The Modified Barium Swallow Study: When, How, and Why?
Images
CE credit is available for this article at appliedradiology.org/aici.
Dysphagia, or difficulty swallowing, can be caused by a number of conditions, including stroke, oropharyngeal and esophageal cancers and cancer treatments, a number of neurologic diseases, and gastroesophageal reflux disease.1 Procedures that result in long-term and/or complicated intubation can also result in dysphagia, with two-thirds of patients intubated for more than 48 hours following intubation or surgery demonstrating signs and/or symptoms of dysphagia.2,3 As a result of a number of related, potentially serious clinical complications, including starvation, dehydration, airway obstruction, and aspiration, patients with dysphagia experience greater risk of pneumonia, reintubation, and death.4-6 Although effective management of swallowing disorders has been shown to improve quality of life (QOL), dysphagia has a significant negative impact on both patients and caregivers.7,8
An estimated 8% of the world’s population, or almost 600 million people, are affected by dysphagia.9 Due to the presence of comorbidities, the elderly have additional risk,10 with a reported prevalence of dysphagia of 17%,11 and dysphagia associated with feeding difficulties reported in up to 60% of nursing home residents.11 With the aging of the population, as well as the increasing prevalence of obesity and gastroesophageal reflux disease,10 the number of individuals suffering with dysphagia is expected to rise. Attempts to identify the cause of dysphagia, and the proposal and implementation of effective strategies to minimize the effects of dysphagia, represent important clinical objectives.
The modified barium swallow study (MBSS), a real-time fluoroscopic motion study, is the reference standard to assess swallowing physiology involving the oropharynx and esophagus. Here, we discuss technical considerations for the MBSS as it is performed in adults at The Johns Hopkins Hospital, with a focus on the importance of standardization of contrast, and collaboration between radiologists and speech-language pathologists (SLPs).
Background
The MBSS, also known as a video fluoroscopic swallow study (VFSS), is optimally performed by an SLP together with a radiologist, assisted by a radiologic technologist, to evaluate anatomy and swallowing physiology simultaneously in real time. The goals of the MBSS are to assess both swallowing function and safety (eg, aspiration, choking). In addition to identifying the presence of disordered swallowing physiology, a critical portion of the exam is an evaluation of compensatory strategies the patient may be able to use to enhance swallowing efficiency and/or reduce risk. The report generated from combining outcomes from the patient’s swallowing — with and without compensations — will result in recommendations for the least restrictive but safe dietary consistencies that will keep the patient adequately hydrated and nourished.12 Depending on the cause of the dysphagia, the patient’s care team may include a number of additional clinicians, including those in gastroenterology, thoracic surgery, neurology, otolaryngology-head and neck surgery, and physical medicine. Collaboration as a multidisciplinary team is essential in the clinical role of the MBSS.
The MBSS was first introduced to SLPs in the 1980s by Jerilyn Ann Logemann, PhD, an SLP at Northwestern University.13 Dr. Logemann was one of the original founding members of the Dysphagia Research Society and associate editor of the journal Dysphagia since its inception in 1985. Several radiologists, including Martin Donner, MD, Bronwyn Jones, MD, and Bob Gayler, MD, have also been influential in the study of dysphagia, contributing to the literature, editing journals, and fostering the growth of medical societies, including the Dysphagia Research Society, which seek to better understand and manage dysphagia.13,14 The work of these individuals was done at The Johns Hopkins Hospital, where they worked for decades to develop and refine the MBSS from both the radiologist’s and SLP’s perspectives.
