Emergency Head and Neck Radiology: Neck Infections
Images

Dr. McKellop is a Radiologist, Department of Radiology, NYU Langone Medical Center/Bellevue Hospital Center, New York, NY. Dr. Mukherji is Professor and Chief of Neuroradiology in the Department of Radiology at the University of Michigan, Ann Arbor, MI. Dr. Mukherji is also Professor of Radiology, Otolaryngology Head and Neck Surgery, Radiation Oncology, Periodontics and Oral Medicine in the University of Michigan Schools of Medicine and Dentistry, Ann Arbor, MI.
Emergency neck infections are diverse in both their presentation and their affected patient population; pathology ranges from a transient enlargement of a child’s cervical lymph node to a rapidly spreading necrotizing fasciitis in an adult diabetic. Despite the widespread availability of antibiotics and early surgical intervention, deep neck infections still present significant morbidity and mortality in clinical centers. Complex neck anatomy can frequently obscure or delay diagnoses, so timely and appropriate radiological interpretation are critical to patient care. This article will review common neck infections that may be encountered in the emergency setting and detail some of their most salient findings on imaging.
Infections of the lymph node
In children, enlarged cervical lymph nodes are most commonly due to an associated infectious process rather than malignancy. A variety of infectious and non-infectious processes may cause enlargement of the cervical lymph nodes. The stimulated node is often referred to as “reactive.” Ongoing and untreated infection may eventually result in necrosis of the node leading to suppurative adenitis.
Cervical adenitis
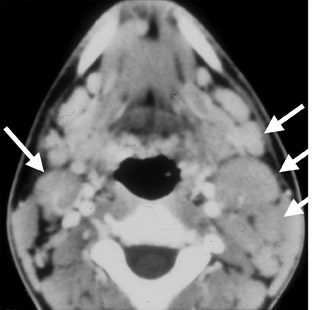
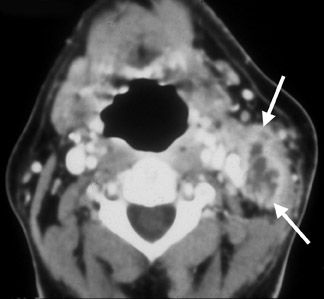
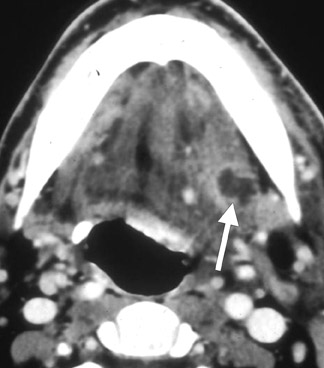
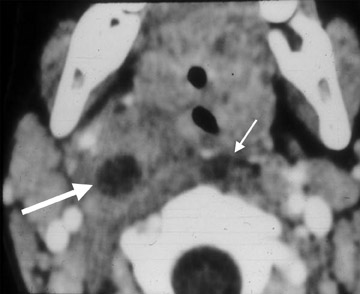
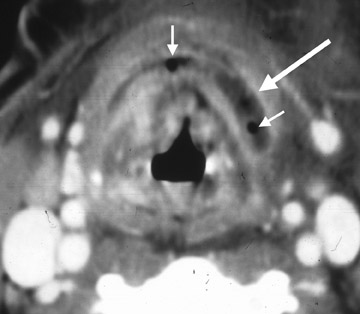
The term cervical adenitis denotes an inflammation of the lymph nodes due to an infectious process (Figure 1A) Suppurative adenitis indicates an infected node which has undergone liquefaction necrosis (Figure 1B). The likelihood of developing cervical adenitis, especially suppurative forms, decreases with age, although, the incidence of suppurative adenitis is increasing in older patients.
The most common cause of lymph node enlargement in children is a benign viral infection of the upper respiratory tract.1 Young adults with infectious mononucleosis, also present with generalized lymphadenopathy, along with complaints of weakness, fever and malaise. Another noteworthy viral infection is the acquired immunodeficiency syndrome (AIDS), which is caused by human T-cell lymphotropic virus type III (HTLV-III), and is a potentially devastating disease of childhood. Symptoms include localized or generalized lymphadenopathy, thrush, parotid swelling, interstitial pneumonitis, hepatosplenomegaly, and diarrhea.
