White Matter Hyperintensities in Brain Are Not Biomarkers for mTBI on 3T MRI
Images
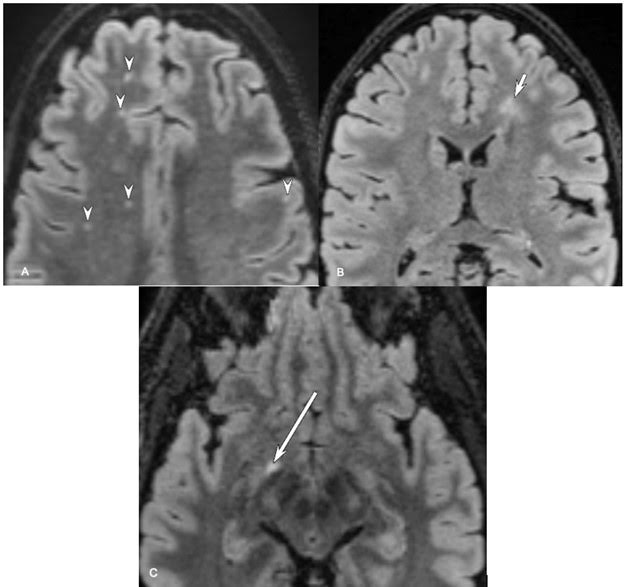
White matter hyperintensities (WMHs) are common on high-resolution FLAIR images at 3-T MRI and do not serve as a biomarker of mild traumatic brain injury (mTBI), according to research published in the American Journal of Roentgenology (AJR).
“WMHs did not show significant differences between mTBI and control groups, nor significant associations with clinical markers in the mTBI group,” clarified senior and corresponding author Teena Shetty, MD, MPhil, from the Hospital for Special Surgery in New York City.
Shetty et al. recruited individuals with acute mTBI and a matched control group of individuals without mTBI from seven U.S. centers (November 2015–January 2018). Participants underwent up to four clinical encounters (baseline through approximately 3 months after enrollment). At each encounter, clinical markers of head injury were tested, including the Rivermead Post-Concussion Symptoms Qustionnaire-3 (RPQ-3), assessing early postconcussive symptoms (physical symptoms), Rivermead Post-Concussion Symptoms Questionnaire-13 (RPQ-13), assessing late postconcussive symptoms (psychosocial functioning and lifestyle), and Balance Error Scoring System (BESS) test, assessing postural stability. Additionally, participants underwent 3-T MRI at each encounter, including a high-resolution isotropic 3D T2-weighted FLAIR sequence. Two neuroradiologists independently reviewed FLAIR sequences from baseline encounters for presence of at least one WMH and of abnormal WMHs (defined as ≥ 5 punctate foci, at least one focus measuring >3 mm, or at least one focus in an atypical location); discrepancies were resolved by a consensus process involving possible review by a group of four neuroradiologists.
Ultimately, in Shetty and colleagues’ prospective multicenter study, participants with acute mTBI and matched control participants showed no significant difference in the frequency of at least one WMH (35% vs. 35%) or of abnormal WMHs (40% vs. 35%). In the mTBI group, WMHs were not associated with clinical markers of head injury.