The Johns Hopkins MBSS protocol: Technical and patient considerations
Patients with suspected dysphagia are first clinically evaluated — for inpatients, at the bedside by an SLP, or for outpatients, by an SLP or other specialty clinician in an outpatient setting. If appropriate after the clinical evaluation, the patient is referred for an MBSS. Exceptions where the patients are automatically sent for an MBSS include new tracheostomy placements and those for whom it is necessary to rule out an esophageal leak. The MBSS is not appropriate in cases when the patient is unable to be cooperative, or if they have an allergy to one or more of the additives in barium sulfate contrast agents (very rare).1
At the start of the MBSS, the patient is typically standing or seated in a special chair, and placed in the space between the fluoroscopic table and the image intensifier. Variations in X-ray equipment (eg, C-arm vs standard fluoroscopic unit) or limitations in the patient’s mobility (eg, ability to sit or stand) can necessitate modifications in patient positioning. In terms of temporal resolution, 30 frames per second, which is the standard continuous fluoroscopic image rate, is required during the swallow study to allow for the freeze-frame and slow-motion video viewing essential to understanding swallowing physiology.15 The standard lateral view is from lips to cervical spine and from the nasopharynx to the upper esophageal sphincter (with care taken to minimize eye exposure).16 Use of typical lead shielding for both clinicians and patients has been shown to be adequate for protection during the MBSS.17,18
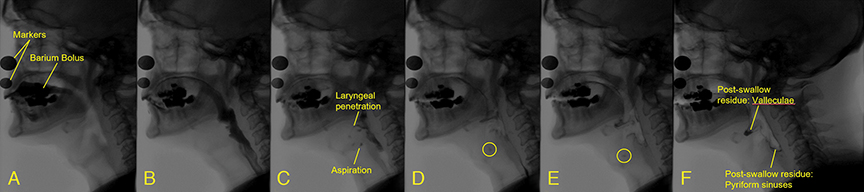
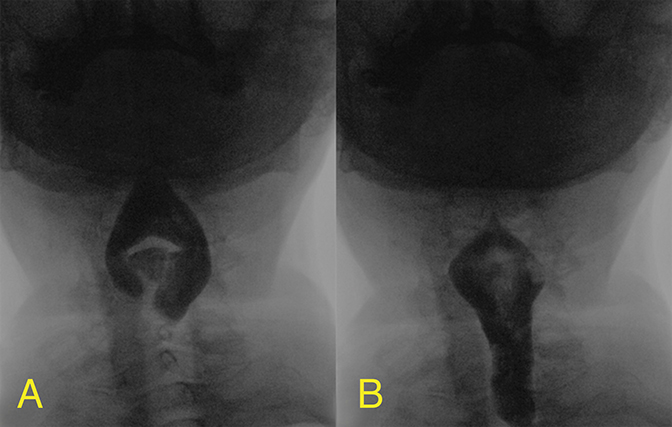
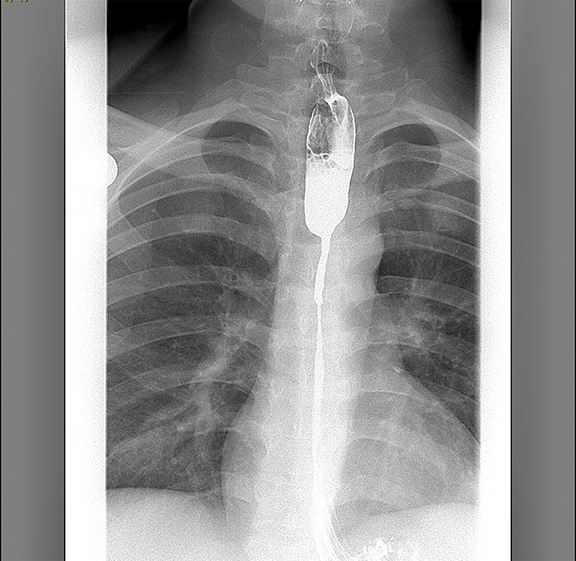
Prior to the MBSS, preliminary scout images are reviewed for any findings that potentially impact swallowing physiology (eg, swelling, arthritis, abnormal air), and a pre-examination discussion occurs between the radiologist and SLP. Then, for most patients, both lateral and anterior-posterior (AP) views will be obtained during swallowing (Figures 1-3). The SLP and the radiologist then follow the standardized protocol set forth by the Modified Barium Swallowing Impairment Profile (MBSImP).16 The MBSImP protocol necessitates the use of Varibar® barium sulfate (Bracco Diagnostics Inc., Monroe Twp., NJ),19,23 the only standardized preparation of barium sulfate specifically for use during the MBSS. To this end, patients are presented with a series of the barium-sulfate–containing products, from thin to thick in consistency, and from a lower volume to higher volume; specifically, 5 mL thin liquid, graduating to 15 mL thin liquid, then a single sip from a cup or straw, then continuous sips from a cup or straw, progressing similarly to nectar, to honey, to pudding, and finally, to a cookie dipped in pudding.12 Most often, a complete series from thin to barium-coated cookie is completed, but exceptions exist where the clinical scenario dictates omitting consistencies or changing the order in which they are given, at the discretion of the SLP and radiologist. In the lateral view, it is relatively easy to observe most of the components of swallowing, with the exceptions of pharyngeal contraction, lateralization of residue, and the esophagus, which