Bacterial infections are the most common cause of suppurative cervical adenitis with staphylococcus aureus (S. aureus) and group A streptococcus bacterium (Streptococcus pyogenes) being the most common etiologic agents.2,3 Infected patients typically present with fever and upper respiratory tract infections. Early in the course of infection, discrete nodes are palpated. With uncontrolled infection, the firm nodes are replaced by a palpable fluctuant mass (suppurative adenitis), which may require drainage.
Computed tomography (CT) is the preferred modality to evaluate patients suspected of having cervical lymphadenitis. Early involvement by infection is characterized by homogeneous enlargement, loss of the fatty hilum and increased enhancement of the involved lymph node on CT. Reticulation of the adjacent fat surrounding a suppurative lymph node, or the presence of a circumferential rim of soft tissue, may be indicative of an inflammatory etiology as the cause of the abnormal node—as opposed to metastases.
Cat-scratch disease
Cat-scratch disease (CSD) is a very common cause of enlarged cervical lymph nodes in the pediatric age group and has been reported to be the cause of ≤73% of head and neck masses in children in which the diagnosis was subsequently confirmed by biopsy. The disorder is caused by the bacteria Bartonella henselae and usually presents within 3 to 10 days following contact. A prior history of a cat scratch is present in 72% of cases. Clinically, these patients present with tender, enlarged cervical lymph nodes, fever, and malaise. Approximately 10% of patients develop overlying erythema and fluctuant lymph nodes that require drainage.
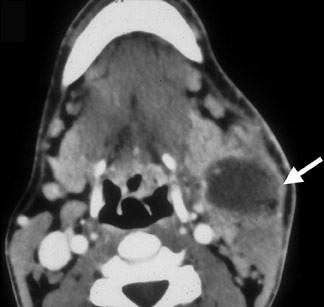
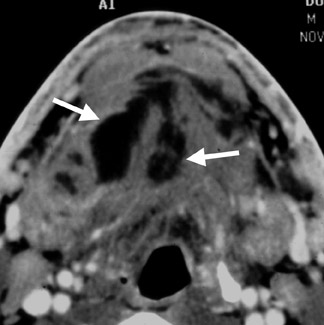
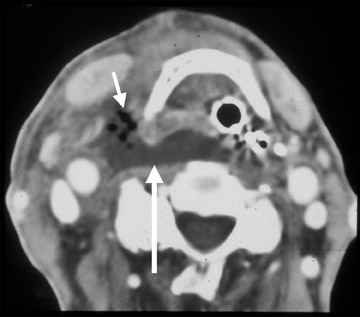
The typical findings on CT are a unilateral clumped group of enlarged lymph nodes clustered in the primary echelon drainage of the site of contact. Central areas of decreased attenuation within the lymph nodes are rare (Figure 2). There may be some subtle reticulation of the fat surrounding the lymph nodes, however, gross findings of extracapsular extension are rare. On magnetic resonance imaging (MRI), the signal characteristics are nonspecific and can be seen in a variety of disorders. The nodes typically enhance with contrast and contain high T2 signal.
Tuberculous lymphadenitis
There is a dramatic rise in the prevalence of tuberculosis in industrialized countries due to the AIDS epidemic, drug abuse and increased migration. The most common form of head and neck tuberculosis is lymphadenitis. Cervical lymphadenopathy is usually painless. Involvement is commonly bilateral and most frequently involves the internal jugular, posterior triangle and supraclavicular nodes. In advanced stages, the overlying skin may be inflamed and sinus tracts may appear.
Pathologically, tuberculosis typically shows tubercles with marked fibroblastic response. These tubercles show characteristic amorphous caseating necrosis which may rupture into surrounding structures, such as the airway and blood stream, causing endobronchial or hematogenous dissemination.
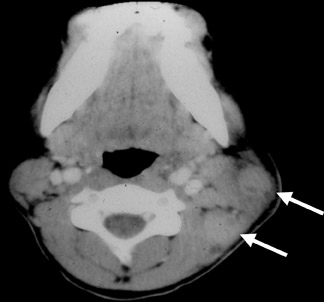
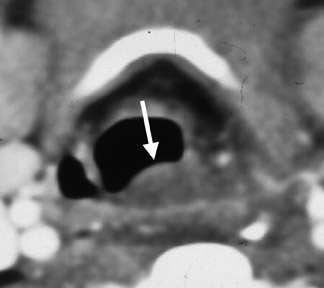
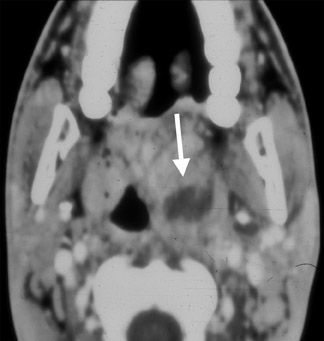
CT imaging of the early stages of tuberculous lymphadenitis reveals nodes with homogeneous contrast enhancement. As the disease evolves, central necrosis can be detected as foci of low density associated with rim enhancement (Figure 3). Healed lesions and nodes undergoing chemotherapy may show calcifications.
