Striking a balance in PET imaging transforms patient care
Images
Supplement to Applied Radiology December 2012, sponsored by Philips
Dr. Osman is the Program Director of the Division of Nuclear Medicine, Department of Radiology, Saint Louis University Hospital, St. Louis, MO.
One of the most significant transformations in patient care can be achieved simply by striking a balance across the continuum of care. This is especially true when managing oncology patients from diagnosis to staging to monitoring disease, where managing tradeoffs is critical to delivering the best treatment.
As the second most common cause of death in the United States, preceded only by cardiovascular disease (CVD), cancer accounts for nearly 1 of every 4 deaths.1 In 2012, an estimated half-million Americans, or >1,500 people a day, were expected to die of cancer.1
The use of integrated positron emission tomography and computed tomography (PET/CT) imaging with18F fluorodeoxyglucose (FDG) is a widely established imaging technique with major indications in oncology for staging, re-staging, and monitoring response to therapy.2 In fact, at leading nuclear medicine institutions, such as Saint Louis University School of Medicine, St. Louis, MO, 90% of PET studies are conducted on patients with cancer, while the other 10% is divided among neurological and cardiac PET-imaging studies. The majority of PET studies involve lymphoma and cancers of the lung, head and neck, colon, esophageal, melanoma, and breast.
One of the challenges with PET/CT imaging is respiratory motion, which can have a major degrading impact on PET-based tumor quantification and delineation,3-7 and inhibits the ability to define accurate target volumes in radiation oncology. This is particularly true for small lesions found in borders between organs, such as the lung and liver.
In lesion detection, the challenge is the difference in the resolution. In the PET world, the accuracy of a lesion 1 cm or less in size used to be suboptimal. It was even more complicated if the same small-size lesion was in a patient with a high body-mass index (BMI). In obese patients, scatter and attenuation artifacts led to more challenges in identifying and characterizing small lesions.
Additionally, with organized industry efforts, such as ALARA (as low as reasonably achievable) and the Image Gently® Campaign, to lower the levels of radiation dose patients are exposed to during medical imaging exams, radiologists and nuclear medicine physicians have been challenged to find strategies to manage dose without degrading image quality.
The main problem we have had in PET imaging is how to balance scanner throughput without compromising image quality and without having to resort to higher radiotracer dose. Up until now, balancing image quality, dose and scan time has been the tradeoff.
The Ingenuity TF PET/CT advantage
The need for more accurate tumor quantification and delineation has led to the development of technology that enables high-quality PET/CT images to be acquired at low dose levels.
Philips Ingenuity TF PET/CT addresses the challenges of localization, specificity and low dose in oncology and neurological imaging exams, and overcomes obstacles for conducting cardiac perfusion and diagnostic CT studies. The system is equipped with Astonish TF with 4-dimensional (4D) time-of-flight (TOF) capabilities for high-speed and full-fidelity PET imaging. With 495 picoseconds (ps) timing resolution on the system, Astonish TF provides the fastest timing resolution currently available, helping to lead to enhanced localization of events.
Astonish TF provides TOF technology designed to enhance image quality by reducing noise and providing high sensitivity. The high-quality images help to improve lesion detection and localization to increase diagnostic confidence and preserve healthy tissue during treatment. This latest generation in TOF technology leads to enhanced contrast by up to 30% compared to non-TOF images.
The 4D component of TOF is designed to provide additional image quality and standard uptake value (SUV) quantitation improvements to account for patient movement during respiratory-gated studies. In fact, Astonish TF shows up to 50% improved contrast resolution, while maintaining quantitative accuracy with up to 4 times the reconstruction speed of previous-generation systems.
Low dose techniques for quality imaging
To address the need to manage CT dose without sacrificing image quality, the system comes available with iDose4, a CT iterative reconstruction technique.
As an iterative reconstruction technique, iDose4 gives the user control of the dial, enabling clinicians to personalize image quality based on the patients’ needs at low dose. iDose4 is designed to improve spatial resolution at low dose, reduce noise with a natural appearance, provide robust artifact prevention, and improve image quality*. In fact, iDose4 improves spatial resolution by up to 57% on the Ingenuity CT platform.
