Urinary bladder paraganglioma
Images



CASE SUMMARY
A 22-year-old pregnant female with gestational age of 12 weeks presented with a history of headache, sweating, hypertension, palpitations, lower abdominal pain, and post-micturition syncope. Routine laboratory investigations like complete blood picture, complete urine examination, liver function test, renal function test, thyroid profile and electrolytes were found to be normal with slightly elevated random blood sugar (205 mg/dl) and blood pressure (170/110 mmHg). The patient’s 24-hour urine catecholamine value of noradrenaline (NE) was 646.5 microgram/day, 7 times higher than normal, while adrenaline (E) was 12.99 microgram/day, and metanephrines were 72.21 microgram/day, all within normal range. Cystoscopy findings included slightly congested mucosa with normal left lateral wall and mucosal bulge of size 5 × 5 cm noted in the right posterolateral wall.
IMAGING FINDINGS
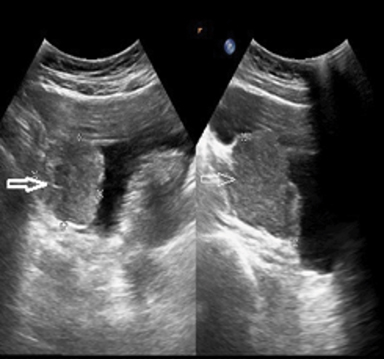
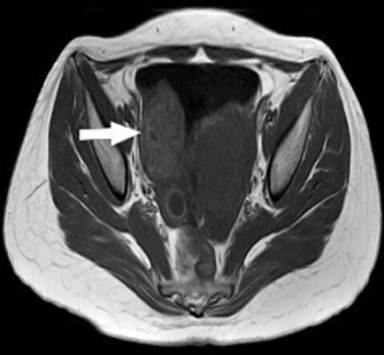
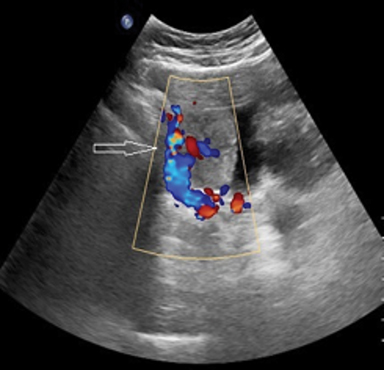
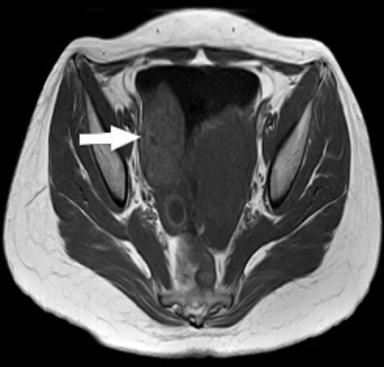
USG findings included a well-defined heterogeneously echogenic lesion of size 4 × 4 × 5 cm noted in the right posterolateral aspect of the urinary bladder with significant internal vascularity (Figure 1). Noncontrast MRI performed on Philips Achieva 1.5 Tesla scanner revealed a well-defined, multilobulated lesion of 40 × 43 × 60 mm arising from the right posterolateral aspect of the urinary bladder, which was heterogeneously hyperintense to muscle on T1 with few hyperintense foci and hypointense foci (flow voids) representing classical salt and pepper appearance suggestive of paraganglioma. These lesions appeared heterogeneously hyperintense on T2 SPAIR imaging (Figure 2). A contrast-enhanced study was not performed in light of the patient’s early gravid status.
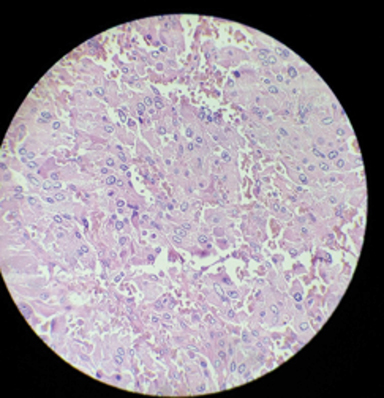
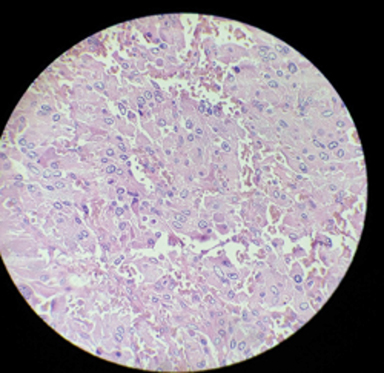
The tumor was locally resected and a sample was sent for histopathology (Figures 3, 4). On histopathology, the tumor cells were arranged in nests and a trabecular (Zellballen) pattern within a prominent vascular network. Individual cells were round to oval with abundant granular eosinophilic cytoplasm with vesicular nuclei exhibiting pleomorphism and hyperchromasia (salt and pepper nuclei). Occasional mitotic figures were noted, along with hyalinised and congested blood vessels, and adjacent fibrocollagenous tissue.