are better evaluated in the AP view. Therefore, toward the end of exam, the patient is turned to the AP view to assess these components. The appearance of glottic closure and opening (ie, adduction and abduction of the arytenoid cartilages) is also assessed by eliciting phonation in the AP view. It should be noted that a full evaluation of the esophagus cannot be done following a full pharynx exam, since the various consistencies of barium sulfate will interfere with esophagus mucosal assessment. In addition, a proper esophageal evaluation includes the horizontal orientation for evaluation of peristalsis and gastroesophageal reflux.
During the examination, the radiologist and SLP are viewing the same images to evaluate swallowing physiology. As both radiologist and SLP have a unique expertise and perspective, having both present and interacting to interpret the fluoroscopy images contributes to the quality of the exam and improves patient outcomes.24 In addition, as the exam is performed in real time, there are clear advantages to having two individuals observing and/or reviewing the swallow study. Both the continuous dialogue and the collaboration between the two specialists and the patient are considered necessary for a most effective and successful MBSS.
Once disordered swallowing physiology is identified, the SLP can implement a compensatory posture (eg, tucking the chin down, turning or tilting the patient’s head to the right or left) or maneuver (eg, supraglottic swallow, Mendelsohn maneuver) to attempt to change the swallowing dynamics on the next swallow of the same volume/consistency, improving function and/or safety.25
After the exam, the SLP uses slow motion and frame-by-frame analysis to carefully review the MBSS images and recommend a therapeutic regimen, often in consultation with the radiologist. The regimen is individually tailored to the patient’s specific swallowing physiology to improve his or her ability to obtain adequate and safe nutrition, and may be composed of any combination of postures, exercises, and/or diet consistency changes.
The MBSS is a diagnostic study; it is not a screening that provides a binary “pass” or “fail” result, nor is it a test to determine the presence of aspiration. The MBSS provides a real-time assessment of swallowing physiology and functional outcome, a necessary step toward safe swallowing and rehabilitation.
Importance of standardization
The MBSS is, to some extent, a subjective test; therefore, standardizing the exam has the potential to increase its robustness and decrease the variability of its results. Beneficial effects of standardization also include increased inter-rater reliability, enhanced communication between the radiologist and SLP, and increased capability of clinicians to determine which strategies potentially improve swallowing function and/or safety. In addition, such standardization facilitates intrapatient, interpatient, and cross-population comparisons, while contributing to the clinical training of both radiologists and SLPs who execute and are interested in MBSSs.
There are two main aspects of the MBSS that have been successfully standardized: (1) the barium products of various consistencies used during the exam, and (2) the method of assessment and reporting of the MBSS results.
