The Benefits of Using Synthesized 2D (C-View™) Images in Breast Tomosynthesis Exams
Images
Breast tomosynthesis, also known as 3D mammography, has been shown to greatly reduce detection challenges associated with overlapping structures in the breast, which is the primary drawback of conventional 2D mammography. In the recent large study of tomosynthesis in breast cancer screening published in the Journal of the American Medical Association, the authors found a significant (41%) increase in the detection of invasive cancers with a simultaneous decrease in false positives.1 These results are consistent with the findings of earlier, smaller studies.2,3
These studies all reported on the performance of 3D mammography using Hologic Selenia® Dimensions® systems operating in combo mode, where both two 2D full field digital mammography (FFDM) views and two 3D views (altogether 2D-CC, 2D-MLO, 3D-CC, 3D-MLO) are acquired for each breast. The clinical advantages of combo mode are clear. However, the radiation exposure is higher, albeit within allowable limits, than for conventional 2D mammography, because both a 2D and a 3D exposure is acquired for each projection. For this reason, Hologic developed C-View™ software, which generates the 2D images directly from the 3D dataset and avoids the need for the 2D exposures altogether. The dose for the 3D plus C-View procedure is similar to that of 2D mammography.
The retrospective reader study performed by Hologic as part of their FDA submission for this new operating mode found that C-View images plus 3D was superior to 2D mammography alone.4 The performance of C-View was also studied and compared to combo mode and the authors Skaane et al found that C-View plus 3D “performed comparably” to combo mode.5
The high performance of C-View plus 3D images in breast cancer screening, along with its dose reducing capability, motivated my institution to incorporate it into our routine clinical practice. As a result, we are realizing all the benefits of tomosynthesis at doses comparable to conventional 2D mammography.
Adoption of Tomosynthesis and C-View images
Tomosynthesis was FDA approved in February 2011, and we installed our first unit at the John C Lincoln Breast Health and Research Center in April 2011. Based on patient demand, a second unit was installed in September 2011. The third unit was placed when we opened a new location in 2013. The fourth unit, along with the Affirm™ breast biopsy system, was installed in February 2014 at our main location.
Because we believed in the superior performance of tomosynthesis, but wanted to offer a lower dose option to our patients, we started using C-View software in August 2013. We elected to stop doing the traditional 2D imaging from the very beginning, so we have been doing 3D with C-View exclusively since that time.
Generating C-View images
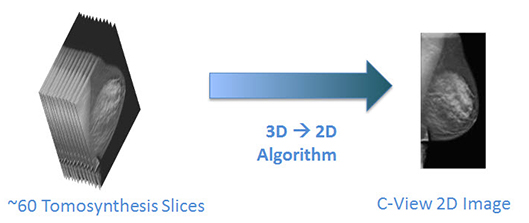
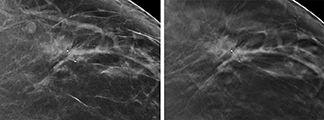
When using C-View software, the tomosynthesis acquisition and reconstruction is performed in the standard manner. This can be done in any desired projection. Following the reconstruction, an algorithm converts the 3D data into a single 2D C-View image (Figure 1). The radiologist is presented with both the C-View plus 3D images.
Use of C-View images in clinical practice
In our practice, we find that the C-View 2D image can be used in the same way as an acquired 2D image is used, as part of a 3D examination. It facilitates comparison to 2D priors, judging left/right asymmetry, and assessing the distributional aspects of calcifications. C-View images are never reviewed by themselves; they are reviewed along with the tomosynthesis images. Any potential finding in the C-View image is confirmed and evaluated in the 3D images before making a diagnosis, because the 3D images are the “fundamental” images in the study.
Performing a tomosynthesis examination without the use of either 2D or C-View images has been proposed, but we firmly believe that having a 2D image available facilitates the above-mentioned tasks that radiologists perform when reading screening examinations.
Comparison of C-View images to traditional 2D images
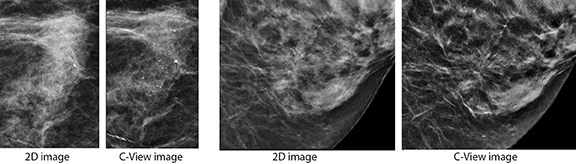
A C-View is similar to, but different from, an acquired 2D image. The parenchymal density ‘look’ differs a little from traditional 2D images. This is not unexpected, as they are different images. We are already familiar with images that have a variety of looks, and we face and deal with this issue when reviewing images from the different manufacturers of digital mammography equipment.
