Technology and Industry: Osteoporosis update
Images
Osteoporosis poses a significant health risk in the United States, particularly among women, and the problem is expected to only intensify as the population ages, according to a recent Surgeon General's Report. 1
The scope of the problem
Within the next 25 years, roughly 20% of the U.S. population (~71 million people) will be ≥65 years. 2 Current estimates indicate that 10 million Americans have osteoporosis and 34 million are at risk of developing it. 1 By 2020, those numbers are expected to reach 14 million and 47 million, respectively. 1
Each year, 1.5 million adults suffer an osteoporotic fracture. 1 According to the National Osteoporosis Foundation, a woman's risk of hip fracture is equal to her risk of breast, uterine, and ovarian cancer combined. 3 Nearly 3 times as many women have an osteoporotic fracture as have a heart attack. 4 For the approximately 300,000 of those who suffer a hip fracture, the outcome can be devastating. 3 The 1-year mortality rate for people >50 years who experience a hip fracture is approximately 24%. 3 For many of those who do survive, however, life is never the same. At 6 months, only 15% of hip fracture patients can walk across a room unaided. 3 Another 20% who were ambulatory before the injury may require long-term care as a result, 3 and up to 80% may be unable to carry out at least 1 independent activity of daily living following a hip fracture. 4 In addition to hip factures, osteoporotic vertebral factures, of which there are approximately 750,000 per year, 4 can result in chronic pain and disability.
"We're clearly not getting to all the patients who need treatment," said John Jenkins, Director of Product Management at Hologic Inc. (Bedford, MA). "The large population of baby boomers are reaching, or have just passed, menopause. They are now in the target period for osteoporosis testing. With the number of patients who have osteoporosis now, factoring in the changing demographics through 2020, it's clear that it is a growing health concern."
The financial burden of bone disease on the healthcare system is enormous. In 2002, it was estimated that the national direct-care expenditures for osteoporotic factures was $18 billion. 3 This number can only be expected to rise. In his recent report, the Surgeon General warned, "Due primarily to the aging of the population and the previous lack of focus on bone health, the number of hip fractures in the United States could double or even triple by the year 2020." 1
Risk factors for developing osteoporosis
In addition to being female and of advanced age, risk factors for developing osteoporosis include: history of fracture after age 50, low bone mass, being thin or having a small frame, a family history of osteoporosis or fracture in a close relative, estrogen deficiency, amenorrhea, anorexia nervosa, low lifetime intake of calcium, Vitamin D deficiency, an inactive lifestyle, the presence of certain chronic medical conditions, and the use of certain medications, among others. 3
What can be done?
Creation of maximum bone mass early in life and prevention of bone loss later in life are the keys to long-term skeletal health. Approximately 98% of a woman's bone mass is formed before the age of 20; therefore, building a healthy skeletal system during childhood and adolescence is the best defense against later osteoporosis. 3 This process can be aided by a lifetime diet high in calcium and Vitamin D, performance of weight-bearing exercise, and avoidance of smoking and excessive alcohol intake. 3
One of the greatest challenges with osteoporosis is that the first recognized symptom is often a fracture. Therefore, bone mineral density (BMD) testing before a fracture occurs is extremely important for the diagnosis of osteoporosis and the prevention of fractures. The National Osteoporosis Foundation recommends that all women over the age of 65 undergo BMD testing regardless of their risk factors. 5 They also recommend testing for younger, postmenopausal women with ≥1 risk factor other than gender and age, and postmenopausal women who present with any facture. 5 For those over the age of 65, Medicare covers the cost of BMD testing every 2 years.
Many imaging centers suggest that patients undergo mammography and BMD testing during the same visit. "The women who need mammograms also need bone density studies," noted Jenkins.
Advances in osteoporosis assessment technology
A variety of technologies have been used to assess skeletal health, the most common of these is dual-energy X-ray absorptiometry (DXA), which measures the spine, hip, or total body. Recent advances in this imaging technology have made the assessment of skeletal health faster and more accurate.
The Discovery QDR Series bone densitometer (Hologic Inc., Bedford, MA) features High Definition Instant Vertebral Assessment (IVA), which takes a 10second scan of the lumbar thoracic spine to visualize vertebral deformities (Figure 1). "This helps classify additional patients as osteoporotic even with border-line results by typical BMD," said Jenkins. "With this, the physician can take rapid images and determine whether or not there is a vertebral compression fracture."
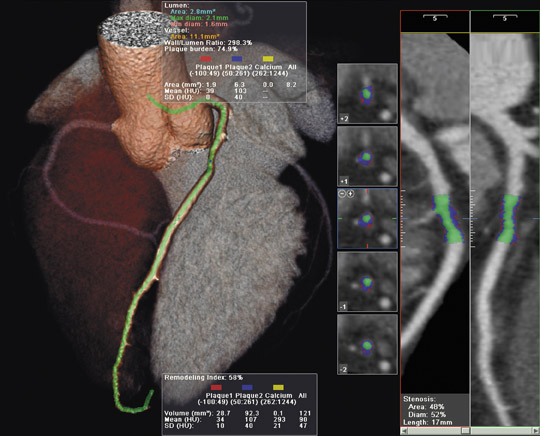
The system also features CAD fx , a computer-aided detection system. "With CAD fx , the user clicks on a vertebral body," explained Jenkins. "The software outlines the vertebral body and takes a quantitative measurement that compares the anterior height and the medial height of the vertebral body to the posterior height. This provides quantification for grading vertebral deformities." Discovery also features Hip Structure Analysis (HSA) software designed by The Johns Hopkins University Applied Physics Laboratory (Baltimore, MD) to examine the structural geometry of the hip with 2-dimensional densitometry images. This software was developed to assess the structural integrity of the bone, not just bone mineral density.
Hologic recently received U.S. Food and Drug Administration clearance for use of the Discovery images as "a measure of the possibility of coronary heart disease, stroke, and other forms of cardiovascular disease" through the assessment of aortic calcifications on the densitometry images (Figure 2). With this, physicians can use the information already contained within the scan to assess the patient's risk of a cardiovascular event, since aortic calcification is a strong predictor of cardiovascular disease. 6
Conclusion
"All of these advances are ways to make the DXA basic bone density system a more useful tool in looking at overall patient health," explained Jenkins. "You start out with a basic bone density value, which is a good assessment of fracture risk. When you add vertebral imaging, it becomes a better assessment of fracture risk. Then, since hips are essentially a mechanical device that hold the body up, with bone geometry, the clinician is better able to predict potential bone failure. With the ability to assess cardiovascular risk, there is yet another layer of value."
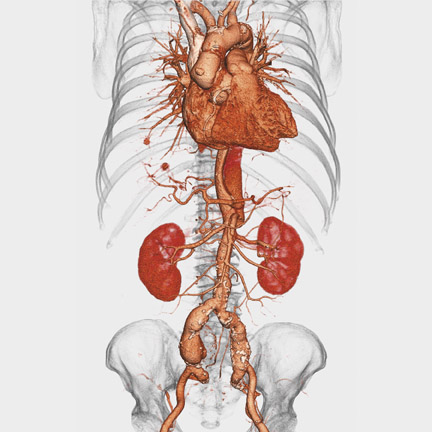
Looking to the future, Jenkins predicts that the next advance in DXA technology will be 3-dimensional reconstruction of the hip with bone densitometry images, similar to computed tomography reconstructions. "By taking a limited data set and reconstructing a 3D image of the hip," he concluded, "we hope to take very accurate geometric measurements of the hip and to better assess its strength."
Citation
Technology and Industry: Osteoporosis update. Appl Radiol.
September 12, 2007