The Many Faces of Facial Trauma
By Omami G




Facial fractures are common sequelae of assaults, traffic accidents, and sporting accidents;1,2 radiologists and surgeons must have a detailed understanding of facial anatomy, biomechanics, and occlusion.3 To this end, radiologic examination is essential to the diagnostic evaluation of facial trauma, as it helps accurately identify and characterize fractures and associated complications.
CT is the imaging modality of choice with respect to evaluating mid- and upper-facial injuries, as it has the advantage of providing multiplanar and three-dimensional visualization of the craniofacial structures.4 However, for mandibular fractures, two plain or projection images taken at right angles to one another are often necessary to visualize displacements (eg, panoramic and posteroanterior views).4
This article provides an overview of the common patterns of facial fractures based on the concept of facial buttresses, with the goal of simplifying diagnosis of these injuries.
Anatomy of the Facial Buttresses
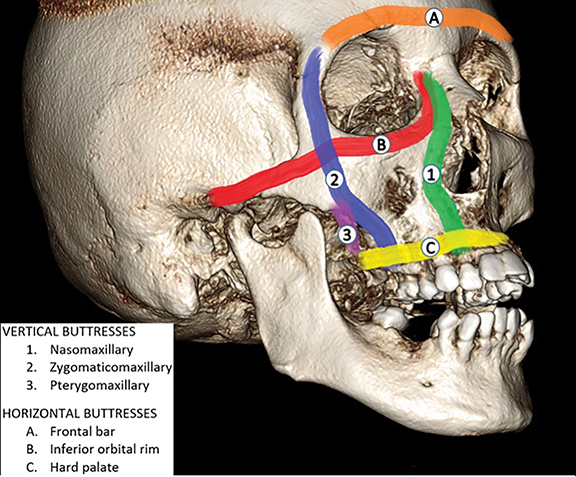
The facial skeleton can be conceptualized in terms of the supporting struts or buttresses that serve as structural pillars for the midface. The concept of facial buttresses helps identify key areas of fracture, necessitating surgical fixation for restoration.5 Fixation is typically performed by using rigid titanium plates and screws anchored in the buttress.
There are three paired vertical and three transverse buttresses (Figure 1). The vertical buttresses include (1) the lateral wall of the pyriform aperture and the medial orbital wall (nasomaxillary buttress), (2) the lateral wall of the maxilla, the body of the zygoma, and the lateral orbital wall (zygomaticomaxillary buttress), and (3) the maxillary tuberosity and the pterygoid process (pterygomaxillary buttress). The transverse buttresses include the superior orbital rim and the floor of the anterior cranial fossa (frontal bar); the inferior orbital rim, the orbital floor, and the zygomatic arch (upper transverse maxillary buttress); and the maxillary alveolar process and the hard palate (lower transverse maxillary buttress).
Mandibular Fractures
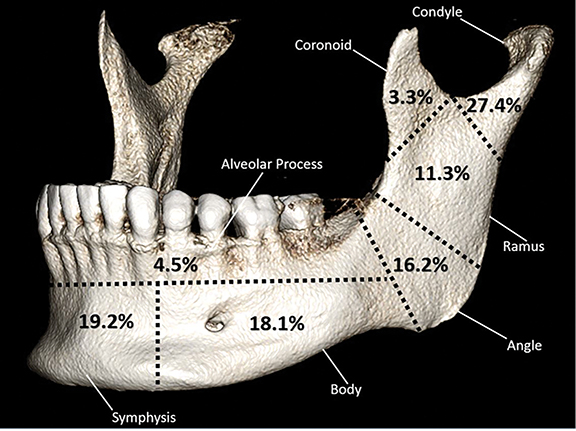
Because of the U-shape of the mandible, forces applied to a single area of the bone often results in simultaneous fractures. Six distinct regions of the mandible are commonly fractured: the condyle/condylar neck, ramus, angle, body, symphysis, and alveolar process (Figure 2).