Standardized barium-sulfate-containing contrast agent consistencies
To date, the Varibar series is the only FDA-approved set of standardized barium sulfate products available in varying consistencies for evaluation of the oropharyngeal swallow and esophageal clearance.19-23 Varibar is made specifically for oropharyngeal swallow examinations and is available in 5 consistencies (ie, thin liquid, thin honey, honey, nectar, pudding), all containing the same concentration of barium sulfate (40% weight/volume).19-23,26 Use of a set of standardized barium sulfate contrast agents in place of homemade barium sulfate products reduces preparation time and wasted materials, supports high-quality imaging,27,28 and enables reproducible results.27-30 Moreover, nomenclature is standardized such that all clinicians are using the same terminology to describe the clinical findings with the different consistency products — so regardless of where the examination is performed, thin liquid, honey, etc., always means the same thing.
Standardization of scoring and reporting the MBSS with the MBSImP
The MBSImP, developed by Bonnie Martin-Harris, PhD and colleagues, is a standardized protocol to interpret and communicate swallowing impairment in a manner that is specific, consistent, accurate, and objective.16 The MBSImP scores 17 identified components of swallowing function and bolus clearance during the MBSS for each barium-sulfate–containing product.16 The MBSImP is particularly powerful because it is used in conjunction with the Varibar series such that all patients are assessed with standardized barium sulfate measurements and consistencies, ensuring that the same information (eg, definitions of mild, moderate, severe for each component for each consistency) is recorded in the patient’s record. At The Johns Hopkins Hospital, the use of the MBSImP is part of the training for all staff administering and scoring the MBSS.
Conclusions
Patients with suspected dysphagia are best evaluated by a radiologist together with an SLP, using the MBSS (ie, real-time fluoroscopy). To enhance robustness of the MBSS, both the barium sulfate contrast and the swallowing function scoring are standardized using Varibar and the MBSImP, respectively. More than just a diagnostic exam, MBSS allows for strategies to be evaluated that are likely to improve the swallowing function, safety, and QOL in dysphagia patients.
Acknowledgements: The authors thank Bronwyn Jones, MD, and Bob Gayler, MD, for expert review of this article, and Cindy Schultz, PhD, for medical writing assistance.
References
- Peterson R. Modified Barium Swallow for Evaluation of Dysphagia. Radiol Technol. 2018;89:257-275.
- Skoretz SA, Flowers HL, Martino R. The incidence of dysphagia following endotracheal intubation: a systematic review. Chest. 2010;137:665-673.
- Skoretz SA, Yau TM, Ivanov J, Granton JT, Martino R. Dysphagia and associated risk factors following extubation in cardiovascular surgical patients. Dysphagia. 2014;29:647-654.
- Palmer JB, Drennan JC, Baba M. Evaluation and treatment of swallowing impairments. Am Fam Physician. 2000;61:2453-2462.
- Popa Nita S, Murith M, Chisholm H, Engmann J. Matching the rheological properties of videofluoroscopic contrast agents and thickened liquid prescriptions. Dysphagia. 2013;28:245-252.
- Macht M, Wimbish T, Clark BJ, et al. Postextubation dysphagia is persistent and associated with poor outcomes in survivors of critical illness. Crit Care. 2011;15:R231.
- Singh S, Hamdy S. Dysphagia in stroke patients. Postgrad Med J. 2006;82:383-391.
- Namasivayam-MacDonald AM, Shune SE. The Burden of Dysphagia on Family Caregivers of the Elderly: A Systematic Review. Geriatrics (Basel). 2018;3:1-14.
- Cichero JA, Lam P, Steele CM, et al. Development of international terminology and definitions for texture-modified foods and thickened fluids used in dysphagia management: the IDDSI Framework. Dysphagia. 2017;32:293-314.
- Aslam M, Vaezi MF. Dysphagia in the elderly. Gastroenterol Hepatol (N Y). 2013;9:784-795.
- Jardine M, Miles A, Allen JE. Swallowing function in advanced age. Curr Opin Otolaryngol Head Neck Surg. 2018;26:367-374.
