Urethral Diverticulum Containing Calculi
Images

CASE SUMMARY
A 45-year-old female with a history of total hysterectomy secondary to cervical cancer presented with complaints of dyspareunia and a 4-year history of pelvic pain when sitting and voiding, a sense of a bulge in her vagina, feeling of incomplete and difficult voiding, and nocturia. Recent progression of these symptoms prompted her to seek medical care.
On physical exam, a painful marble-sized nodule was palpated immediately adjacent to the urethra. This prompted an ultrasound scan and cystoscopy. The cystoscopy ruled out urethral cyst but questioned a urethral diverticulum. Ultrasound revealed and cystic structure of unknown etiology. Subsequent pelvic MRI revealed calculi within a urethral diverticulum. Surgical excision and extraction of the periurethral stones resulted in alleviation of the patient’s symptoms.
IMAGING FINDINGS
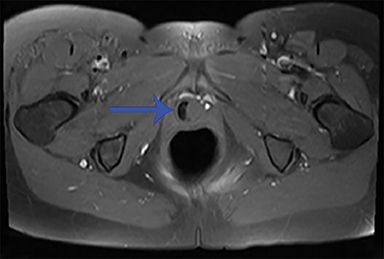
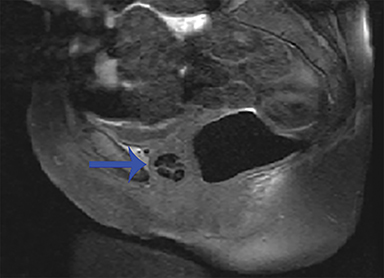
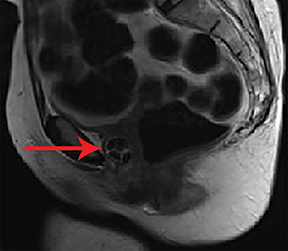
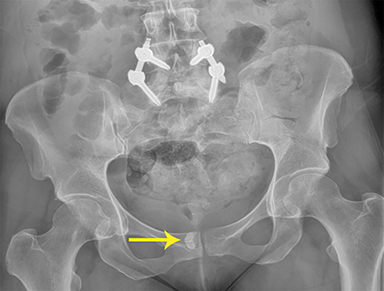
Unenhanced axial, sagittal, and coronal fat-suppressed T1, and fat-suppressed T2 MRI of the pelvis was performed to verify the presumed diagnosis. A crescentic, cystic lesion posterolateral to the urethra, with hypointensity on T1 (Figure 1) and hyperintensity on T2 (Figure 2), representing a urethral diverticulum, was observed. Both T1 and T2 imaging revealed irregular filling defects within the lumen, corresponding to calculi. This correlated with irregular calcifications seen in the lower pelvis on X-ray performed 10 months’ prior (Figure 3).
DIAGNOSIS
Urethral diverticulum containing calculi.
DISCUSSION
Urethral diverticula can present a diagnostic dilemma for many clinicians and patients. The mean interval from the onset of symptoms to diagnosis is 2-5 years, due to a variety of factors.1,2
First, the classic, “3D symptoms” (dysuria, dribbling, and dyspareunia), are present in only 20-30% of patients.1,3 Additional symptoms are varied and nonspecific, including: recurrent urinary tract infections, urinary incontinence, frequency, urgency, and hematuria. Urethral diverticulum is also a rare entity with a prevalence of 1-6%.1 As a result, the index of suspicion must be high. Our patient exemplifies the unfortunate norm for this condition: patients often live with symptoms for years before receiving a diagnosis and undergoing treatment.
Successfully diagnosing a urethral diverticulum is not only important to relieving patient symptoms, but also to avoid complications. These may include recurrent urinary tract infections, metaplasia, and malignancy. Metaplasia results from chronic inflammation. Malignancy, a rare complication, occurs in 3-9% of patients, with 100 cases reported over 60 years, but it carries a poor prognosis, with death occurring in 40% of cases.3 The types of cancers seen include adenocarcinoma, transitional cell carcinoma, squamous cell carcinoma, and clear cell carcinoma. These complications are exacerbated by the presence of stones within the diverticulum, which occurs in 10% of cases, owing to urinary stasis.
The pathogenesis of urethral diverticula is unknown. The leading theory is that chronically infected periurethral ducts become obstructed, leading to diverticulum formation.2,3 This is based on the most common location of urethral diverticula (dorsal and in the distal 2/3), which corresponds to the position of the periurethral ducts. Additionally, there are associations that would aid in obstructing periurethral glands: trauma (including difficult and prolonged vaginal deliveries), and repeated infections.
MRI is the gold standard for diagnosing urethral diverticula.3, 4, 5 The most essential components for imaging the urethra are a small field of view, high resolution, and T2 images in the axial, coronal, and sagittal planes.1 The histological layers of the normal urethra give its classic target-like appearance on T2 images: the outermost, collagen-rich muscle fibers are hypointense, the middle, elastin-rich submucosa is relatively hyperintense, and the innermost mucosa is again hypointense. The urethral diverticulum will appear as a hyperintense (urine signal) cystic lesion adjacent to or surrounding the urethra on T2 imaging.1, 5 Orthogonal planes aid in finding the neck, which makes the diagnosis definitive. Complications of urethral diverticulum may also be evident on MRI. If the diverticulum demonstrates irregular margins, wall thickening, or other features suspicious for malignancy, the clinician should obtain pre- and postcontrast, fat-saturated T1- sequences.1
Definitive treatment consists of surgical excision, the most effective method of which is via a transvaginal approach with three-layer closure; the procedure successfully eliminates symptoms in 83-97% of cases.3 Less-invasive techniques, such as fulguration, endoscopic deroofing, and marsupialization, are reserved for high-risk patients, including those who are pregnant or do not desire surgery.3
CONCLUSION
Although rare, urethral diverticulum should be kept in mind in the setting of nonspecific lower urinary tract symptoms unresponsive to conservative treatment and traditional work up. Complications are serious, and symptoms lead to significant decrease in quality of life for many patients. Surgical treatment is definitive, resulting in a very low recurrence rate. The presence of recurrent urinary tract infections without other cause, especially in the setting of palpable perivaginal mass on pelvic exam, should significantly raise the clinician’s suspicion for this condition and prompt a pelvic MRI.
REFERENCES
- Itani M, Kielar A, Menias CO, Dighe MK, Surabhi V, Prasad SR, O’Malley R, Gangadhar K, Lalwani N. MRI of female urethra and periurethral pathologies. Int Urogynecol J. 2016; 27: 195-204.
- Crescenze IM, Goldman HB. Female urethral diverticulum: current diagnosis and management. Curr Urol Rep. 2015; 16: 71.
- Greenwell TJ, Spilotros M. Urethral diverticula in women. Nature Reviews Urology. 2015; 12: 671-80.
- Surabhi VR, Menias CO, George V, Siegel CL, Prasad SR. Magnetic resonance imaging of female urethral and periurethral disorders. Radiol Clin N Am. 2013; 51: 941-53.
- Singla P. Long SS, Long CM, Genadry RR, Macura KJ. Imaging of the female urethral diverticulum. Clinical Radiology. 2013; 68: e418-e425.
Citation
A S, J G, R S, M P, Y S, T T.Urethral Diverticulum Containing Calculi. Appl Radiol. 2020; (4):46-47.
July 1, 2020