MR imaging shows nonspecific homogeneous enhancement on T1-weighted (T1W) images and high signals on T2-weighted (T2W) images. In nodes undergoing necrosis, contrast-enhanced MR imaging shows rim enhancement with a central area of no enhancement representing caseating necrosis. These nodes typically show high signal intensity on T2W images. MR imaging, although helpful in demonstrating lymphadenitis, cannot detect nodal calcifications.
Sublingual space infections
The sublingual space (SLS) is located inferior to intrinsic muscles of the oral tongue, lateral to the genioglossus-geniohyoid complex and superomedial to the mylohyoid muscle. Anteriorly, it is related to the mandible. Posteriorly, the SLS communicates with the submandibular space (SMS) with no fascia separating these spaces.
Sublingual space abscess
Abscesses originating in this space are usually due to sublingual or submandibular duct stenosis or calculus disease. Dental infection or mandibular osteomyelitis may also extend into the SLS. The most commonly encountered organisms in SLS abscess formation are S. aureus and Streptococcus viridans.
Clinically, patients with SLS abscess usually present with pain, tenderness and swelling in the anterior floor of the mouth. There may be a history of salivary colic, recent dental disease or dental manipulation. Treatment of an SLS abscess should commence with antibiotic therapy followed by surgical drainage.
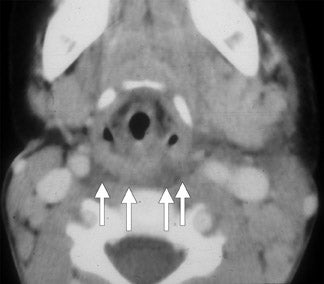
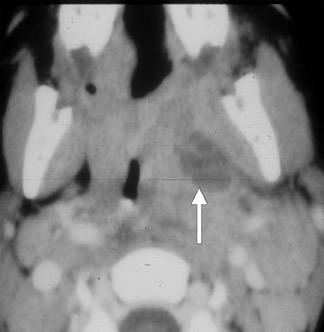
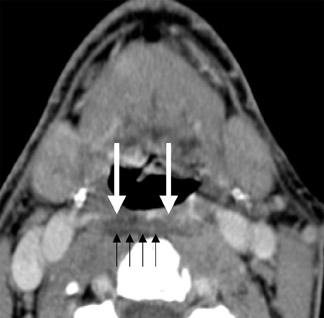
CT shows an enhancing mass involving the SLS associated with subcutaneous streaking and thickening of the platysma muscle. The genioglossus-geniohyoid complex is often displaced medially or across the midline (Figure 4). If an SMS component is present, this abscess may track into parapharyngeal space, where further spread can take place in the craniocaudal axis. Infection may also spread to the medial pterygoid or masseter muscles.
MR imaging is rarely used for inflammatory disease involving the floor of the mouth. A floor-of-the-mouth abscess shows the typical enhancing mass on T1W images and high signal intensity on T2W images. In contrast-enhanced images, a central area of no enhancement, indicating pus collection, can readily be demonstrated. Mandibular marrow edema is more readily demonstrated on MR as intermediate signal tissues replacing high signal intensity fat on T1W images.
Ludwig’s angina
The term “Ludwig’s angina” refers to cellulitis involving the floor of the mouth. This infection is usually due to streptococcus or staphylococcus species. Patients usually present with pain, tenderness and swelling of the mouth floor. The infection is usually precipitated by an odontogenic infection.4 In neglected cases, Ludwig’s angina may spread inferiorly through fascial planes into the mediastinum. Hence, some patients may present with chest pain.