- Martin-Harris B, Jones B. The videofluorographic swallowing study. Phys Med Rehabil Clin N Am. 2008;19:769-785.
- Logemann JA. Manual for the videofluorographic study of swallowing. 2nd ed. ProEd; Austin: 1993.
- Jones B, Donner, MW. Normal and abnormal swallowing: Imaging in diagnosis and therapy. Springer Verlag; New York: 1991.
- Bonilha HS, Blair J, Carnes B, et al. Preliminary investigation of the effect of pulse rate on judgments of swallowing impairment and treatment recommendations. Dysphagia. 2013;28:528-538.
- Martin-Harris B, Brodsky MB, Michel Y, et al. MBS measurement tool for swallow impairment--MBSImp: establishing a standard. Dysphagia. 2008;23:392-405.
- Hayes A, Alspaugh JM, Bartelt D, et al. Radiation safety for the speech-language pathologist. Dysphagia. 2009;24:274-279.
- Bonilha HS, Huda W, Wilmskoetter J, Martin-Harris B, Tipnis SV. Radiation Risks to Adult Patients Undergoing Modified Barium Swallow Studies. Dysphagia. 2019;Mar 4.
- VARIBAR® THIN LIQUID (barium sulfate) for oral suspension full Prescribing Information. Monroe Twp., NJ: Bracco Diagnostics Inc.; April 2019.
- VARIBAR® THIN HONEY oral suspension full Prescribing Information. Monroe Twp., NJ: Bracco Diagnostics Inc.; January 2018.
- VARIBAR® HONEY (barium sulfate) oral suspension full Prescribing Information. Monroe Twp., NJ: Bracco Diagnostics Inc.; March 2018
- VARIBAR® NECTAR (barium sulfate) oral suspension full Prescribing Information. Monroe Twp., NJ: Bracco Diagnostics Inc.; February 2018
- VARIBAR® PUDDING (barium sulfate) oral paste full Prescribing Information. Monroe Twp, NJ: Bracco Diagnostics Inc.; Oct. 2016.
- Jones J. Case Study: Collaboration Comes Standard. March 2018. Available at: https://www.acr.org/-/media/ACR/Files/Case-Studies/Quality-and-Safety/CollaborationComesStandard/Imaging3_CollaborationComesStandard_March2018-(1).pdf. Accessed: June 4, 2019.
- Martin BJ, Logemann JA, Shaker R, Dodds WJ. Normal laryngeal valving patterns during three breath-hold maneuvers: a pilot investigation. Dysphagia. 1993;8:11-20.
- Steele CM, Barbon C, Namasivayam A. Best Practices in Videofluoroscopy. Dysphagia Cafe. Available at: https://dysphagiacafe.wordpress.com/2014/03/19/best-practice-in-videofluoroscopy-by-dr-catriona-steele-carly-barbon-and-ashwini-namasivayam/. Accessed May 20, 2019.
- Robbins JA, Nicosia M, Hind JA, Gill GD, Blanco R, Logemann J. Defining Physical Properties of Fluids for Dysphagia Evaluation and Treatment. Perspectives on Swallowing and Swallowing Disorders. Dysphagia. 2002;11:16-19.
- Martin-Harris B, Humphries K, Garand KL. The Modified Barium Swallow Impairment Profile (MBSImP™©) – Innovation, Dissemination and Implementation. Perspectives of the ASHA Special Interest Groups. 2017:2:129-138.
- Hind J, Divyak E, Zielinski J, et al. Comparison of standardized bariums with varying rheological parameters on swallowing kinematics in males. J Rehabil Res Dev. 2012;49:1399-1404.
- Steele CM, Molfenter SM, Péladeau-Pigeon M, Stokely S. Challenges in preparing contrast media for videofluoroscopy. Dysphagia. 2013;28:464-467.
Citation
MM F, C S, MB B.The Modified Barium Swallow Study: When, How, and Why?. Appl Radiol. 2019; (5):
September 25, 2019