Common patterns of simultaneous fractures include those of the angle with the contralateral condylar neck, bilateral angle fractures, angle with the contralateral body, and symphyseal with bicondylar fractures (Figures 3, 4). Predominance of angle fractures is often related to the relative mandibular weakness in patients with impacted third molars. Bilateral symphyseal fractures can result in posterior displacement of the anterior mandibular segment, potentially allowing for posterior displacement of the tongue and airway embarrassment.7
Fractures of the mandible could be favorable or unfavorable, depending on the angulation of the fracture line in relation to the vector of muscle pull. In a favorable fracture, the muscle pull tends to splint the fractured segments in place. In an unfavorable fracture, the muscle pull tends to draw the fractured segments apart (Figure 5).
Another classification of mandibular fractures categorizes fractures as simple (closed), compound (open), comminuted, and greenstick. A simple fracture occurs within a non-tooth-bearing segment of the mandible. A compound fracture results in communication with the oral or external environment through the gingival sulcus and periodontal ligament, or lacerations in the overlying skin or mucosa. Therefore, any fracture in a tooth-bearing area is essentially a compound fracture. In a comminuted fracture, the fractured bone is left in multiple fragments (eg, high-energy injuries). A greenstick fracture is an incomplete fracture involving only one cortical plate; this type usually occurs in children.
Mandibular fractures in children may be complicated by a disturbance of normal facial growth. Ankylosis of the temporomandibular joint occurs in 1–7% of condylar fractures.8 An oblique fracture that involves both cortical plates may appear on panoramic images as two lines that converge at the inferior border of the mandible, suggesting two separate fractures when in reality only one exists.
Midfacial Fractures
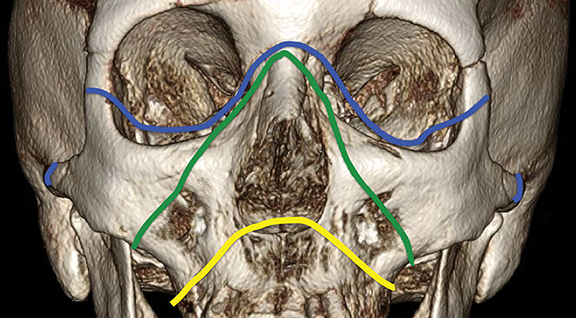
Midfacial fractures can be classified as Le Fort I, II, or III; zygomatic; or orbital blow-out fractures. These injuries may be isolated or occur in combination.9
Le Fort I Fractures
The Le Fort I fracture results from a horizontal blow to the body of the maxilla (Figure 6). This type of trauma may separate the maxilla in one piece from the middle face or split the palate (Figure 7). The fracture plane passes at a level just above the roots of the teeth and nasal floor, and then runs posteriorly through the maxillary sinus and the tuberosity to the pterygoid plates.
Le Fort II Fractures
Forces applied to the central facial region frequently result in a Le Fort II fracture, which is the separation of the maxilla and the attached nasal complex from the orbital and zygomatic structures (Figure 8). The fracture line extends through the root of the nose bilaterally to involve the medial and inferior orbital walls, and then runs down the zygomaticomaxillary suture and the lateral and posterior walls of the maxilla to the pterygoid plates. This creates a pyramid-shaped central midface fracture (Figure 6).
Le Fort III Fractures
A Le Fort III fracture results when horizontal forces are applied at a level superior enough to separate the entire facial skeleton from the skull base (craniofacial separation, Figure 9). The fracture line extends through the root of the nose bilaterally, across the medial orbital walls, and then posterolaterally across the orbital floors through the inferior orbital fissure to the lateral orbital walls; and then down across the posterior walls of the maxilla to the pterygoid plates. The zygomatic arches also are fractured, thereby completing facial skeleton separation from the cranial base (Figure 6).