Securing a patent airway is an important aspect of the management of this entity along with IV antibiotics and, if necessary, surgical drainage of secondary abscesses.5
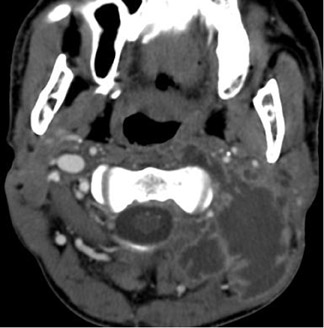
Contrast-enhanced CT shows swelling of the floor of the mouth (Figure 5). This finding is frequently associated with streaky changes in the adjacent subcutaneous fat and thickening of the overlying platysma muscle. Enlargement of the submental or submandibular lymph nodes may also be seen. In late cases, pus or gas formation may take place and the airway may be compressed.
Contrast-enhanced MR images show a thickened floor of the mouth with strong enhancement. On T2W images, diffuse high signals are evident in the floor of the mouth and adjacent soft tissues.
Neck infections
Retropharyngeal space infections
In adults, infection of the retropharyngeal space is usually due to a penetrating injury. Gram-positive cocci are the most common pathogen implicated in such cases.6 In children, however, retropharyngeal space infections are most commonly due to an upper respiratory tract infection. Acute pharyngitis is common in childhood and affects children usually <3 years of age. The causal organism is usually Hemophilus influenzae. From the pharynx, microorganisms can spread to the retropharyngeal nodes resulting in suppurative adenitis. If treatment is delayed, suppurated lymph nodes may rupture and result in the formation of retropharyngeal abscess or retropharyngeal cellulitis. Clinically, patients with retropharyngeal space infection often present with fever, neck pain, sore throat and neck mass.7 The patients may also complain of a choking feeling and difficulty in swallowing. Inspection of the pharynx will reveal edema and redness.
On imaging, plain film typically demonstrates thickening of the soft tissues in the prevertebral space. This is a nonspecific finding and may be seen in retropharyngeal cellulitis, retropharyngeal suppurative adenitis, or retropharyngeal abscess.
On CT, retropharyngeal cellulitis is identified by symmetric low attenuation in the retropharyngeal space (Figure 6). There is some anterior displacement of the posterior wall of the pharynx from the prevertebral muscles. However, the symmetric displacement does not exceed more than a few millimeters. Retropharyngeal suppurative adenitis is identified by enlarged paramedian retropharyngeal lymph nodes that contain a low-attenuation center (Figure 7). A retropharyngeal abscess is identified by a low-attenuation fluid collection that causes substantial anterior displacement of the posterior wall of the pharynx from the prevertebral muscles (Figure 8). This collection may be asymmetric. Retro-pharyngeal abscesses usually do not have a thick enhancing wall.
On MR, enlarged retropharyngeal nodes show intermediate signal intensity on T1W images and strong contrast enhancement. Rim enhancement indicates the presence of suppurative lymphadenitis. On T2W images, the inflamed nodes show high signal intensity. Soft-tissue thickening, as a result of cellulitis, also shows strong contrast enhancement and high signals on T2W images.
Tonsillar abscess
In contrast to acute tonsillitis, which is more common in children, a tonsillar abscess is more common in young adults. The average age is 25 years with >65% of patients falling between 20 and 40 years of age. The most common symptoms are sore throat, dysphagia, fever and trismus. Almost all patients have a history of recurrent pharyngitis. Management typically includes incision and drainage with antibiotic coverage.8
CT should be used to evaluate a suspected tonsillar abscess because it is quicker and cheaper than MRI. CT shows an enhancing mass in the tonsillar fossa that may or may not show pus formation (Figure 9). Extension into the parapharyngeal space may involve the medial pterygoid muscles (leading to trismus). In extensive disease, the inflammatory process may spread posterolaterally to involve the carotid sheath. It is important to evaluate this entity for possible jugular vein thrombosis or carotid artery erosion.
Parapharyngeal abscess
The parapharyngeal space is the area within the deep neck medial to the masseter muscle and lateral to the superior pharyngeal constrictor. It is divided into anterior and posterior compartments by the styloid process, the latter of which contains the carotid artery and internal jugular vein. An abscess in this space may arise from direct extension of infection from the pharynx through the pharyngeal wall, as a consequence of odontogenic infection, local trauma, and occasionally peritonsillar abscess.9 Diabetes is the most common systemic condition predisposing one to parapharyngeal abscess.
Patients with parapharyngeal abscess often present clinically with fever, sore throat and neck swelling. Erythema, odynophagia, and dysphagia often accompany such infections.10 Trismus is most commonly associated with anterior compartment abscesses.
