Spontaneous Intestinal Perforation
Images

Case Summary
A neonate, born at 29 weeks’ gestation, was transferred with moderate abdominal distention and a large volume pneumoperitoneum. Upon arrival to the neonatal intensive care unit, the infant underwent peritoneal drain placement. At 2 weeks of age the infant developed recurrent pneumoperitoneum with associated leukocytosis. An exploratory laparotomy was performed to identify and treat the presumed bowel perforation. An abscess cavity was identified in the right lower quadrant with associated ileal perforation approximately 4 cm from the ileocecal valve. This abscess was drained, and the abnormal bowel was resected. No cause for the ileal perforation was identified.
Imaging Findings
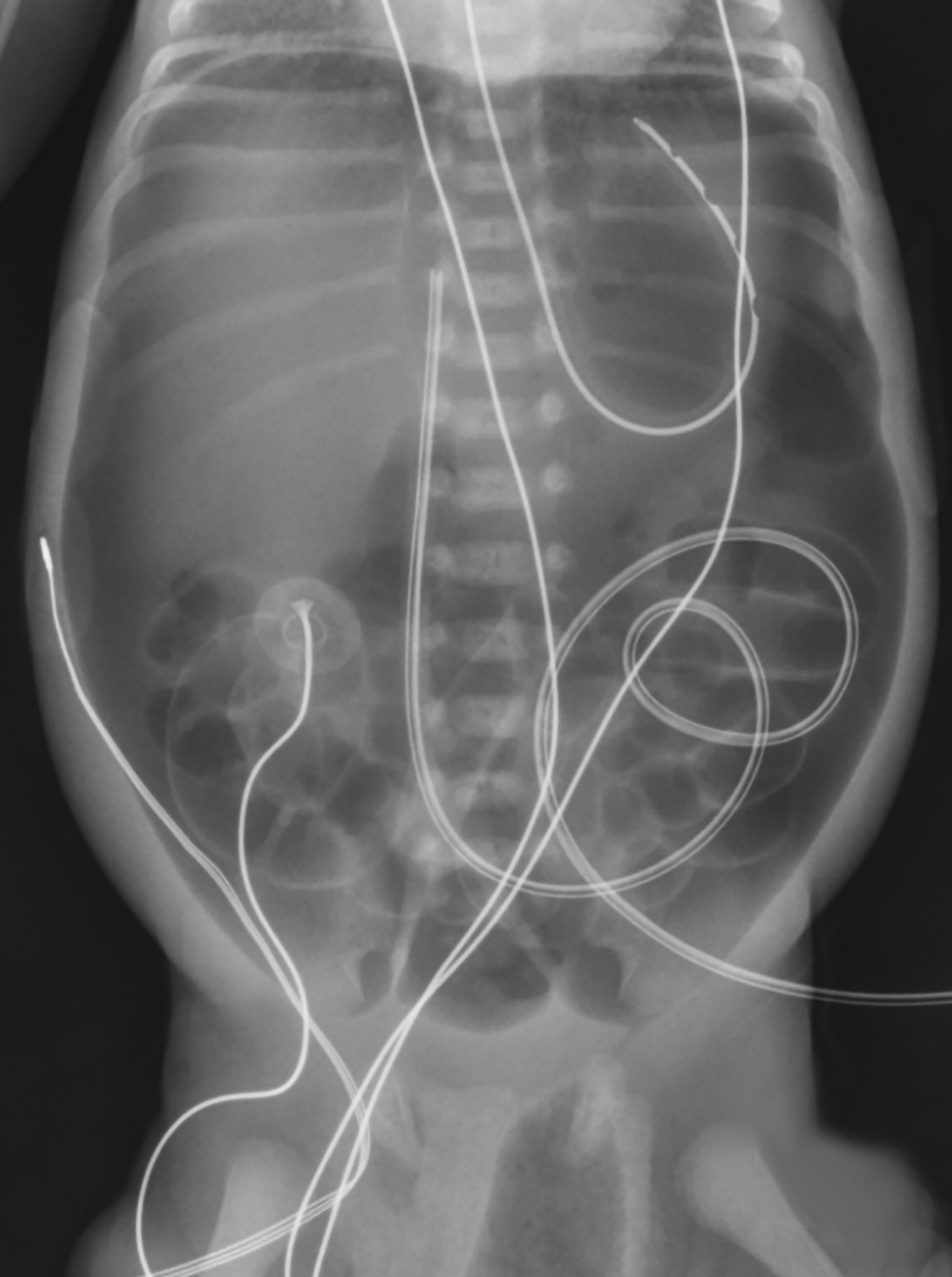
Abdominal radiograph at 2 days of life revealed a large amount of pneumoperitoneum with a nonobstructive bowel gas pattern (Figure 1).
Diagnosis
Spontaneous intestinal perforation.
