Complex Extraspinal Musculoskeletal Interventions: Role of 4D CT (Angio-CT) in Planning and Treatment
Percutaneous musculoskeletal ablation and/or cementoplasty may be used to evaluate a variety of conditions ranging from osteoporotic fractures to osteolytic metastases. This wide applicability and implied range of patient dispositions necessitates robust techniques that allow for precise imaging of local structure, as well as methods to approximate the volume occupied by the injected matrix.
Current conventional approaches to extraspinal procedures utilize either computed tomography (CT) or fluoroscopy, which provide precise anatomical information and real-time imaging, respectively.2 This article presents examples of how 4D CT (Angio-CT) fluoroscopy may further aid needle guidance and polymethylmethacrylate (PMMA) injection in complex cases.
The CT-only approach is typically the most convenient; this approach offers sufficient detail within a given plane to assess positioning prior to injection. However, it presents challenges in cases that also require real-time imaging and significant maneuverability along the Z-axis.1
Fluoroscopic procedures, on the other hand, are limited in their ability to appreciate complex anatomy situated within the pelvis, a growing space for percutaneous interventions owing to the morbidity of open surgical treatment in this area.3 Despite this limitation, live, real-time imaging is crucial to ensure adequate cement penetration. Although cone beam CT (CBCT) may serve as a third option for real-time imaging and generating 3D reformatted images, widespread and successful complex acquisitions or reconstructions remain elusive.4
Angio-CT allows for rapid transition to live fluoroscopic imaging following CT-guided needle placement. The correct placement may be confirmed using oblique, sagittal, and coronal reformats of intraprocedural CT images, reducing the need for gantry repositioning and angulation during the procedure. This method also allows for optimal needle placement, more in plane with the long axis of the lesion to take advantage of the oblong ablation zones of most thermal ablation systems.
Angio-CT also can be used for subsequent 3D reconstruction following a switch to fluoroscopy. This approach may also increase operative efficiency and reduce the need for repeat CT to confirm needle placement. Post-injection CT also visualizes small polymer leaks that may not be immediately apparent on fluoroscopy because of insufficient visualization of soft tissues and neurovascular structures. Additionally, rapid transition to fluoroscopy during cement injection directly reveals PMMA distribution over time and immediately identifies leakage. This offers the opportunity to leverage the strengths of each modality throughout the procedure.
In addition to the advantages outlined above, Angio-CT also offers the benefits of multiplanar imaging with real-time visualization of matrix injection and delivers spatiotemporal information to help address the limitations of alternative approaches. Additionally, it helps to establish postoperative treatment plans and enhance workflow efficiency through timely transitioning between modalities. However, Angio-CT is not without its weaknesses; these include the risk of increased radiation exposure and image quality that largely depends on the patient’s ability to remain motionless during the acquisition.6,7 Therefore, continued efforts to attenuate exposure and refine image acquisition techniques are pivotal to advancing the viability of the modality in these procedures.
Two examples, a pelvic and glenoid cementoplasty performed using a 4D CT system (Canon Medical Systems USA, Inc.) are outlined below.
Case 1
Pelvic cementoplasty using 4D CT fluoroscopy in a 65-year-old patient with hepatocellular carcinoma and oligometastatic lesion to the iliac bone.