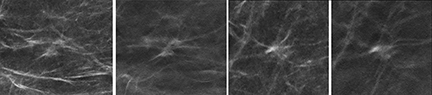
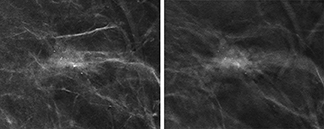
In our early evaluation of this technology, we found C-View images to be superior to traditional 2D images in some respects. The appearance of micro-calcifications is often, although not always, higher in contrast than on a 2D image. Similarly, architectural distortions and spiculations are also often more conspicuous in the C-View image than on the corresponding 2D image, as illustrated in Figure 2.
Other advantages of C-View images
In addition to clearer visibility in some cases, there is absolutely no dose associated with C-View images. This allows us to have a full two-view 2D dataset as part of a two-view 3D study without any additional dose beyond the 3D images themselves. In addition, our patients are pleased that the compression time is shorter, because the 2D exposure is eliminated.
Additionally, some advocate for just one view tomosynthesis to reduce dose; our experience reveals that two 3D views result in optimal detection potential. Some cancers, because of pattern growth, are only visible on one 3D view.
Case Examples
Distribution of calcifications using C-View.
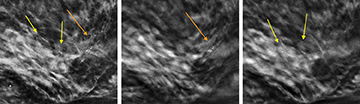
A 65-year-old patient with heterogeneously dense breasts. With C-View, we can clearly see a heterogeneous cluster of microcalcifications in the posteromedial right breast (Figure 3). On the tomosynthesis slices, not all of these calcifications are in focus at the same time, so the cluster orientation is more difficult to appreciate, though the individual calcifications are very well seen. A 3D-guided biopsy was done, showing columnar cell hyperplasia with atypia. Surgical pathology result: flat epithelial atypia and ADH.
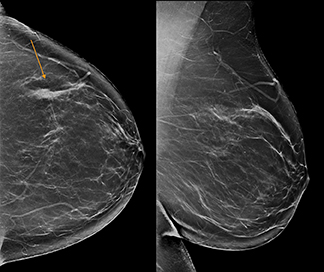
C-View appearance of architectural distortion
65-year-old female, presenting for routine screening. No prior mammograms were available. The patient has fairly fatty breasts. C-View shows a 9 mm architectural distortion, though subtle, in the right breast at 2 o’clock. The distortion is clearer on the tomosynthesis slices, and particularly better seen on the CC view (Figure 4). Though subtle, the tomosynthesis findings were felt to be definitive without need for additional mammographic views. Ultrasound showed a 9-10 mm irregular hypoechoic lesion to correlate with the screening mammogram. Ultrasound-guided biopsy showed infiltrating mammary carcinoma with extensive lobular differentiation, Nottingham score 2/3.
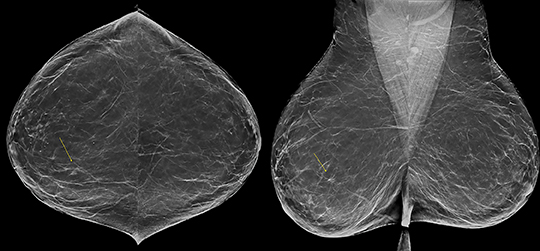
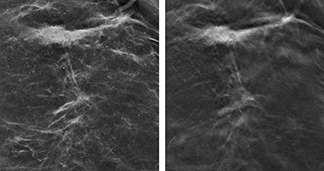
Multifocal disease
53-year-old female, presenting for routine screening. Prior mammograms were not available at the time of screening, but were obtained subsequently. The breast is minimally dense. C-View images show distortion in the left UOQ, well seen with tomosynthesis to measure about 1.2 cm (Figure 5). This larger distortion is seen on both the CC and MLO views. A smaller area of distortion was also noted on the CC view only, central to the nipple. These areas were seen on prior exams but were more prominent, and tomosynthesis clearly showed the distortion in addition to the asymmetric densities.
