3D Printing: Bridging the Gap Between Radiologists and Surgeons
Images


Hand a cardiac surgeon a 3D-printed model of their patient’s own heart, or an orthopedic surgeon a 3D-printed model of their patient’s own spinal column and watch what happens. Don’t be surprised if they respond with nothing less than childlike wonder, says Susan A Churchill, MBA, BSRT(R)(N)(CT).
“We’re recreating anatomy in a tangible form, and when you give doctors these prints, they are like kids at Christmastime with a new toy in their hands,” says Churchill, supervisor of the Multi-Dimensional Image Processing Laboratory at Duke Radiology, Duke University Health System, Durham, NC. “They stare at it and twist it around, almost gleefully. We’re bridging that gap between radiologists and surgeons.”
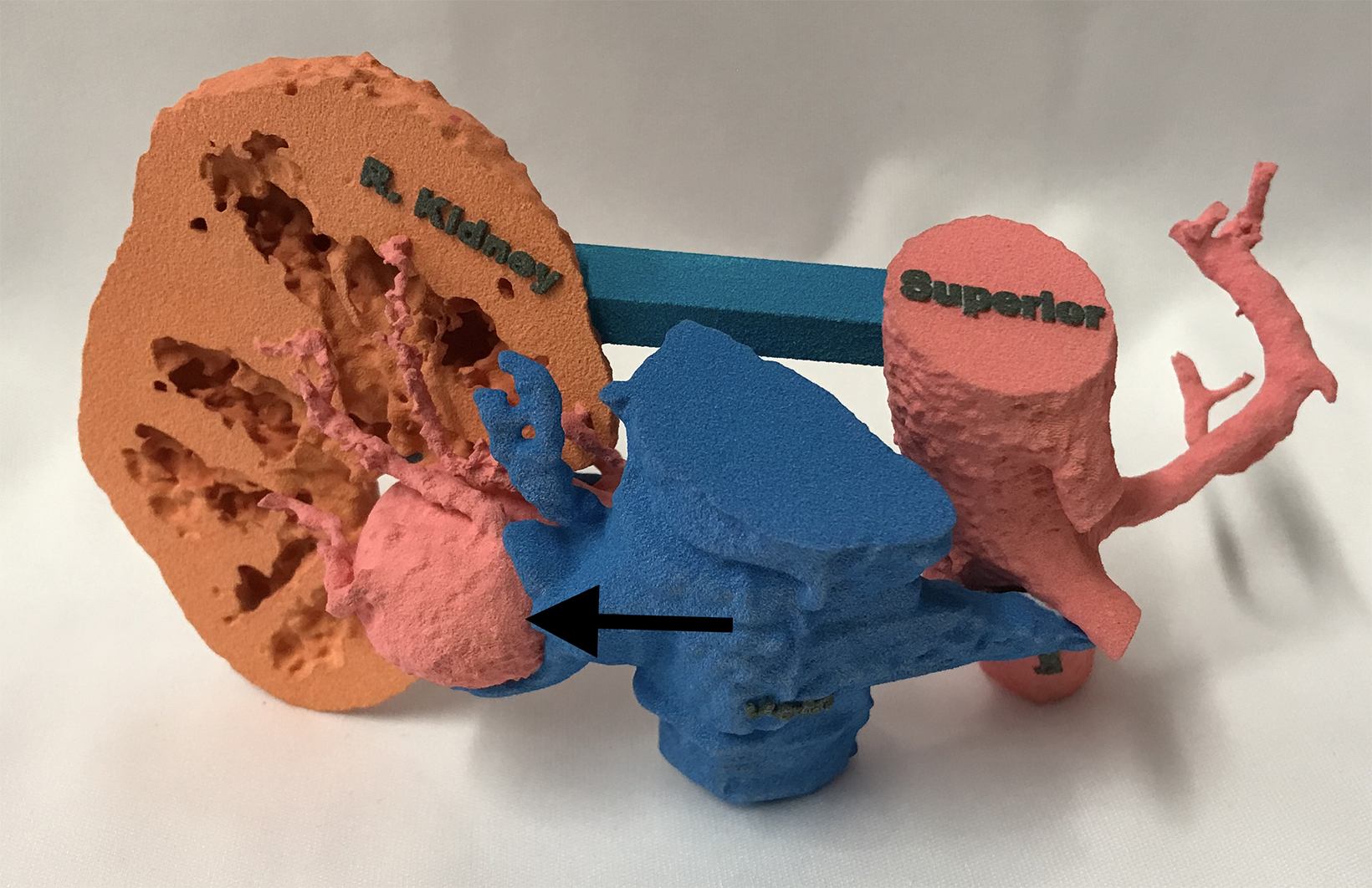
Indeed, thanks to the technological miracle that is 3D printing, radiologists are no longer just converting MRI and CT datasets into multidimensional images that can be turned every which way on a computer screen. They are using the data to generate actual physical models, complete with realistic textures, and colors, for enhanced surgical planning and simulation.
“We take that digital blueprint and turn it into a 3D model that’s transportable into the operating room or to the patient’s bedside,” says Sarah Bastawrous, DO, associate professor of radiology at the University of Washington School of Medicine and VA Puget Sound Health Care System, both in Seattle. “Radiology remains central in the growing field of medical 3D printing to improve the care of patients.”
Fides Regina Schwartz, MD, a senior research associate in the department of radiology at Duke, agrees.
“The fact that we now have resolutions of .6 mm with most systems and even a CT scanning system that can provide spatial resolution down to .2 mm slice thickness, that really helps a lot in making the models true to what you’d actually see in the patient,” Dr Schwartz says.