On imaging, plain film findings are typically nonspecific and include thickening of the soft tissues in the prevertebral space and loss of cervical lordosis. Contrast-enhanced CT is the examination of choice to diagnose parapharyngeal abscess. CT shows a single or multiloculated low-density lesion with an air and/or fluid center (Figure 10). Contrast-enhanced sequences may occasionally demonstrate enhancement of the abscess wall.
Necrotizing fasciitis
Cervical necrotizing fasciitis is a rapidly spreading bacterial infection of the soft tissue that can quickly become a life-threatening condition. It is commonly caused by either streptococcal or polymicrobial infections. However, methicillin-resistant S. aureus (MRSA) species have been seen with increasing prevalence.11 Patients commonly present with high fevers and appear acutely ill. The overlying skin of the affected tissue may be erythematous and tender. One might appreciate crepitus with gas-producing bacterium. Patients with necrotizing fasciitis are best managed in the ICU and are typically treated with parenteral antibiotics and frequent surgical debridement.12
CT imaging will reveal nonspecific findings of diffuse reticulation of subcutaneous fat along with thickening and enhancement of the platysma. One may also find multiple abscesses extending along the fascial planes. Presence of gas within the soft tissue in the absence of prior surgery or radiation therapy is pathognomonic for necrotizing fasciitis (Figure 11).
Bezold’s abscess
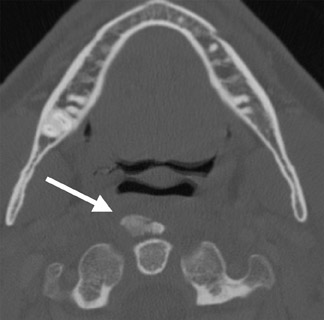
A Bezold’s abscess is a rare complication of otomastoiditis characterized by necrosis of the mastoid tip and spread of infection from bone to the adjacent soft tissue. Inflammatory collections form inferior to the mastoid process and may course along the plane of the sternocleidomastoid muscle to the lower neck. If left untreated, the abscess may spread as far as the larynx and mediastinum which results in poor prognosis. Clinically, patients present with fever, neck pain, restricted neck motion, and otalgia. Since the secondary abscesses lie deep to the superficial fascial planes surrounding the sternocleidomastoid and trapezius muscles, the fluctuance and contours may be difficult to palpate, clinically.13
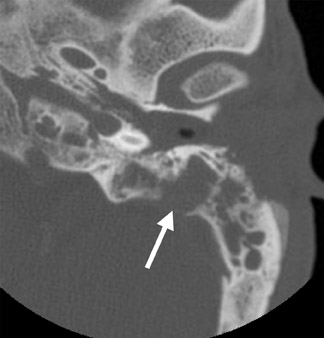
On CT imaging, one can appreciate unilateral opacification of the middle ear and mastoid cavities, often associated with bone erosion especially of the mastoid tip (Figure 12A). The abscess involves the adjacent musculature surrounding the mastoid and extends inferiorly (Figure 12B).9,14 Surrounding the abscess, one may notice obliteration of the fat planes, reticulation of the subcutaneous tissues and thickening of the overlying skin.
Other pathologies
Foreign body ingestion
Among other complications, inadvertent swallowing of foreign objects may result in retropharyngeal space infections, most notably, retropharyngeal abscess formation. Nearly 80% of all swallowed pharyngeal and esophageal foreign bodies take place in the pediatric population.15 However, adult patients who are stuporous, senile, or have psychiatric illness, are prone to swallowing a variety of foreign objects including animal bones and dentures. These objects are usually lodged in areas of normal anatomic narrowing in the cricopharyngeus area, the aortic arch or the distal esophagus. Sharp objects may perforate the pharynx or esophagus and migrate along tissue planes and compartments. This may result in abscess formation in the adjacent spaces such as the retropharyngeal space.
Children present clinically with respiratory distress, drooling or regurgitation but adults usually present with pain and dysphagia. Senile, psychiatric or stuporous patients may present late with evidence of fever or sepsis.
Non-contrast CT of the neck may be performed to confirm the presence or absence of an ingested foreign body. Contrast-enhanced CT will demonstrate the site and level of the resultant inflammation or abscess. Frequently, gas translucencies are detected within the retropharyngeal space. MR imaging is seldom used for foreign body ingestion as it cannot define reliably the presence of foreign body or gas collections.
