroblastic Osteosarcoma of the Mandible
Case Summary
A previously healthy adult presented with worsening unilateral facial swelling and numbness over 5 years. The patient had a significant increase in swelling over 6 weeks, and endorsed trismus as well as perinasal and mandibular numbness over the past year. They denied having pain, purulence, dysphagia, or sialolithiasis. The patient also denied tobacco or alcohol use. There was no personal or family history of salivary cancer, squamous cell cancer, or other malignancy. On clinical examination, there was pronounced right-sided facial swelling without overlying skin changes or tenderness to palpation. Laboratory findings were unremarkable.
Imaging Findings
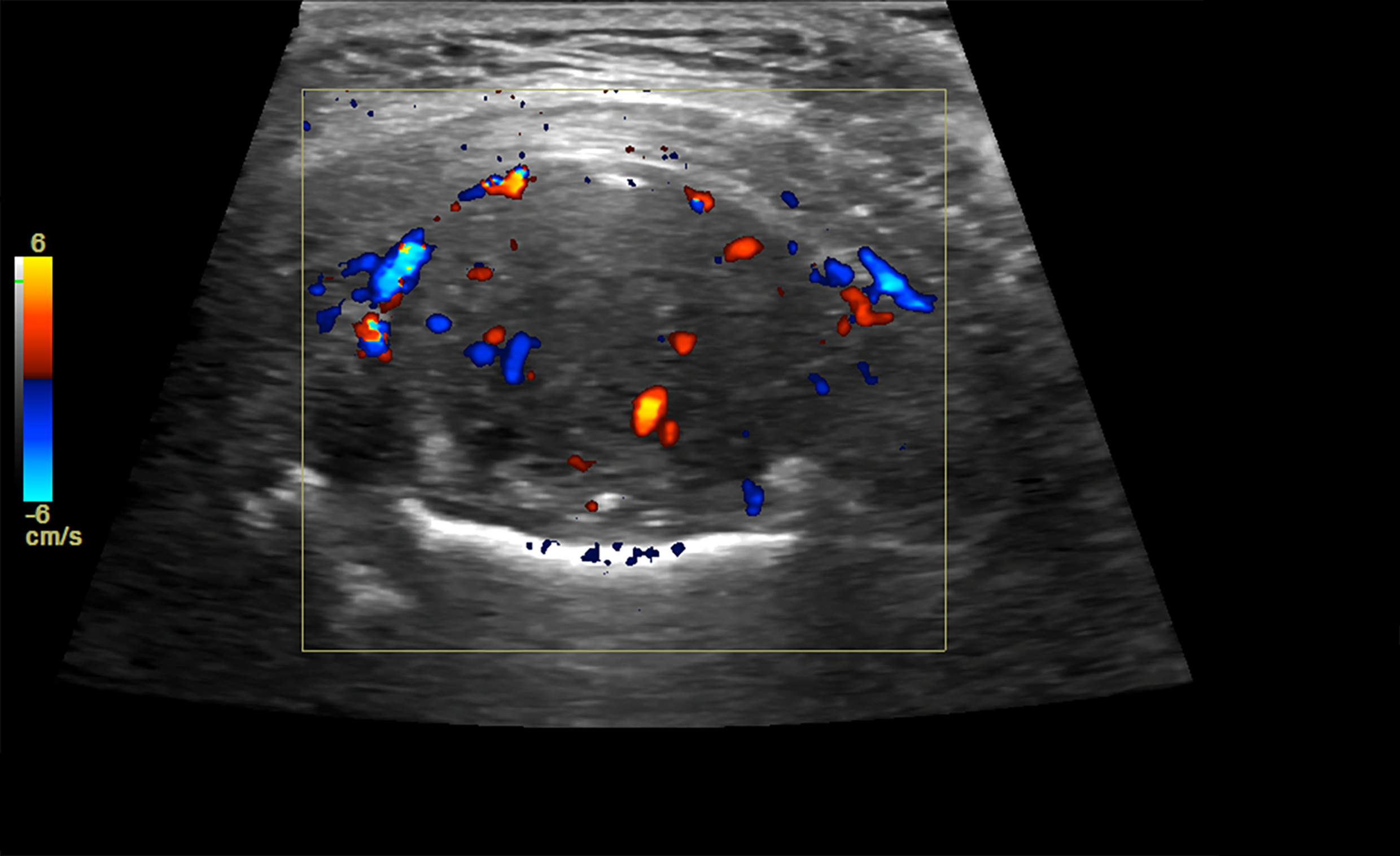
Superficial ultrasound of the right facial swelling ( Figure 1 ) revealed a 4.5-cm, heterogeneously hypoechoic, solid mass, with few focal hyperechoic areas suggestive of calcifications. Internal flow was demonstrated at the region of the right mandible/parotid gland. Subsequent neck MRI ( Figure 2 ) demonstrated a large, aggressive-appearing, diffusely enhancing mass in the right masticator space, with significant local mass effect. Portions of the mass demonstrated indistinct borders with the ipsilateral parotid, masseter, and pterygoid muscles, concerning for invasion. There was no intracranial extension or perineural tumor spread. Facial CT, to better assess osseous involvement, demonstrated heterogeneous expansion of the mandibular condyle ( Figure 3 ). Prominent bilateral level 2A lymph nodes were unchanged from the MRI.