Clinical Benefits
Among a growing number of other 3D printing applications, models of the spine are being used to plan surgery for scoliosis and other deformities, says David Ballard, MD, assistant professor of radiology and director of the 3D Printing Lab at the Mallinckrodt Institute of Radiology at the Washington University School of Medicine in St Louis, Missouri. At Duke, Churchill says, models of the pelvis and shoulder are being used to help plan treatment of femoroacetabular impingement and complex fractures, while 3D-printed models of the brain are being used to plan surgery for refractory epilepsy.
The technology is also being used to treat cardiac diseases in children, despite the challenges of obtaining the data needed to print such small heart models for these cases. These include the size of the patients and the patient motion during CT and MRI scans. Fortunately, advances in imaging technology are making it easier to capture high-quality imaging data in these patients, says Churchill.
“The quality of the 3D model is only as good as the data used to create it,” she observes. “In gated studies, the ability to take a motion-free image is huge. The advancements in spatial resolution give us better visualization for the detailed anatomy, faster scans, and reduced motion artifacts … which all improves the output.”
Patient-specific 3D models also facilitate communication as well as patient and family understanding of their condition and proposed treatment(s).
“If the patient can see and hold their model, they understand what they’re dealing with and can really be part of the planning and care,” Churchill says.
In recent years, 3D printer capabilities and modeling materials have both improved while the costs of 3D printing have been falling, says Dr Schwartz. Improved technology and reduced costs have led to widespread use of 3D printing across healthcare, despite challenges such as reimbursement, funding, and regulatory considerations.
Hospital-based 3D printing programs can vary dramatically, from novelty applications to established clinical services with large volume production across many medical domains. As the possibilities for clinical use and research expand, Dr. Bastawrous asserts, “Medical 3D printing will add value to our surgical colleagues and allow for personalized patient care to improve health outcomes and patient satisfaction.”
Workflow and Resource Considerations
Despite 3D printing’s growing value to medical care, healthcare systems face a variety of operational and financial challenges to implementation. For one, the complexity of the 3D printing process demands a dedicated 3D printing lab and specially trained CT and MRI technologists and radiologists.
“You can’t just take the images you have in PACS and put them into a 3D printer,” says Dr Schwartz. “The DICOM format doesn’t print in 3D.” Instead, the radiologist or technologist must devise a special protocol for image acquisition and creation of an STL file for printing the 3D model. Many quality control steps are then executed in the segmentation and printing process before the model’s final review by a radiologist, she says, noting that adding 3D printing to already existing daily responsibilities of most technologists and radiologists would be “nearly impossible.”
Dr Ballard agrees, adding that, “you need at least one FTE (full time equivalent) — usually a non-physician — who’s doing the 3D printing and the majority of the segmentation, and a radiologist who often acts as an overseer of accuracy.”
The Costs of 3D Printing
The costs associated with opening and operating a 3D printing lab are significant. While equipment prices have dropped in recent years, they remain considerable. Duke purchased a 3D printer in 2016 for $350,000, with printing materials priced at about $600 per package. This year, Duke was quoted $56,000 for a similar printer, with materials coming in at about $400, Dr Schwartz says.
Dr Ballard adds that low-end printers range anywhere from $500 to $5,000, while mid-tier printers can cost $5,000 to $20,000; and high-end printers can reach upwards of $100,000 to $300,000.
“A lot of people get excited about the idea of a low-cost 3D printer, but it’s important to know what your surgeons—your end users— want in terms of capabilities and benefits. The less expensive ones may not perform as well,” Dr Ballard says. Other costs that must be taken into account include segmentation software licensing and the time required for technologists to print each model and radiologists to review it.
“If it takes the radiologist one hour per case, that may be too much time if it’s not accounted for, a big cost consideration for starting a 3D printing lab,” Dr Ballard says, noting that 3D printing cannot simply be a “pet project” of two or three radiologists. Instead, it must have the full backing of the institution.
Finally, there is the fact that 3D printing and models are not yet eligible for Medicare reimbursement. “In the vast majority of cases, it’s not reimbursed at all or adequately,” Dr Ballard says. “Just about every 3D printing lab I know of … operates at a loss.”
However, given the 2019 approval of temporary category III Current Procedural Terminology (CPT) codes for the emerging technology, there is the chance that Medicare eventually will eventually cover it. In the meantime, Dr Ballard advises institutions to get “creative” when it comes to covering their costs.
At Barnes-Jewish Hospital and St Louis Children’s Hospital where he currently practices, Dr Ballard says 3D printing price tiers are based on the length of time, level of difficulty, and other factors associated with generating a given 3D model. These charges are then folded into the diagnosis-related group charge for surgery.
Healthcare systems would also do well to look beyond the direct financial returns on their investment in 3D printing, as it can result in savings associated with faster surgical procedures and shorter patient recovery times.
“When the surgeons have planned it out ahead of time [with 3D printed models], the outcomes are better, the surgery is faster, so they improve turnaround and recovery times and save money,” Duke’s Churchill says.
Benefits like these have sparked efforts by major radiological groups to have 3D printing approved for reimbursement. The Radiological Society of North America and the American College of Radiology, for example, have partnered to establish a 3D printing clinical data registry, the goal of which is to provide the data needed to support the technology’s transition coverage under Category I CPT codes.
“The anecdotal evidence we see day to day is there, but the biggest challenge is making the time to establish the scientific evidence. This is something we need to improve in the community,” Dr Ballard says.
For her part, Dr Bastawrous remains optimistic that 3D printing will become a mainstay of radiology sooner rather than later. “As more clinical evidence showing the utility and benefits of 3D printing become available, category I (CPT) codes will be adopted, and reimbursement will follow,” she says.
Citation
K R.3D Printing: Bridging the Gap Between Radiologists and Surgeons. Appl Radiol. 2023; (3):30-31.
May 5, 2023