The patient returned for ultrasound, without need for additional mammographic imaging. Ultrasound showed a 9 mm irregular hypoechoic lesion to correlate with the more central distortion, and a 1.6 cm irregular lesion at 2 o’clock, correlating with the larger UOQ distortion. A plump axillary node was also noted, which was not seen on the mammogram due to its deep location.
Ultrasound-guided biopsies were done of all three areas: Both breast lesions were invasive lobular carcinoma, provisional Nottingham grade 1. The axillary node was positive for carcinoma, consistent with metastasis (residual nodal material was not seen on the core biopsy).
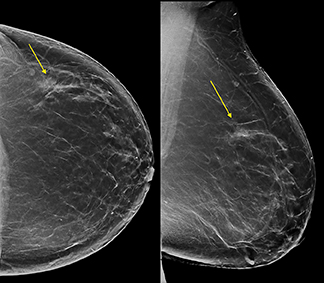
Tomosynthesis reveals architectural distortion
54-year-old female, presenting for routine screening. The breasts are mildly dense. New clustered microcalcifications were seen in the left UOQ, well seen with C-View images, and tomosynthesis shows associated architectural distortion to better advantage (Figure 6). Magnification imaging was done, but does not show the distortion as well as the tomosynthesis images. Ultrasound does show an irregular hypoechoic mass within the UOQ, correlating well. Ultrasound-guided biopsy showed DCIS, intermediate grade, predominantly cribriform and micropapillary types, with possible secondary involvement of a papillary lesion.
The distortion and irregular mass appearance on ultrasound made this lesion very suspicious for an invasive component. The surgeon was advised, and at lumpectomy, a sentinel node biopsy was done based on this suspicion. Surgical pathology did confirm invasive ductal carcinoma.
Conclusion
C-View images serve as an excellent replacement for the traditional 2D images. The “2D” image set is still essential for: side-by-side comparison, comparison to priors, and evaluation of the overall configuration of a calcification cluster. Surgeons, oncologists, and other radiologists without tomosynthesis still need to see these “2D” images as well.
C-View images excel in that architectural distortions are preserved, and therefore may be much better seen than on traditional 2D images. This is because the 3D images themselves are used to create this image, so structural information seen much better with tomosynthesis will be preserved on C-View images. Similarly, calcifications are often also of higher contrast than seen on FFDM, serving to draw your eye to the region, so we can focus on that area in our review of the tomosynthesis set. Finally, the use of C-View allows us to acquire both the CC and MLO views in 3D mode, which is important to help keep our recall rates low and to maximize cancer detection, as we often see the lesions appear better in one of the two views, more often than not the 3D CC view.
All of this is done with zero added dose over the 3D dose, giving us an exam far superior to digital mammography: We get the now well-proven benefit of 3D imaging, and the usefulness of the “2D” set, but with a radiation dose comparable to FFDM. In our 14-months of experience using C-View images, not only are we offering fully two-view 3D screening at the same dose as FFDM, but are also seeing a slight increase in cancer detection using C-View images compared to our original use of acquired 2D plus 3D imaging.
References
- Friedewald SM, Rafferty EA, Rose SL, et. al. Breast Cancer Screening Using Tomosynthesis in Combination with Digital Mammography. JAMA. 2014;311(24):2499-2507.
- Rose SL, Tidwell AL, Bujnoch LJ, et al. Implementation of breast tomosynthesis in a routine screening practice: an observational study. AJR Am J Roentgenol. 2013 Jun; 200(6):14018, 2013.
- Skaane P, Bandos AI, Gullien R, Eben EB, et al. Comparison of digital mammography alone and digital mammography plus tomosynthesis in a population-based screening program. Radiology. Apr; 267(1):47-56, 2013.
- FDA PMA Number P080003 S001. http://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfpma/pma.cfm?id=17925
- Skaane P, Bandos A, Eben E, et al. “Two-View Digital Breast Tomosynthesis Screening with Synthetically Reconstructed Projection Images: Comparison with Digital Breast Tomosynthesis with Full-Field Digital Mammographic Images” Radiology. 2014 Jun; 271(3):655-63.
Citation
The Benefits of Using Synthesized 2D (C-View™) Images in Breast Tomosynthesis Exams. Appl Radiol.
November 6, 2014