Enterocolitis (NEC) is the most common cause of neonatal pneumoperitoneum. Less common causes include perforation related to bowel obstruction caused by meconium ileus, Hirschsprung disease, or intestinal atresia.1
Discussion
Spontaneous intestinal perforation (SIP) is a focal bowel perforation without gross intestinal necrosis and lacking the radiographic and pathologic findings of NEC.2 One study estimated the incidence of SIP to be 1 in 5000 live births.3 SIP is more common in premature, low birth weight, and male infants with African American ancestry.2,4-6 Its etiology is unknown. However, several potential mechanisms have been hypothesized, including a congenital absence of intestinal musculature in the perforated segment, a focal area of ischemia, or fungal infection.3-7 Risk factors for SIP include a history of a patent ductus arteriosus with subsequent indomethacin treatment; a need for vasopressors; presence of an umbilical artery catheter, surfactant or steroid administration; and maternal antibiotic administration during labor/delivery.4-6, 8
It is often difficult to distinguish SIP from NEC. Neonates with SIP most commonly present with discoloration of the abdomen or inguinal region, sudden onset abdominal distention, and a decrease in bowel sounds.2,4-7 Signs of infection such as abdominal wall rigidity and tenderness are associated with NEC but are often absent in SIP.2,5 While there is variation in the reported age of onset, SIP is generally diagnosed within the first 2weeks of life.2-4,6,10 The average gestational age and birth weight is lower in cases diagnosed with SIP as compared to those diagnosed with NEC.
The diagnosis of SIP can be based on radiologic and pathologic findings. Plain abdominal radiographs often show a large volume of pneumoperitoneum but pneumatosis intestinalis is not present.2,4,7,8 At surgery a localized area of perforation is visible.2,6 SIP most commonly affects the ileum, as in our patient.4,5,8 Laboratory findings are nonspecific, but leukocytosis and thrombocytopenia may be suggestive of SIP.2,4,5
The standard treatment for SIP is laparotomy with resection of the perforated segment. A peritoneal drain often placed to drain residual fluid and gas.9 The survival rate is higher for SIP than for NEC, perhaps due to earlier detection and limited bowel involvement.2,6 Postoperative complications can include intestinal obstruction (19%), fistula formation and wound complications (13%), and sepsis with death (6%).4 However, the risk of adverse outcomes is greater with perforation from NEC than SIP.6 Unlike with NEC, SIP does not have long-term gastrointestinal complications.10
Conclusion
Spontaneous intestinal perforation should be considered in the premature neonate presenting with abdominal wall discoloration, distention, and a large volume of intraperitoneal free air. An abdominal radiograph can be used for diagnosis, showing free intraperitoneal air. In contrast to NEC, pneumatosis intestinalis is not present.
References
- Gupta R, Bihari Sharma S, Golash P, Yadav R, Gandhi D. Pneumoperitoneum in the newborn: is surgical intervention always indicated? J Neonatal Surg. 2014 Jul 10;3(3):32.
- Okuyama H, Kubota A, Oue T, Kuroda S, Ikegami R, Kamiyama M. A comparison of the clinical presentation and outcome of focal intestinal perforation and necrotizing enterocolitis in very-low-birth-weight neonates. Pediatr Surg Int. 2002 Dec;18(8):704-706.
- Attridge JT, Clark R, Walker MW, Gordon PV. New insights into spontaneous intestinal perforation using a national data set: (2) two populations of patients with perforations. J Perinatol. 2006 Mar;26(3):185-188.
- Ragouilliaux CJ, Keeney SE, Hawkins HK, Rowen JL. Maternal factors in extremely low birth weight infants who develop spontaneous intestinal perforation. Pediatrics. 2007 Dec;120(6):e1458-464.
- Meyer CL, Payne NR, Roback SA. Spontaneous, isolated intestinal perforations in neonates with birth weight less than 1,000 g not associated with necrotizing enteroco- litis. J Pediatr Surg. 1991 Jun;26(6):714-717.
- Shah J, Singhal N, da Silva O, Rouvinez-Bouali N, Seshia M, Lee SK, Shah PS; Canadian Neonatal Network. Intestinal perforation in very preterm neonates: risk factors and outcomes. J Perinatol. 2015 Aug;35(8):595-600.
- Litwin A, Avidor I, Schujman E, Grunebaum M, Wilunsky E, Wolloch Y, Reisner SH. Neonatal intestinal perforation caused by congenital defects of the intestinal musculature. Am J Clin Pathol. 1984 Jan;81(1):77-80.
- Gordon PV, Swanson JR, Attridge JT, Clark R. Emerging trends in acquired neonatal intestinal disease: is it time to abandon Bell’s criteria? J Perinatol. 2007 Nov;27(11):661-671.
- Eltayeb AA, Hashem M. Management and outcome of neonatal bowel perforation. Ann Pediatr Surg. 2008;4:83-88.
- Tiwari C, Sandlas G, Jayaswal S, Shah H. Spontaneous intestinal perforation in neonates. J Neonatal Surg. 2015 Apr 1;4(2):14.
References
Citation
AJ KPPTTRSCLYT.Spontaneous Intestinal Perforation. Supplement to Applied Radiology. 2022; (5):6-7.
September 2, 2022