Calcific tendinitis
Calcific tendinitis is a benign inflammatory condition caused by deposition of hydroxyapatite in the tendon fibers of the longus colli muscles.16 Patients present clinically with either sudden onset or subacute pain in the neck and throat worsened by head movement and swallowing.17 Due to its rare occurrence, it is often mistaken, clinically, for traumatic injury, retropharyngeal abscess, or infectious spondylitis, causing patients to frequently undergo unnecessary tests and treatment. The condition, however, is self-limited and resolves after 1 to 2 weeks upon calcium resorption.
Lateral neck radiography may show extensive soft-tissue swelling between C1 through C4 with amorphous calcific deposits anterior to C1 and C2.18 Likewise, CT will demonstrate the same findings along with prevertebral edema – a finding that must be distinguished from that found within retropharyngeal space infection (Figure 13).
Though typically unnecessary for diagnosis, MRI will demonstrate a signal void anterior to C1 and C2 representing an amorphous calcification. Additionally, MR may demonstrate marrow edema in adjacent vertebrae.
Conclusion
Emergency head and neck infections are indeed diverse, requiring a thorough appreciation for neck anatomy and the imaging modalities used to investigate such pathology. While plain film, ultrasound and MRI certainly play their part in the investigation of inflammatory and infectious pathology of the neck, cross-sectional imaging with CT has a central role. In the emergency setting, timely interpretation of radiologic images is critical to the care of acutely ill patients, namely those with a threatened airway.
REFERENCES
- Peters T, Edwards K. Cervical lymphadenopathy and adenitis. Pediatr Rev. 2000;21:399-405.
- Baker CJ. Group B streptococcal cellulitis-adenitis in infants. Am J Dis Child. 1982;136:631-633.
- Dajani AS, Garcia RE, Wolinski E. Etiology of cervical lymphadenitis in children. N Engl J Med. 1963;268:1329-1333.
- Weed HG, Forest LA. Deep neck infection. In: Cummings CW, Flint PW, Harker LA, et al, eds.Otolaryngology: Head and Neck Surgery, vol. 3. 4th edition. Philadelphia, PA: ElsevierMosby;2005: 2515-2524.
- Bross-Soriano D, Arrieta-Gomez J, Prado-Calleros H, et al. Management of Ludwig’s angina with small neck incisions: 18 years experience. Otolaryngol Head Neck Surg. 2004;130:712-717.
- Brook I. Microbiology and management of peritonsillar, retropharyngeal, and parapharyngeal abscesses. J Oral Maxillofac Surg. 2004;62:1545-1550.
- Craig FW, Schunk JE. Retropharyngeal abscess in children: Clinical presentation, utility of imaging, and current management.Pediatrics. 2003;111:1394-1398.
- Johnson RF, Stewart MG. The contemporary approach to diagnosis and management of peritonsillar abscess. Curr Opin Otolaryngol Head Neck Surg. 2005;13:157-160.
- Glynn F, Skinner LJ, Riley N, Donnelly M. Parapharyngeal abscess in an insulin dependent diabetic patient following an elective tonsillectomy. J Layngol Otol. 2007;121:e16. Epub.
- Page C, Biet A, Zaatar R, Strunski V. Parapharyngeal abscess: Diagnosis and treatment. Eur Arch Otorhinolaryngol. 2008;265:681-686.
- Smouha EE, Levenson MJ, Anand VK, Parisier SC. Modern presentations of Bezold’s abscess. Arch Otolaryngol Head Neck Surg. 1989;115:1126-1129.
- Miller LG, Perdreau-Remington F, Rieg G, et al. Necrotizing fasciitis caused by community-associated methicillin-resistant Staphylococcus aureus in Los Angeles. N Engl J Med.2005;352:1445-1453.
- Castillo M, Albernaz VS, Mukherji SK, et al. Imaging of Bezold’s abscess. AJR Am J Roentgenol. 1998;171:1491-1495.
- Gaffney RJ, O’Dwyer TP, Maguire AJ. Bezold’s abscess. J Laryngol Otol. 1991;105:765-766.
- Digoy GP. Diagnosis and management of upper aerodigestive tract foreign bodies. Otolaryngol Clin North Am. 2008;41:485-496.
- Vieira F,Allen SM, Stocks RM, Thompson JW. Deep neck infection. Otolaryngol Clin North Am.2008;41:459-483, vii.
- Eastwood JD, Hudgins PA, Malone D. Retropharyngeal effusion in acute calcific prevertebral tendinitis: Diagnosis with CT and MR imaging. AJNR Am J Neuroradiol. 1998;19:1789-1792.
- Haun CL. Retropharyngeal tendinitis. AJR Am J Roentgenol. 1978;130:1137-1140.