Zygomatic Fractures
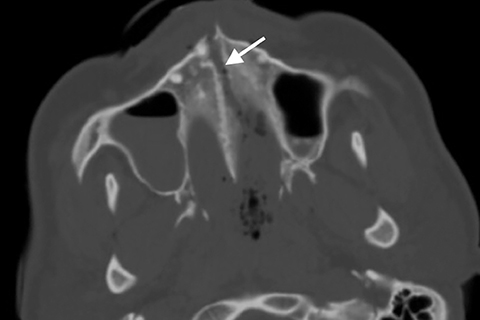
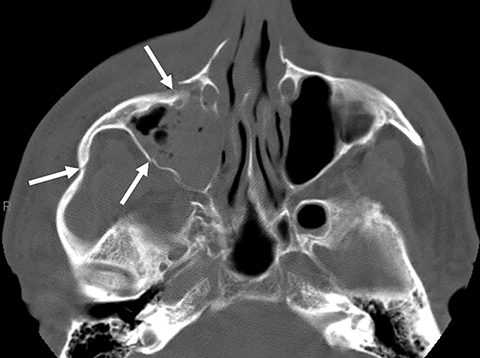
Zygomatic fractures are the second-most common midfacial fractures after nasal bone fractures, usually result from a direct blow to the prominence of the cheek. These injuries are commonly known as “trimalar,” “tripod,” or “zygomatico-maxillary complex” fractures. The zygoma is often disrupted at its articulations with the maxillary, frontal, temporal, and sphenoid bones (Figure 10).
Zygomatic fractures may extend to the orbital apex, resulting in a number of serious neurovascular injuries.10 A blow to the lateral midface may result in a depressed zygomatic arch fracture. Mandibular movement may be restricted if the displaced zygomatic bone impinges on the coronoid process.
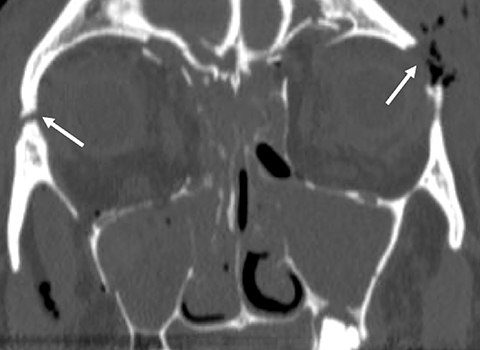
Orbital Blow-out Fractures
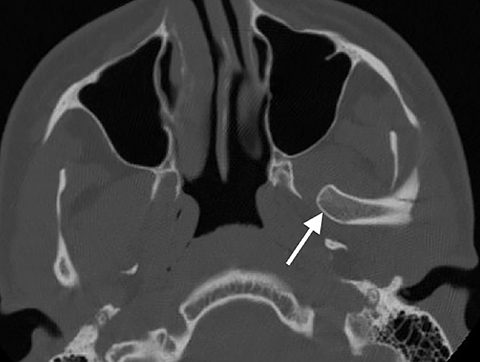
Blow-out fractures involve the orbital floor and/or medial wall. They result from direct blunt trauma to the orbit, such as from a fist or a baseball. The infraorbital rim is typically intact in blowout fractures. The periorbital fat may herniate through the bony defect into the adjacent maxillary or ethmoid sinus. Extraocular muscle (inferior or medial rectus) herniation may result in entrapment and restricted eye movement (Figure 11). The fracture and herniated tissue are best seen on coronal CT or coronal MR imaging. The fracture alone is best seen on coronal CT or coronal MR imaging; however, sensitivity for small fracture segments is considerably higher on CT.11
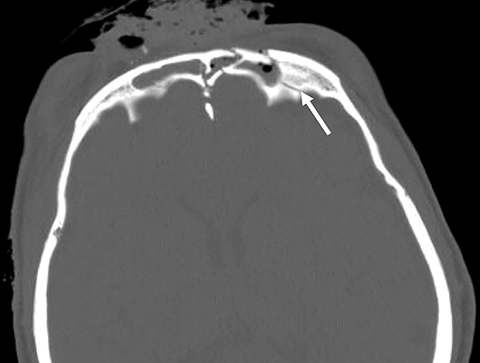
Frontal Sinus Fractures
Frontal sinus fractures are the result of either a direct blow or an extension of a skull fracture into the sinus. They comprise 5-15% of all facial fractures.10 The fracture line may extend inferiorly, involving the superior orbital rim. Dural tears and cerebrospinal fluid rhinorrhea may occur if the fracture extends along the floor of the anterior cranial fossa.
