The rain artifact: A newly described artifact encountered in the critical care setting
Images


CASE SUMMARY
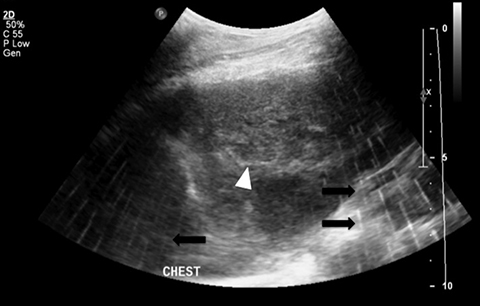
A 15-year-old female with no significant past medical history was transferred to the pediatric service with chest pain and cough. With persistent symptoms after conservative management, subsequent work-up, including an echocardiogram, demonstrated a mediastinal mass with compression of the right ventricle. Findings were subsequently confirmed with CT (Figure 1). A biopsy of the mass was requested to confirm the diagnosis. Given her known right heart compression by the mass, it was decided that the biopsy should be per formed in the operating room with general anesthesia and cardiac monitoring via transesophageal echocardiogram (TEE). In the operating room, a transesophageal echocardiogram probe was positioned for cardiac monitoring during the procedure. A C5-1 curvilinear array ultrasound probe (Phillips, Netherlands) was used for the transcutaneous biopsy with a parasternal approach. Initial images were compromised by a discontinuous linear artifact that mimics the appearance of rain (Figure 2).
IMAGING FINDINGS
Initial axial CT of the chest demonstrated a mediastinal mass. Sagittal reconstructions of the abdomen and pelvis did not demonstrate any overt metastases. MRI assessment of the lumbar spine (STIR sequence) demonstrated T2-hyperintense metastases. Post-therapy axial CT images demonstrated resolution of the thoracic mass lesions. Post-therapy CT images of the lumbar spine demonstrate osseous sclerotic response with several new sclerotic lesions. These lesions were not FDG-avid.
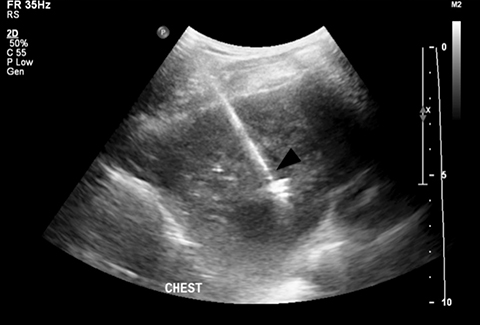
The rain artifact appears as a linear hyperechoic artifact covering the field of view. The artifact was intensified in color Doppler mode (Figure 3). The artifact persisted in various planes and with an alternative probe. It was suspected that the TEE probe was causing interference. When the TEE probe was turned off, the artifact resolved and biopsy was then performed (Figure 4).
DIAGNOSIS
We present an ultrasound artifact that we call the rain artifact that has not been previously described in the literature.
DISCUSSION
As intraoperative and procedural ultrasound use increases, it becomes vital that operators have an understanding of unique artifacts they may encounter.1,2,3 There are many common artifacts that an ultrasound operator may encounter every day, which have been well described in the literature.4,5,6
Ultrasound images are generated by emission of high frequency sound waves from piezoelectric crystals within the ultrasound probe. As the probe emits and receives sound waves, an image is generated by interpretation of the time delay and attenuation of the original sound wave.6
CONCLUSION
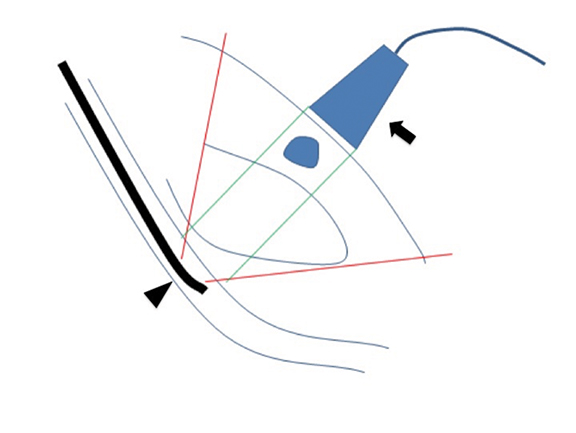
The ultrasound rain artifact is produced when multiple discontinuous linear artifacts as a result of interference from a TEE probe, causing misregistration (Figure 5). When performing ultrasound-guided procedures, the operator may encounter interference from internally generated sound waves if a TEE probe is in use. In such cases, it is important to recognize the source of the artifact, and to temporarily stop using the TEE probe for critical portions of the procedure.
REFERENCES
- Moore C, Copel J. Point-of-care ultrasonography. N Engl J Med. 2011;364(8):749-757.
- Kendall J, Hoffenberg S, Smith R. History of emergency and critical care ultrasound: The evolution of a new imaging paradigm. Critical Care Medicine. 2007;5:126-130.
- Perera P, Lobo V, Williams S, Gharahbaghian L. Cardiac echocardiography. Crit Care Clin. 2014;30(1):47-92.
- Kremkau F, Taylor K. Artifacts in ultrasound imaging. Journal of Ultrasound in Medicine. 1986;5(4):227-237.
- Scanlan K. Sonographic artifacts and their origins. AJR. 1991;156:1267-1272.
- Feldman M, Katyal S, Blackwood M. US artifacts. Radiographics. 2009;29(4):1179-1189.
Citation
T H, M H.The rain artifact: A newly described artifact encountered in the critical care setting. Appl Radiol. 2016; (7):30-31.
July 2, 2016