List mode capabilities
Another important feature of Astonish TF for improving lesion detection is list mode reconstruction capabilities. This technology records each event and timing sequentially to enhance image resolution and improve accuracy. By leveraging list-mode reconstruction, Astonish TF can provide higher accuracy in SUV values without compromising performance.
List mode reconstruction enables us to acquire all the information with a single event at a time and to process this data in a short amount of time. It produces a more uniform picture and better tradeoff. What’s unique about the Astonish TF is what’s described as full fidelity, and it is the only TOF that offers a highly accurate way to reconstruct images in a very fast mode.
Clinical applications
Improving lesion detection
The clinical advantage of TOF technology for PET is that it produces sharper images that are better for lesion detection and localization. This increases diagnostic confidence for the physician and contributes to preserving healthy tissue during radiation therapy treatments.
Another advantage of the TOF is the ability to see smaller and smaller lesions that , until recently, were unable to be detected and/or characterized.
In a recent study,7 TOF PET yielded a significant improvement in lesion detection in oncologic studies over all contrasts and BMIs, and this improvement was greater for lower lesion contrasts. The study evaluated 100 patients with various body types and found that TOF PET scans improved the signal-to-noise ratio for both liver and lung images and resulted in improvement in lesion detection.
Fast image acquisition in TOF PET is enabling doctors to acquire head-to-toe whole-body images acquisitions in a reasonable amount of time without compromising the throughput of the scanner. We are able to see smaller lesions, get better image quality, and image head-to-toe in a reasonable amount of time.
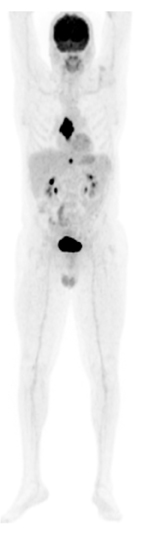
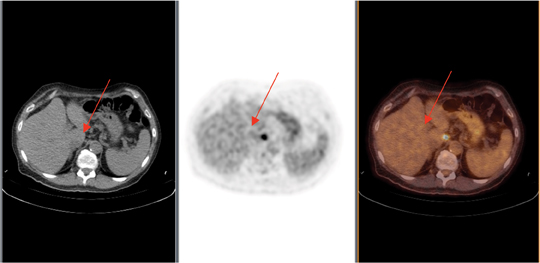
In a recent case, a 65-year-old male presented with a history of laryngeal cancer. Chest, abdomen, and pelvic contrast-CT images revealed an esophageal lesion with no nodal or distant metastases. The PET/CT was ordered for initial treatment strategy. The PET/CT (Figure 1) images revealed a large FDG-avid esophageal mass as well as a 3-mm node FDG-avid abdominal node (Figure 2). While a 3-mm node appeared normal on a CT scan, it was very FDG-avid on PET, demonstrating the metabolic size was significantly larger than the anatomic size (Figure 2). A subsequent biopsy confirmed lymph-node metastases, which changed staging and management in this case.
Expanding neuro-imaging applications
While the majority of PET/CT procedures today are geared toward oncology applications, there are a growing number of PET/CT neurological and cardiovascular imaging studies.10 Most clinical procedures for neurological imaging are for dementia, epilepsy, and brain tumors. Although FDG for brain imaging is still the most important PET/CT tracer, this may change with the recent approval of amyloid tracers for conditions, such as Alzheimer’s Disease. Accordingly, neurological imaging is an area that is expected to experience tremendous growth.
The recent FDA approval of amyloid imaging agents may improve diagnostic evaluation of patients with suspected dementia.8 This coupled with new promising treatment agents may open the door for the routine incorporation of PET in clinical trials in patients with cognitive impairment.
Cardiovascular imaging
In managing patients with known or suspected coronary artery disease, PET/CT is increasingly used to perform tests on the patient at rest or with stress for noninvasive imaging of the perfusion of the heart.9
The introduction of the F-18-based cardiac tracer may present a shift in myocardial nuclear imaging from SPECT to PET. This is possible because image quality in PET is much better than in the SPECT images and is must faster. A whole stress-rest study can be completed in one hour as opposed to 4 hours in the SPECT world.
Astonish TF and PET/CT and F-18-based cardiac tracers will change how nuclear cardiology is being utilized. It will open a whole new area in nuclear cardiology and PET utilization.
