SIR 2019: Virtual reality could replace fluoroscopy for catheter image guidance
Images
Immersive virtual reality (VR) using real-time, three-dimensional (3D) images of the interior of a patient’s blood vessels could eventually replace conventional fluoroscopy for guiding catheterization, according to researchers presenting this week at the Society of Interventional Radiology (SIR)’s annual meeting in Austin, TX.
The researchers, interventional radiologists from the University of Washington, described how a catheter with electromagnetic sensors projecting images to a VR headset could be used to steer the catheter, providing faster, more efficient treatment with greater precision and with less radiation exposure than fluoroscopy.
“Virtual reality will change how we look at a patient’s anatomy during an IR treatment,” said Wayne Monsky, MD, PhD, professor of radiology and lead author of the study. “This technology will allow physicians to travel inside a patient’s body instead of relying solely on two-dimensional (2D) black and white images, which are limited in the level of detail they provide.”
Dr. Monsky’s group created a 3D-printed vasculature model and a holographic image of blood vessels of a patient’s abdomen and pelvis using a computed tomography (CT) angiogram. As a catheter was guided through the 3D model, a transmitter projected an electromagnetic field that tracked sensors attached to the catheter. The sensors’ location and rotation with spatial coordinates relative to the transmitter’s origin were translated in real-time from the transmitter’s coordinate system to the common coordinate system in VR, Dr. Monsky explained. The tracking system displayed the image from the catheter through the VR headset.
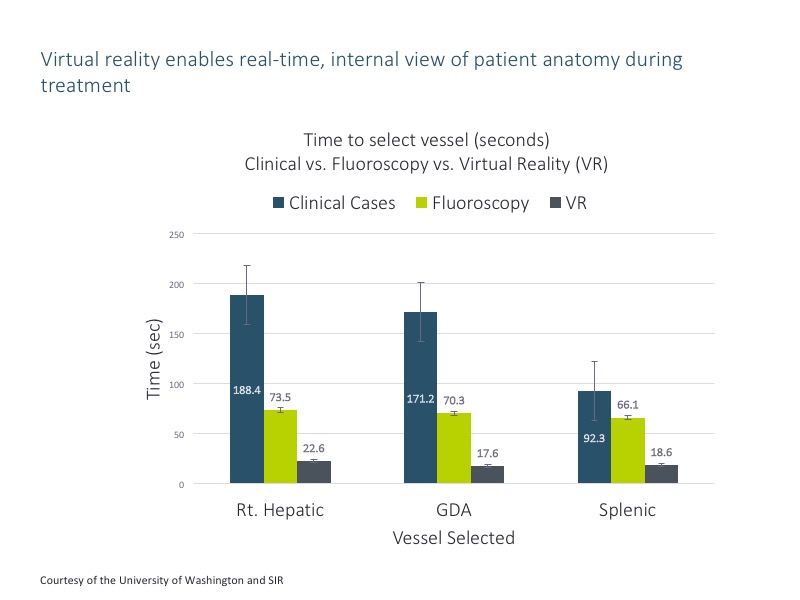
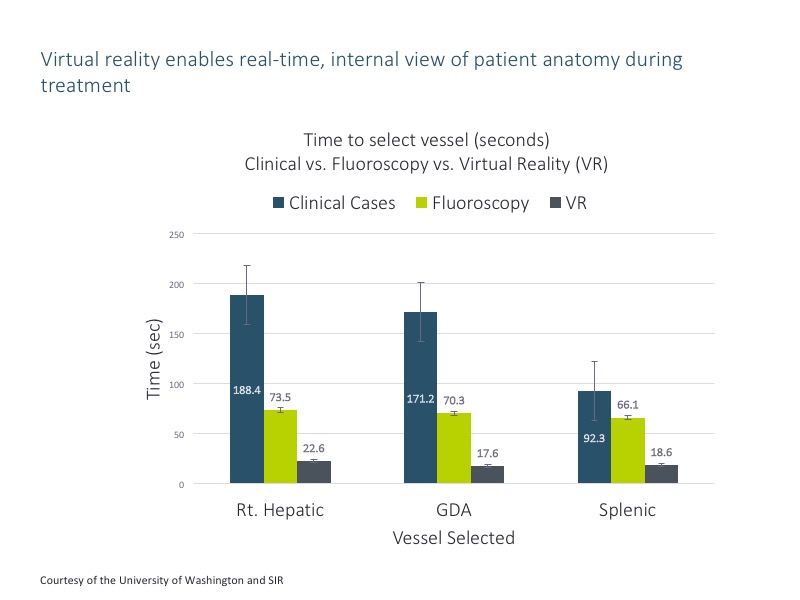
As they simulated catheterization, the researchers compared the time it took to steer the catheter from the entry point of the femoral artery to three targeted vessels with conventional fluoroscopic guidance as well as the time to perform similar real-life clinical angiographic procedures. In 18 simulations, the mean time to reach the vessels using VR was much lower than with fluoroscopy. For example, VR took 17.6 seconds compared to 70.3 seconds for fluoroscopy, and the real-life procedure took 171.2 seconds, said Dr. Monsky.
“Our pilot feasibility research suggests we may soon be performing endovascular treatments visualizing the vasculature and catheter in VR,” said Dr. Monsky. “VR offers an immersive display of vasculature and the electromagnetically tracked coregistered catheter, and allows visualization inside of the patient from perspectives never before possible. By reducing the amount of radiation exposure to both patients and physicians, VR could also create safer treatments.”
Dr. Monsky said he and his colleagues are continuing to conduct research in 3D models as well as in animals. The VR software was developed through a University of Washington business incubator that supported development of a startup, Pyrus Medical of Seattle. Dr. Monsky serves as the chief medical officer of the company, which is preparing to submit their work to the U.S. Food and Drug Administration (FDA) for approval.
Citation
SIR 2019: Virtual reality could replace fluoroscopy for catheter image guidance. Appl Radiol.
March 27, 2019