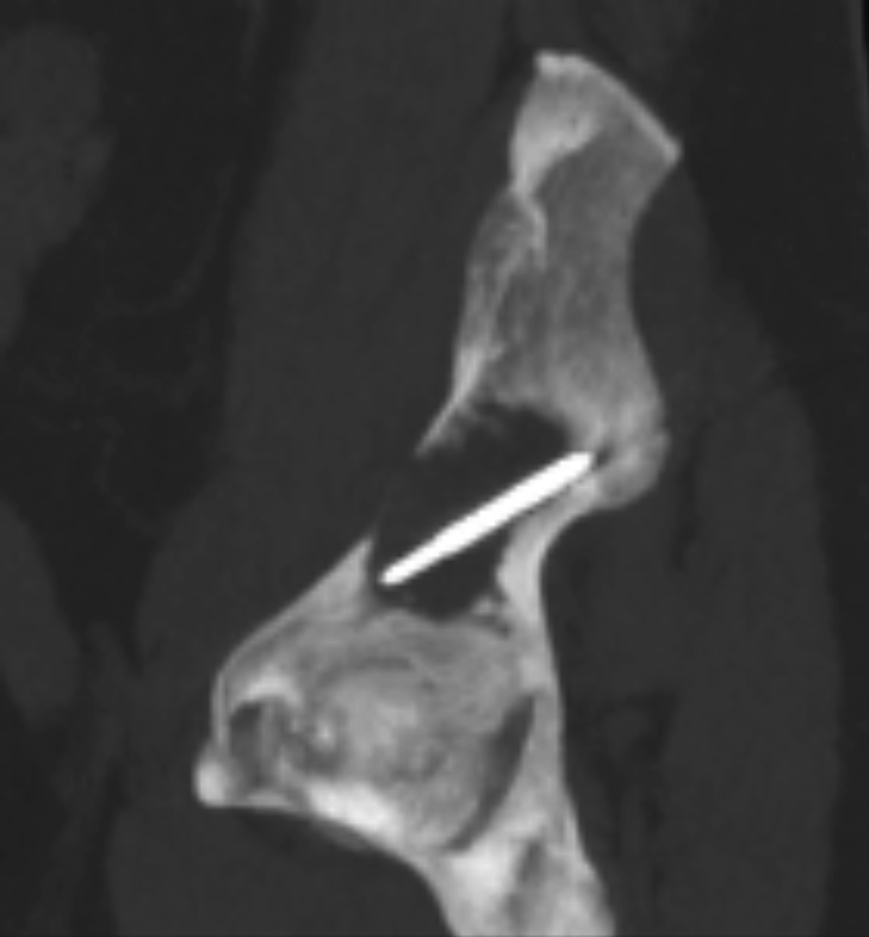
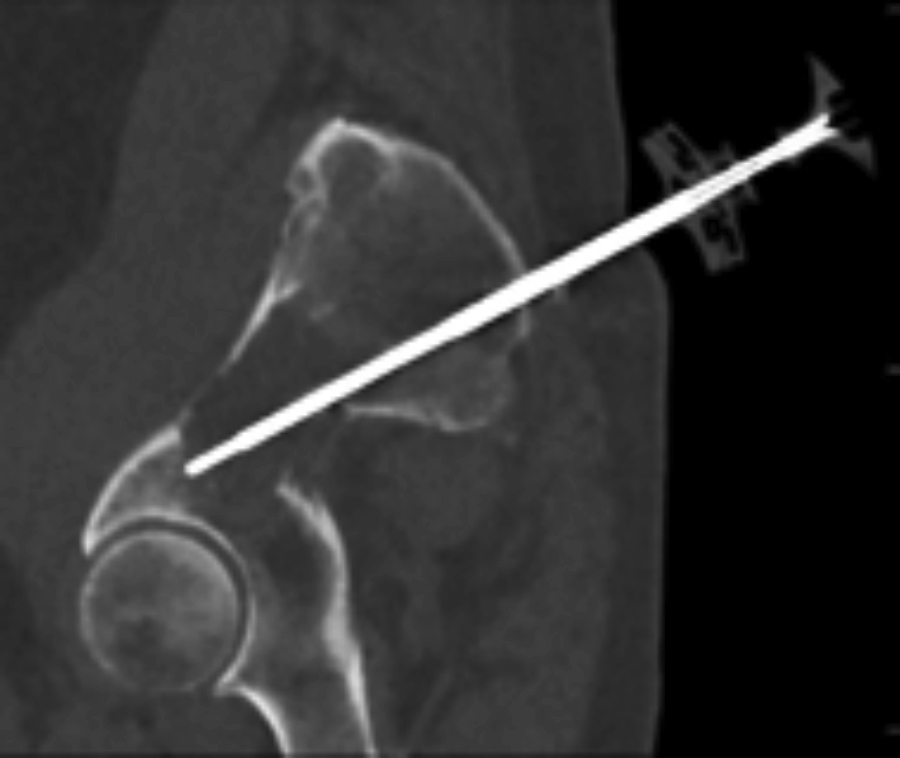
Figure 1. Oblique sagittal reformats demonstrate the ability to use 4D CT to guide needle placement along the long axis of the lesion for thermal ablation.
