Diffuse alveolar hemorrhage
By Kliewer B, Hull C, Yasmer J


CASE SUMMARY
A 29-year-old male with a history of recently diagnosed systemic lupus erythematosus presented to the ED with a 3-day history of hemoptysis and dyspnea. He also complained of weakness and bleeding gums. On physical exam the patient was in no acute distress with a soft, non-tender abdomen. He had normal pulses with 2+ bilateral lower extremity pitting edema. Hemoglobin at time of admission was 6.6 g/dL. The patient had a known history of lupus nephritis and was on hemodialysis for renal failure.
IMAGING FINDINGS
A portable chest radiograph at the time of presentation demonstrated mild cardiomegaly with diffuse interstitial opacities throughout both lungs suspicious for pulmonary edema (Figure 1).
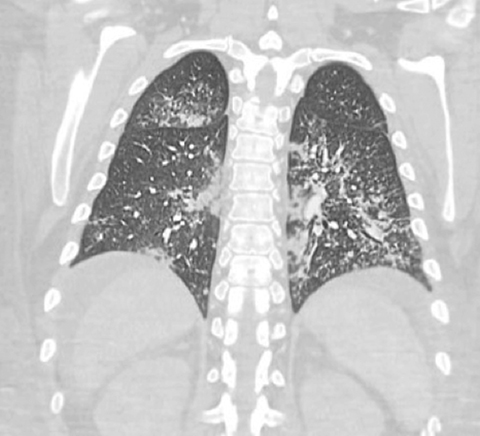
A CT of the chest was subsequently performed secondary to the patient’s hemoptysis. Given the patient’s history of SLE and anemia, there was concern for diffuse alveolar hemorrhage. CT showed diffuse mixed interstitial and alveolar opacities with diffuse interlobular septal thickening throughout both lungs (Figures 2, 3). The partial view of the abdomen demonstrated abdominal ascites and diffuse soft tissue anasarca consistent with the patient’s known history of lupus nephritis and renal failure.
DIAGNOSIS
Diffuse alveolar hemorrhage
DISCUSSION
Diffuse alveolar hemorrhage (DAH) is a clinicopathologic syndrome characterized by the accumulation of red blood cells within the alveoli arising from the alveolar capillaries. The syndrome is an often fatal, dreaded complication of systemic lupus erythematosus (SLE) with a median age at diagnosis of 27 years. It can be acute or subacute, occurring over hours to several days. The clinical syndrome usually includes hemoptysis, dyspnea, anemia, hypoxemic respiratory failure and anemia, with dyspnea being the most common presenting factor occurring in 74-100% of patients. DAH is frequently associated with SLE and has been reported to occur in 2-5% of all cases. It also has a strong association with lupus nephritis with evidence of active kidney disease in 64-100% of patients with lupus related DAH. Diffuse alveolar hemorrhage is typically defined by three major components: signs (blood on bronchoscopy) or symptoms (cough, hemoptysis, and dyspnea); a new drop in hemoglobin; new, diffuse infiltrates on imaging.
Diffuse alveolar hemorrhage occurs in three distinct but overlapping histologic patterns: pulmonary capillaritis, bland pulmonary hemorrhage, and diffuse alveolar damage. Pulmonary capillaritis consists of neutrophilic infiltration of the alveolar interstitium with fibrinoid necrosis of the alveolar and capillary walls. Nuclear debris accumulates within the interstitium with subsequent loss of the alveolar-capillary basement membrane which results in alveolar accumulation of red blood cells. Bland pulmonary hemorrhage presents with accumulation of fibrin and erythrocytes within the alveolar spaces with sparing of the alveolar structures. Lastly, diffuse alveolar damage consists of alveolar septal edema with formation of hyaline membranes. The predominate pattern seen in SLE is that of pulmonary capillaritis.
Mortality is reported to be as high as 50% but is declining with increasing awareness and aggressive treatment. Mortality is mainly attributable to respiratory complications. There are multiple treatment options available as appropriate treatment protocols have yet to be established due to the lack of prospective studies. Corticosteroids are the mainstay of therapy, but there are no reported guidelines for the dose or duration of therapy. The use of cyclophosphamide is controversial and has been linked to both increased survival as well as increased mortality rates. Plasmapheresis is commonly used for other autoimmune related causes of vasculitis related pulmonary bleeding but has not been proven effective for DAH associated with SLE. B-cell depletion has shown promising results but the available data is limited. One study of 6 patients with bronchoscopically confirmed DAH treated with activated recombinant factor VII showed decreased oxygen requirements and sustained hemostasis after treatment. The evidence to support any particular therapy is, therefore, limited.
CONCLUSION
DAH is a potentially deadly complication of SLE that needs timely diagnosis for early management. DAH should remain in the differential for patients with diffuse alveolar opacities, interlobular septal thickening, and a history of SLE, especially those with a history of hemoptysis and new onset anemia.
REFERENCES
- Lara, AR, et al. Diffuse Alveolar Hemorrhage. Chest. 2010; 137(5): 1164-1171. doi: 10.1378/chest.08-2084.
- Zamora MR, Warner ML, Tuder R, Schwarz MI. Diffuse alveolar hemorrhage and systemic lupus erythematosus. Clinical presentation, histology, survival and outcome. Medicine. 1997;76(3):192-202.
- Kazzaz NM, Coit P, Lewis EE, et al. Systemic lupus erythematous complicated by diffuse alveolar hemorrhage: Risk factors, therapy and survival. Lupus Science & Medicine. 2015;2:e000117. doi: 10.1136/lupus-2015-000117.
- Ta R, Celli R, and West AB. Diffuse Alveolar Hemorrhage in Systemic Lupus Erythematosus: Histopathologic Features and Clinical Correlations. Case Reports in Pathology. 2017; Article ID 1936282, doi:10.1155/2017/1936282.
- Singh Virdi RP, Bashir A, Shahzad G, Iqbal J, and Mejia JO. Diffuse Alveolar Hemorrhage: A Rare Life-Threatening Condition in Systemic Lupus Erythematosus. Case Reports in Pulmonology. 2012; Article ID 836017. doi: 10.1155/2012/836017.
- Heslet L, Nielsen JD, Levi M, et al. Successful pulmonary administration of activated recombinant factor vii in diffuse alveolar hemorrhage. Crit Care. 2006; 10(6):R177.
Prepared by Dr. Kliewer and Dr. Hull while PGY-4 Diagnostic Radiology residents, and Dr. Yasmer while serving as Assistant Program Director of Diagnostic Radiology, Hemet Valley Medical Center, Hemet, CA.
