Septic arthropathy of the sacroiliac joint
Images




Pyogenic arthritis of the left sacroiliac joint and abscess related to Streptococcus pneumonia
Findings
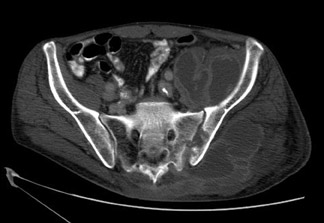
An AP radiograph of the pelvis demonstrated subtle erosive changes of the left sacroiliac joint with a large soft mass in the left gluteal soft tissues (Figure 1). A subsequent CT scan of the abdomen and pelvis (with oral and IV contrast) was obtained for further characterization.
CT examination of the abdomen and pelvis (with oral and IV contrast) demonstrated a large, complex, multiloculated fluid collection involving the left gluteal musculature, left illiacus muscle, left obturator internus muscle, left iliopsoas muscle, and the left iliopsoas bursae (Figures 2A, C and D) In addition, bone windows demonstrated erosive changes in the left sacroiliac joint (Figure 2B). Overall, the findings were consistent with septic arthropathy of the left sacroiliac joint with a large adjacent abscess. Subsequent surgical incision and drainage, along with blood cultures yielded Streptococcus pneumonia.
Discussion
Bacterial arthritis of the sacroiliac joint is relatively uncommon, accounting for 1% to 4% of all cases of septic arthritis.1 Risk factors include pregnancy, trauma, immunocomprised status, rheumatoid arthritis, intravenous drug abuse, and coexistent infection.2–5 Most cases are related to a hematogenous source of infection. Contiguous spread of infection from an adjacent source infection or direct implantation (related to manipulation) are less likely causes.1,2
Patients with pyogenic sacroilitis typically present with unilateral sacroiliac pain, sciatica, fever, leuckocystosis, and an elevated sedimentation rate. Patients with subacute pyogenic sacroilitis are often difficult to diagnose, and can be clinically confused with other conditions such as disc herniation, pyelonephritis, appendicitis or diverticulitis. Evaluation with radiographs, CT, magnetic resonance imaging (MRI) andnuclear medicine have all been shown to be useful in making an accurate diagnosis.2 However, joint aspiration is required to confirm the diagnosis, and to identify the specific infectious agent.
Streptococcus pneumonia is an uncommon cause of septic arthritis, causing 6% of all cases. Half of adults with Streptococcus pneumonia septic arthropathy had another focus of pneumococcal infection. Most patients respond well with antibiotic treatment.6,7
Conclusion
In the proper clinical setting, erosive changes within the sacroiliac joint, along with an effusion are considered highly suspicious for septic arthritis. The presence of an adjacent fluid collection (abscess) would further support this diagnosis. Recognition of these radiographic findings can be critical to making the diagnosis and decreasing patient morbidity.
- Brusch, JL. Septic Arthritis. EMedicine. 2005:Oct 18,1-16. Available at: http://www.emedicine.com/ MED/topic671.htm. Accessed online: December 29, 2009.
- Resnick. Osteomyelitis, Septic Arthritis, and Soft Tissue Infection: Axial Skeleton. Bone and Joint Imaging 2nd ed. Philadelphia, PA: W.B. Saunders; 1996:674-683.
- O’Brien CM, Darley ES, Kelly AJ, et al. Septic sacroiliitis: An unusual causative organism in a rare condition. Int J Clin Pract. 1998;52:206-207.
- Karchevsky M, Schweitzer ME, Morrison WB, Parellada, JA. MRI findings of septic arthritis and associated osteomyelitis in adults. AJR Am J Roentgenol. 2004;182:119122.
- Brower AC. Septic arthritis. Radiol Clin North Am. 1996;34:293-309.
- Pinson AG, Jolles PR, Balkissoon AR. Pneumococcal sacroiliitis. South Med J. 1997;90:649-652.
- Ross JJ, Saltzman CL, Carling P, Shapiro DS. Pneumococcal septic arthritis: Review of 190 cases. Clin Infect Dis. 2003;36:319-327. Comment in Clin Infect Dis. 2004;38:1645-1646.
Citation
Septic arthropathy of the sacroiliac joint. Appl Radiol.
March 4, 2010