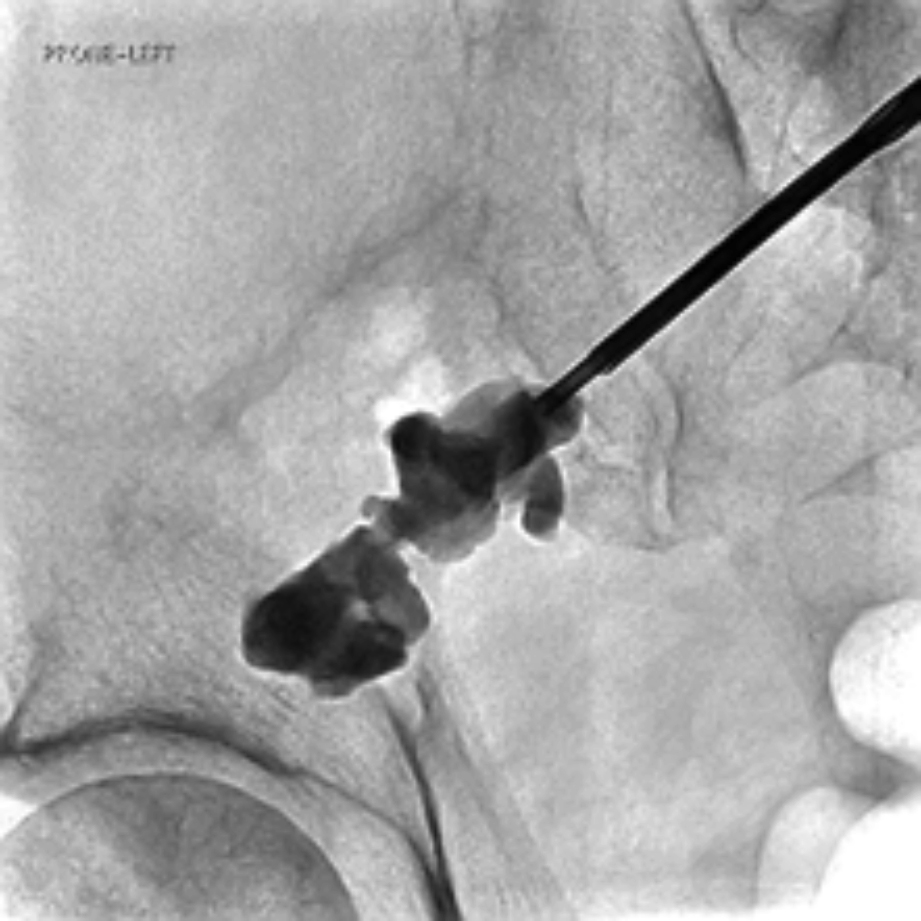
Figure 2. Conversion to live fluoroscopy permits cementoplasty following CT-guided placement (shown in Figure 1) and real-time monitoring for cement leakage.
Case 2
Glenoid cementoplasty in 56-year-old patient with cholangiocarcinoma and metastatic lesion to the glenoid.