DIAGNOSIS
s/o urinary bladder paraganglioma
DISCUSSION
Paragangliomas of the urinary bladder are very rare tumors that originate from chromaffin tissue of the sympathetic nervous system associated with the urinary bladder. These tumors may be functional or nonfunctional. The functional paragangliomas present with symptoms of catecholamine excess, which include hypertension, palpitations, diaphoresis, headache, and post-micturition syncope.3 The earliest case of paraganglioma of the urinary bladder was reported by Zimmerman et al in 1953.4
Urinary bladder paragangliomas account for fewer than 0.05% of all tumors and fewer than 1% of all pheochromocytomas; those associated with pregnancy are extremely rare. The urinary bladder is the most common site for paragangliomas (79.2%) in the genitourinary tract, followed by the urethra (12.7%), pelvis (4.9%) and ureter (3.2%).5,6 They are more common in females than males (3:1) and occur primarily between 30 and 50 years of age.7 The majority of extra-adrenal tumors occur intra-abdominally; 85% occur below the diaphragm along the sympathetic chain at the bifurcation of the aorta or at the origin of the inferior mesenteric artery; ie, from the organ of Zuckerkandl. The least common location of appearance is in the urinary bladder.8
Paragangliomas associated with pregnancy may present with a spectrum of clinical manifestations, such as pre-eclampsia, episodic hypertension, palpitations, sweating, pallor, orthostatic hypotension and glycosuria. Among all the causes of hypertension, the paraganglioma and pheochromocytoma are the rarest causes, accounting for 0.1-1%.The prevalence of paraganglioma and pheochromocytoma during pregnancy is 5 per million.8
The diagnosis of the paragangliomas during pregnancy is often missed, as the clinical picture mimics pre-eclampsia, leading to lethal complications.9 Malignant paragangliomasof the bladder constitutes 10-15% of these tumors.10 Malignant pheochromocytomas cannot be differentiated from benign lesions based on the gross anatomy or histology. The malignant nature of the paraganglioma is determined based on its deep invasion, lymph-node involvement, and metastasis to local or distant organs.11
Grossly, bladder paragangliomas can be found anywhere on the bladder wall as well-circumscribed nodules or nodular aggregates. On microscopy, paraganglioma cells are arranged in a Zellballen pattern11 and surrounded by a fibrous network that is rich in blood vessels. On immunohistochemical analysis, the chief cells will be positive for neuroendocrine markers like chromogranin and synaptophysin and the sustentacular cells will be positive for S-100 protein but negative for cytokeratin, which is an epithelial marker. This feature differentiates paraganglioma from urothelial cancers and carcinoid tumors, which are positive for cytokeratin.12
Paragangliomas have nearly identical imaging features, including a homogeneous or heterogeneous hyperenhancing soft tissue mass on CT. On MRI, multiple areas of signal voids interspersed with hyperintense foci with a characteristic salt-and-pepper appearance are noted. On angiography, an intense tumor blush with enlarged feeding arteries is seen.
The treatment of choice is surgical resection with appropriate preoperative and intraoperative management to prevent hypertensive crisis. In both pregnant and nonpregnant individuals with functional paragangliomas, phenoxybenzamine is the alpha blocker of choice.13 The reported options of surgical treatment for localized or advanced disease of the urinary bladder include radical cystectomy, partial cystectomy, and transurethral resection.14
CONCLUSION
Paragangliomas are rare neuroendocrine tumors that arise from the neural crest cells. They are extra- adrenal pheochromocytomas. The most common location of paragangliomas is the retroperitoneal space and its location is rare in the pelvis. This case is reported because of its rarity.
REFERENCES
- McNichol AM. Update on tuors of the adrenal cortex, phaeochromocytoma and extra adrenal paraganglioma. Histopathology. 2011;58(2):155-168.
- Kajeyogesh D, Tanwar H, Vedpalsingh S, et al. Paraganglioma of urinary bladder presenting as an early preeclampsia with successful perinatal outcome after surgery. J Clin Diagn Res. 2015;9(9): PD01-PD02.
- Sheps SG, JiangNS, Klee GG. Recent developments in the diagnosis and treatment of pheochromocytoma. Mayo Clinicproc. 1990; 65:88-95.10.1016/S0025-6196(12)62113-2.
- Zimmerman IJ, Biron RE, Macmahon HE.Pheochromocytoma of the urinary bladder. NEJM. 1953; 249:25-26.10.1056/NEJM195307022490106.
- Hanji AM,RohanVS, Patel JJ,Tankshali RA.Pheochromocytoma of the urinary bladder: A rare cause of severe hypertention. Saudi J Kidney Dis Transpl. 2012; 23(4):813-816.
- Dahm P, Gschwend JE. Malignant non-urothelial neoplasm of the urinary bladder:areview. European urology. 2003; 44:672-681.10.1016/S0302-2838(03)00416-0.
- Yadav R, Das AK, Kumar R. Malignant non-functional paraganglioma of the bladder presenting with azotemia. Int Urol Nephrol. 2007; 39:449-451.
- Kalra JK, JainV, Bagga R, et al. Pheochromocytoma associated with pregnancy. J Obstet Gynaecol Res. 2003;29(5):305-308.
- Pearson GAH, Eckford SD, Levy A. A reason to panic in pregnancy. Lancet. 2009;374 (9691):756.
- Ahmet MH, Cengiz M,Veli U,Abdullah M. Malignant paraganglioma of the urinary bladder. Eur J Radial Extra. 2006; 58:53-58.
- Kairi-vassilatou E, Argeitis J, Nika H, et al.Malignant paraganglioma of the urinary bladder in a 44-year-old female: Clinicopathological and immunohistochemical study of a rare entity and literature review. Eur J Gynaecol Oncol. 2007;28;149-151.
- Jiang Z. Bladder paraganglioma pathology. http://emedicine.medscape.com/article/1627819-overview#aw2aab6b5. Updated July 14, 2011. Accessed October 24, 2012.
- Wald O, Shapira OM, Murar A, Izhar U. Paraganglioma of the mediastinum: Challenges in diagnosis and surgical management. J Cardiothorac Surg. 2010; 5:19.
- Kempasiddaiah GM,Thimmaiah R, Desai MG. A rare case of early pregnancy with paraganglioma of urinary bladder. IJCRR. 2014; 6(4):15-20.
Citation
G D, C V, T R.Urinary bladder paraganglioma. Appl Radiol. 2019; (3):48A-48C.
June 6, 2019