Grayscale and color Doppler ultrasound evaluation of the right mandible/cheek demonstrates a large heterogeneously hypoechoic solid mass in the region of the right parotid gland measuring up to 4.5 cm in diameter with internal vascular flow.
Coronal fat-suppressed T1 pre- (A) and postcontrast (B) images of the face demonstrate a large, diffusely enhancing (calipers on B) mass in the right masticator space, with significant local mass effect on adjacent structures. Heterogeneous expansion of the mandibular condyle and enhancement of the mandibular periosteum are also present.

Axial (A) and coronal (B) noncontract CT images in bone window/algorithm of the face demonstrate the right masticator space mass that appears to originate from the right mandibular condyle, causing significant local mass effect. There is mandibular osseous remodeling and periosteal reaction with internal calcifications of the soft-tissue component.

Diagnosis
Chondroblastic osteosarcoma of the mandible.
Differential diagnosis for an aggressive mandibular mass includes Ewing sarcoma, chondrosarcoma, metastatic disease, and lymphoma/leukemia.
Discussion
Osteogenic sarcoma is the most common primary bone malignancy. Despite this, it remains an uncommon tumor representing approximately 0.2% of all malignancies.1 Although usually found in the metaphyseal region of long bones, osteosarcoma has been reported rarely in the craniofacial bones. Osteosarcomas represent approximately 1% of head and neck malignancies and 6-10% of all osteosarcomas.2 A specific pathogenesis of osteosarcoma has not been described; however, there are several predisposing factors, including rapid bone growth during adolescence, exposure to radiation, and bony abnormalities such as Paget disease, osteochondromatosis, and chronic osteomyelitis.3, 4 None of these factors applied to the patient.
Osteosarcoma can be classified by cellular differentiation as osteoblastic, fibroblastic, or chondroblastic. The chondroblastic subtype is generally composed of atypical chondroid areas comprising pleomorphic and atypical binucleate cells.5 In the craniofacial bones, osteoblastic osteosarcoma is the most common subtype, followed by chondroblastic.
Physical examination and radiological findings are invaluable in the diagnosis, staging, and preoperative treatment planning of patients with osteogenic sarcomas. Ultrasound and radiographs can diagnose osseous involvement, with one series reporting positive predictive values of 53.3% (24/45) and 97.8% (44/45), respectively.6 Radiographic findings such as a mixed radiolucent and radiopaque lesion, periodontal ligament widening, a radiopaque mass with “moth-eaten” appearance, and presence of a Codman triangle have been reported in head and neck osteosarcomas.7 The classic “sunburst” appearance of malignant osteoid formation in extremity osteosarcomas is also often demonstrated in head and neck osteosarcomas.4
CT is primarily used for staging and improving the diagnostic yield of biopsy. CT findings in the osteosarcoma of the face have been shown to differ based on the location of the mass. Sarcomas of the maxilla tend to be found on the alveolar ridge with an equal distribution of lytic and blastic osseous disease, while those found on the mandible tend to be at the ramus and/or condyle with predominately blastic disease, as was seen in our case.2 CT can also improve the detection of lytic lesions that may not be readily apparent on radiography. MRI is indispensable for accurately staging osteogenic sarcomas, including evaluating for direct and perineural disease spread.8
The most common presentation of mandibular osteosarcoma is local swelling with or without pain or numbness, and limitation in mouth opening.1, 4, 9 Several less common signs include tooth loosening, weight loss, and nasal bleeding.4, 9 Owing to the rarity of the disease, determining a conclusive set of prognostic factors is difficult.4, 9 Several prognostic factors for osteogenic sarcoma have been studied, including age, sex, tumor site, radiographic appearance, histology, tumor grade, and predisposing conditions.4, 9 Of these factors, older patient age (> 60 y), nonmandibular location, tumor size greater than 6 cm, and a history of previous trauma were found to be statistically significant factors associated with decreased disease-free survival.4, 9 Despite this, patients with osteosarcomas of the face generally have a better prognosis than those diagnosed with an extremity osteosarcoma.1, 4, 9
Because of the scarcity of guidelines, treatment of head and neck osteosarcomas is based heavily on data from case reports and treatment modalities utilized against osteosarcomas of other body regions. Management strategies include multidrug chemotherapy, wide-margin radical resection, and radiation therapy.9 Treatment often varies based on patient and tumor characteristics, with larger, more aggressive, and high-grade lesions typically receiving multimodal therapy, including multidrug chemotherapy, to decrease the tumor size prior to radical resection and radiation therapy.
Conclusion
Chondroblastic osteogenic sarcoma of the mandible is a rare tumor in an uncommon location that has been described less extensively than extremity osteosarcoma. Patient presentation may vary but will often include unilateral facial swelling, with diagnostic imaging findings varying with histopathological subtype. Factors that worsen prognosis include older patient age, large tumor size, and a nonmandibular location. Awareness of this tumor can ensure early diagnosis and multimodal therapy to improve survival. Continued reporting of similar cases is necessary to enhance the literature on multimodal radiological diagnostic/staging and treatment schemas of this disease.
References
Citation
Ohioma D, Owens RW, Choi J. Chondroblastic Osteosarcoma of the Mandible. Appl Radiol. 2024;(5):45 - 47.
doi:10.37549/AR-D-24-0010
October 1, 2024