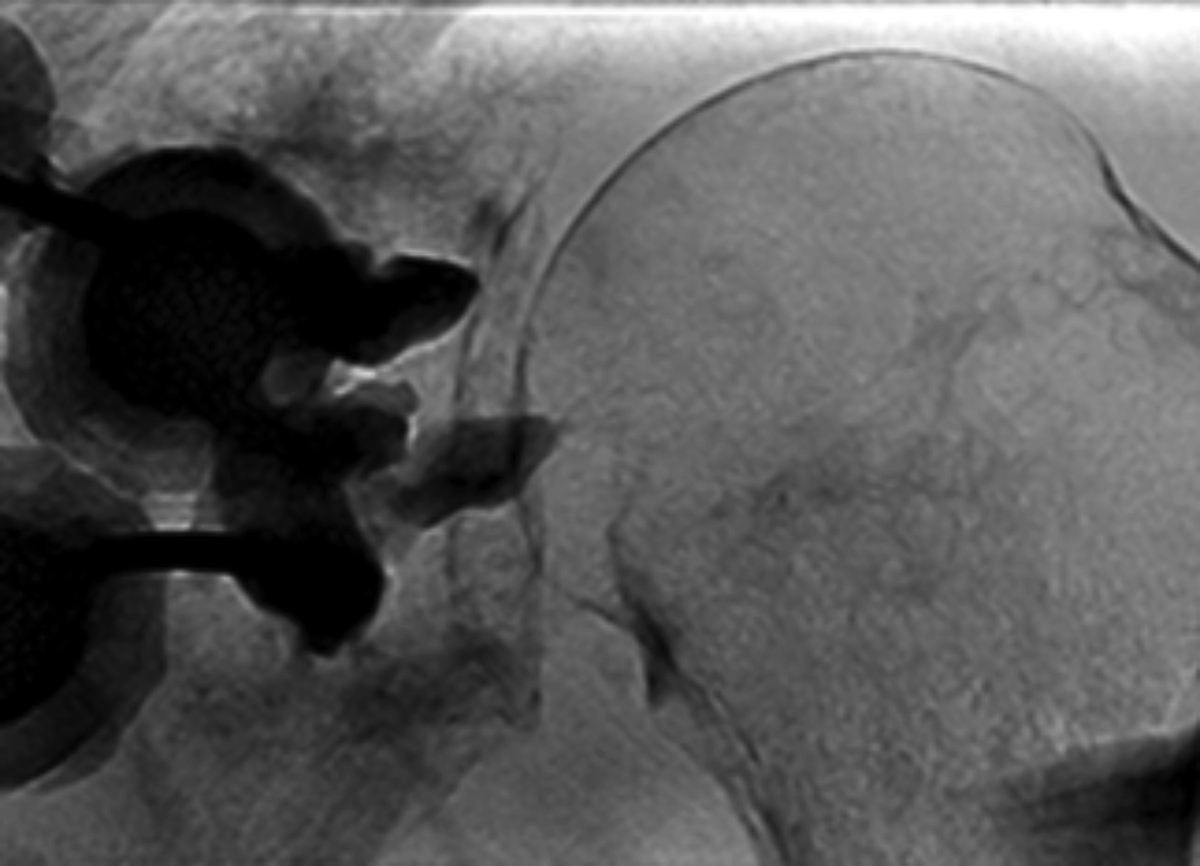
Figure 1. Fluoroscopy of glenoid cementoplasty with suspicion of cement leakage into joint space.
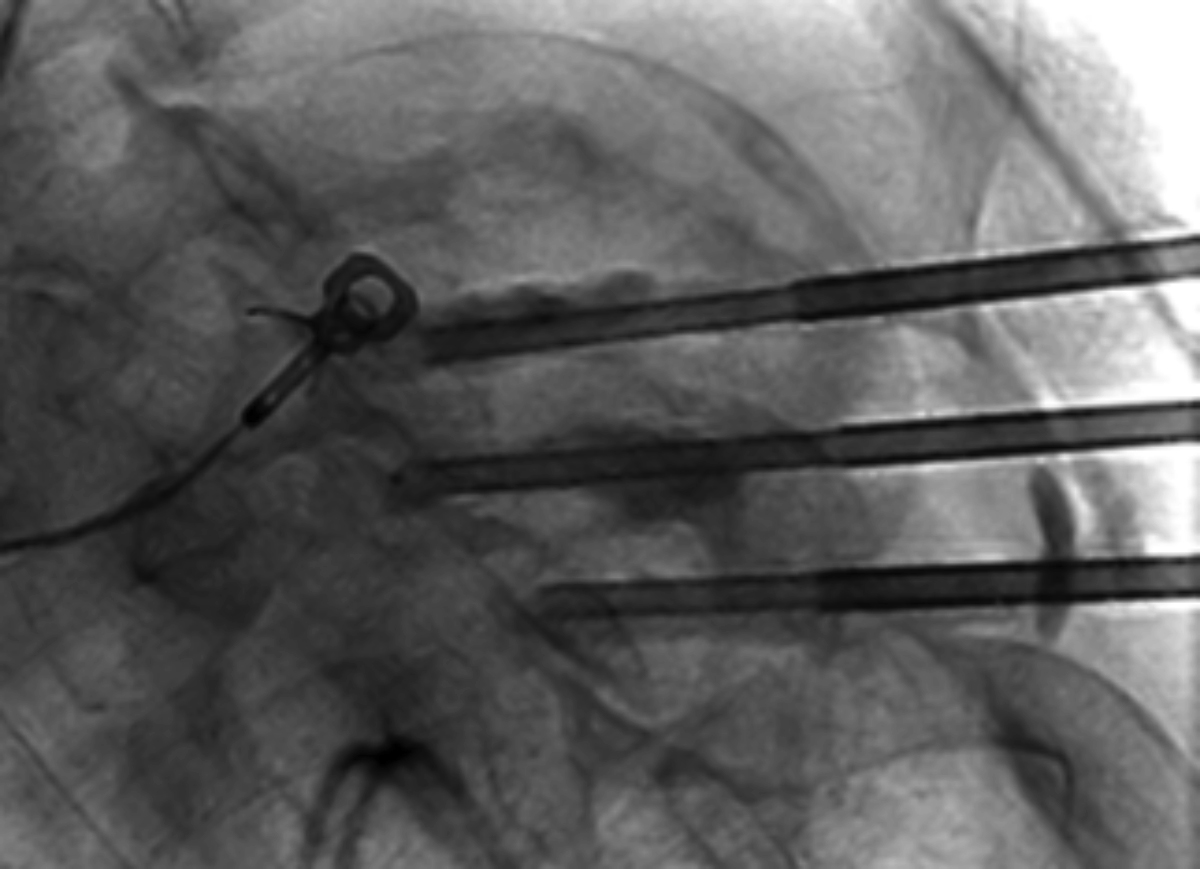
Figure 2. Orthogonal view of cementoplasty, providing minimal additional information with regard to extent of potential leakage.
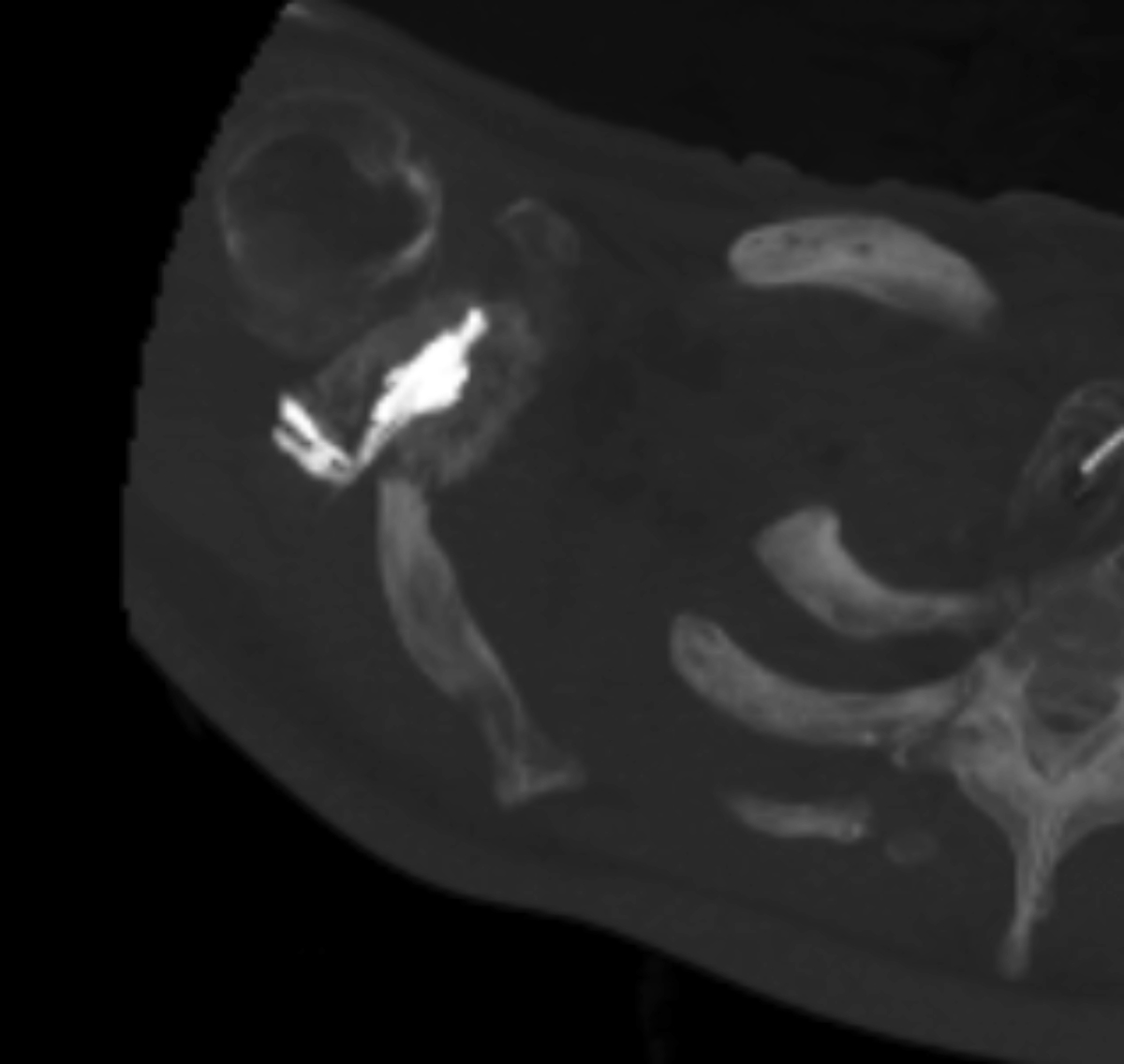
Figure 3. Immediate conversion to intraprocedural CT displays apparent distribution of leakage into posterior soft tissue. This indicates the optimal endpoint for cement fill.
References
- Oñate Miranda M, Moser TP. A practical guide for planning pelvic bone percutaneous interventions (biopsy, tumour ablation and cementoplasty). Insights into Imaging. 2018; 9(3): 275–285. https://doi.org/10.1007/s13244-018-0600-y