Tailored treatment in bariatrics
Another clinical condition that is transforming patient care is obesity. More than 100 million people in the U.S. are defined as obese, 12 million of whom have extreme obesity.10 Along with the increasing number of obese patients comes a growing challenge to diagnostic imaging.
A recent study11 showed TOF scans can help improve lung and liver lesion detectability in heavy patients. This is critical at Saint Louis University School of Medicine, where nearly half of all patients presenting for nuclear medicine exams are obese.
Fundamental to improving image quality in patients with a high BMI is higher sensitivity. The TOF serves as a sensitivity amplifier. On average scanners, to achieve higher detectability of smaller lesions, an injection of a significantly higher dose of FDG may be necessary. But with TOF, small lesions may be detected in obese patients by adjusting imaging protocols and with minimal increase in injected dose. We therefore have higher sensitivity due to the inherent lower signal-to-noise ratio in the TOF scanner.
With solutions like TOF, imaging patients with a large body habitus is feasible.
We use the least amount of radiation, and we are able to produce interpretable scans in patients with high BMI where at other sites these images may be of lower quality.
Transforming patient care for the future
While the adoption of PET for neurological and cardiac imaging promises to revolutionize the future of patient care, we are already seeing a significant transformation today.
We have fast image acquisition, and we are able to detect smaller lesions, produce better quality images independent of body mass index, and on this PET/CT system we can better manage radiation.
Balancing image quality, dose, and scan time no longer has to be a matter of managing tradeoffs. With Astonish TF, we can already strike that balance without compromise.
*Note: Improved image quality is defined by improvements in spatial resolution and/or noise reduction as measured in phantom studies.
References
- American Cancer Society: Cancer Facts and Figures 2012. Atlanta, Ga: American Cancer Society, 2012. Last accessed January 6, 2012.
- Julianne Suhy, BS, CNMT, RT(N), Piotr J. Maniawski, MSc. Routine clinical applications of 4D TOF PET/CT. Philips Healthcare – Nuclear Medicine, Cleveland, OH. http://clinical. netforum.healthcare.philips.com/us_en/Explore/List?modalities=PetCT&documentTypes=White-Papers.
- Lui C, Alessio A, Kinahan PH. Respiratory motion correction for quantitative PET/CT using all detected events with internal—external motion correlation. Med Phys. 2011;38: 2715-2723.
- Erdi YE, Nehmeh SA, Pan T, et al. The CT motion quantitation of lung lesions and its impact on PET-measured SUVs. J Nucl Med. 2004;45:1287-1292.
- Thorndyke B, Schreibmann E, Koong A, Xing L. Reducing respiratory motion artifacts in positron emission tomography through retrospective stacking. Med Phys. 2006;33:2632-2641. doi: 10.1118/1.2207367.
- Nehmeh SA, Erdi YE. Respiratory motion in positron emission tomography/computed tomography: A review. Semin Nucl Med. 2008;38:167-176. doi: 10.1053/j.semnuclmed.2008.01.002.
- Kawano T, Ohtake E, Inoue T. Deep-inspiration breath-hold PET/CT of lung cancer: Maximum standardized uptake value analysis of 108 patients. J Nucl Med. 2008;49:12231231. doi: 10.2967/jnumed.107.049296.
- Yang L, Rieves D, Ganley C. Brain Amyloid Imaging — FDA Approval of Florbetapir F18 Injection. N Engl J Med. 2012;367:885-887. September 6, 2012 DOI:10.1056/ NEJMp1208061.
- Cardiac PET and PET/CT Imaging Practice Guidelines. A summary of the recommendations and practice guidelines of professional groups. SNM PET Center of Excellence. http:// www.snm.org/docs/PET_PROS/CardiacPracticeGuidelinesSummary.pdf. May 2009.
- Gordon-Larsen P, Adair LS, Nelson MC, Popkin BM. Five-year obesity incidence in the transition period between adolescence and adulthood: The National Longitudinal Study of Adolescent Health. Am J Clin Nutr. 2004;80:569-575.
- El Fakhri et al. Improvement in lesion detection with whole-body oncologic time-of-flight PET. J Nucl Med. 2011; 52:347-353.
Citation
Striking a balance in PET imaging transforms patient care. Appl Radiol.
December 10, 2012