Axial CT imaging most clearly confirms the presence of frontal sinus fractures, which often are clinically unobserved because the fragment depression is obscured by soft tissue swelling (Figure 12). In non-displaced frontal sinus fractures, an intracranial pneumocele is a key feature indicative of posterior table involvement. If the nasofrontal duct is disrupted, surgical obliteration of the frontal sinus is necessary to prevent formation of a mucocele.10 Fractures involving the posterior table require neurosurgical consultation.
Conclusion
As practice trends increasingly favor rigid fixation to restore facial anatomy and function, treatment decisions are becoming more dependent on radiologic findings. Therefore, radiology reports should address facial injuries in clinical context with categorization by the need for surgical repair, rather than containing a “laundry list” of fractures. This requires a detailed knowledge of the anatomy and biomechanics of the maxillofacial skeleton.
Acknowledgement: The author thanks Barton Branstetter, MD, from the University of Pittsburgh, for providing Figures 4, 7-12.
References
- Iida S, Kogo M, Sugiura T, et al. Retrospective analysis of 1502 patients with facial fractures. Int J Oral Maxillofac Surg. 2001;30(4):286–290.
- Gassner R, Tuli T, Hachl O, et al. Cranio-maxillofacial trauma: a 10-year review of 9,543 cases with 21,067 injuries. J Craniomaxillofac Surg. 2003;31(1):51–61.
- Hopper RA, Salemy S, Sze RW. Diagnosis of midface fractures with CT: what the surgeon needs to know. Radiographics. 2006; 26(3):783-793.
- Avery LL, Susarla SM, Novelline RA. Multidetector and three dimensional CT evaluation of the patient with maxillofacial injury. Radiol Clin North Am. 2011;49(1):183–203.
- Linnau KF, Stanley RB Jr, Hallam DK, et al. Imaging of high-energy midfacial trauma: what the surgeon needs to know. Eur J Radiol. 2003; 48:17-32.
- Hanson BP, Cummings P, Rivara FP, et al. The association of third molars with mandibular angle fractures: a meta-analysis. J Can Dent Assoc. 2004;70(1):39-43.
- Dreizin D, Nam AJ, Tirada N, et al. Multidetector CT of mandibular fractures, reductions, and complications: A clinically relevant primer for the radiologist. Radiographics. 2016;36(5):1539-1564.
- Alcalá-Galiano A, Arribas-García IJ, Martín-Pérez MA, et al. Pediatric facial fractures: children are not just small adults. Radiographics. 2008;28(2):441-461.
- Bagheri SC, Holmgren E, Kademani D, et al. Comparison of the severity of bilateral LeFort injuries in isolated midface trauma. J Oral Maxillofac Surg. 2005;63(8):1123-1129.
- Fraioli RE, Branstetter BF 4th, Deleyiannis FW. Facial fractures: beyond Le Fort. Otolaryngol Clin North Am. 2008;41(1):51-76.
- Belli E, Matteini C, Mazzone N. Evolution in diagnosis and repairing of orbital medial wall fractures. J Craniofac Surg. 2009;20(1):191-193.
Affiliation: University of Kentucky College of Dentistry, Lexington, KY. Disclosure and Conflict of Interest: The author declares no conflicts of interest.