- Yevich S, Tselikas, L Gravel G, de Baère T, Deschamps F. Percutaneous Cement Injection for the Palliative Treatment of Osseous Metastases: A Technical Review. Seminars in Interventional Radiology. 2018; 35(4), 268–280. https://doi.org/10.1055/s-0038-1673418
- Vaidya R, Scott AN, Tonnos F, et al. Patients with pelvic fractures from blunt trauma. What is the cause of mortality and when? Am J of Surg. 2016; 211(3), 495–500. https://doi.org/10.1016/j.amjsurg.2015.08.038
- Roux C, Tselikas L, Yevich S, et al. Fluoroscopy and Cone-Beam CT-guided Fixation by Internal Cemented Screw for Pathologic Pelvic Fractures. Radiology, 2019; 290(2), 418–425. https://doi.org/10.1148/radiol.2018181105
- Kelekis A, Lovblad KO, Mehdizade A, et al. Pelvic osteoplasty in osteolytic metastases: Technical approach under fluoroscopic guidance and early clinical results. J Vasc Interv Radiol. 2005; 16(1), 81–88. https://doi.org/10.1097/01.rvi.0000141717.84515.92
- Coolens C, Bracken J, Driscoll B, Hope A, Jaffray D. Dynamic volume vs respiratory correlated 4DCT for motion assessment in radiation therapy simulation. Medical Physics. 2012; 39(5), 2669–2681. https://doi.org/10.1118/1.4704498
- Kwong Y, Mel AO, Wheeler G, Troupis JM. Four-dimensional computed tomography (4DCT): A review of the current status and applications. J Med Imag Rad Oncol. 59(5), 545–554. https://doi.org/10.1111/1754-9485.12326
