Sepsis-induced Rapid Left Ventricular Calcification
Images
Case Summary
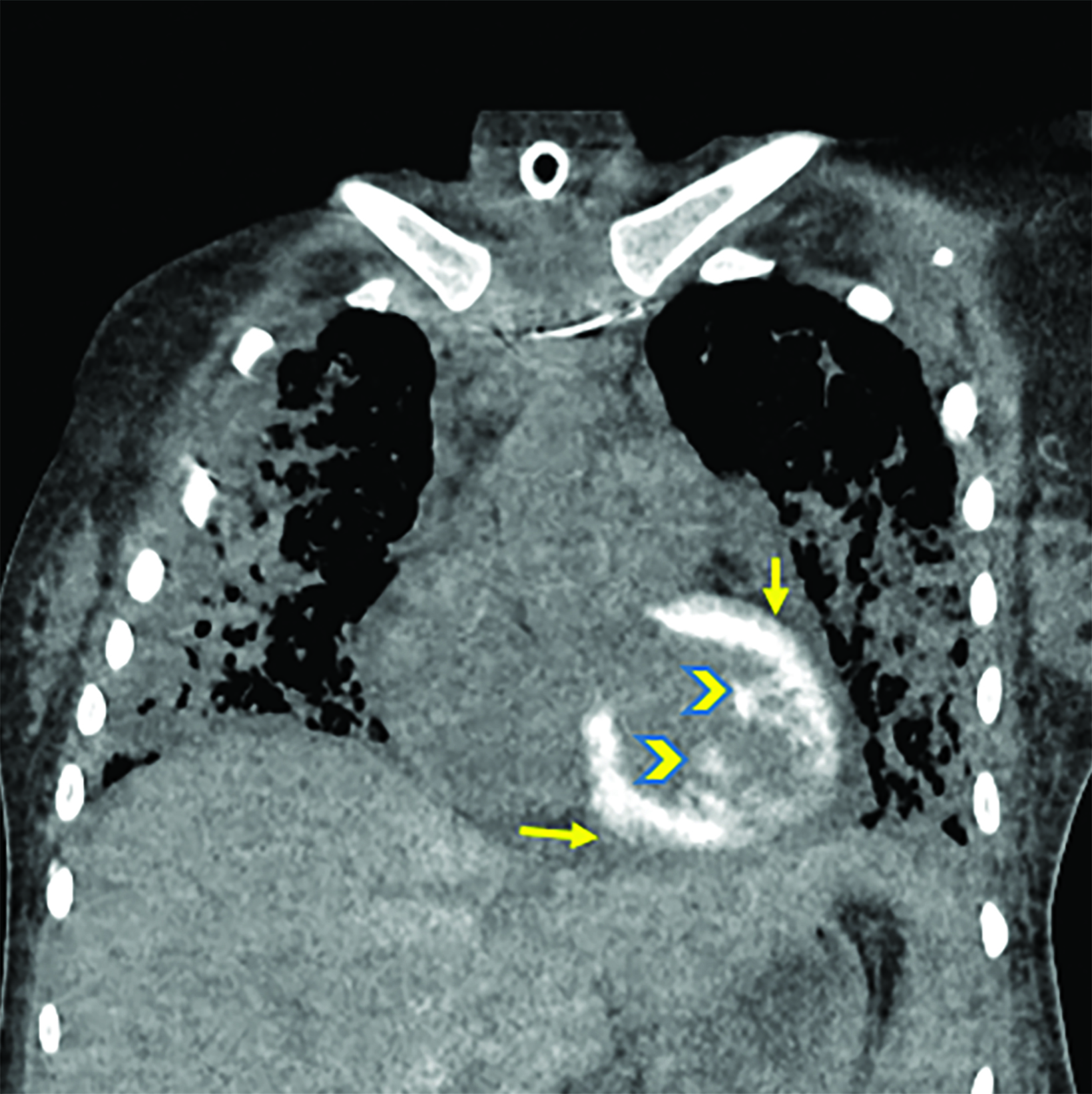
An adult presented to the emergency department with fever and sepsis 7 days postpartum. Pregnancy course and delivery were uncomplicated. Blood cultures were positive for group A streptococcus, and aggressive antibiotics and supportive management were initiated. Shortly afterward, the patient arrested and was placed on extracorporeal membrane oxygenation (ECMO) after attempts to restore cardiac rhythm failed. Acute renal failure, disseminated intravascular coagulation (DIC), and generalized ecchymosis with skin blisters occurred on the second day. A noncontrast computed tomography (CT) scan of the chest on day 5 revealed acute respiratory distress syndrome (ARDS) and early calcification of the left ventricular papillary muscles and myocardium with sparing of the endocardium. This finding was confirmed by echocardiography. The calcifications appeared more dense on follow-up CT images; however, the cardiac ejection fraction (EF) was within normal limits (60%).
Imaging Findings
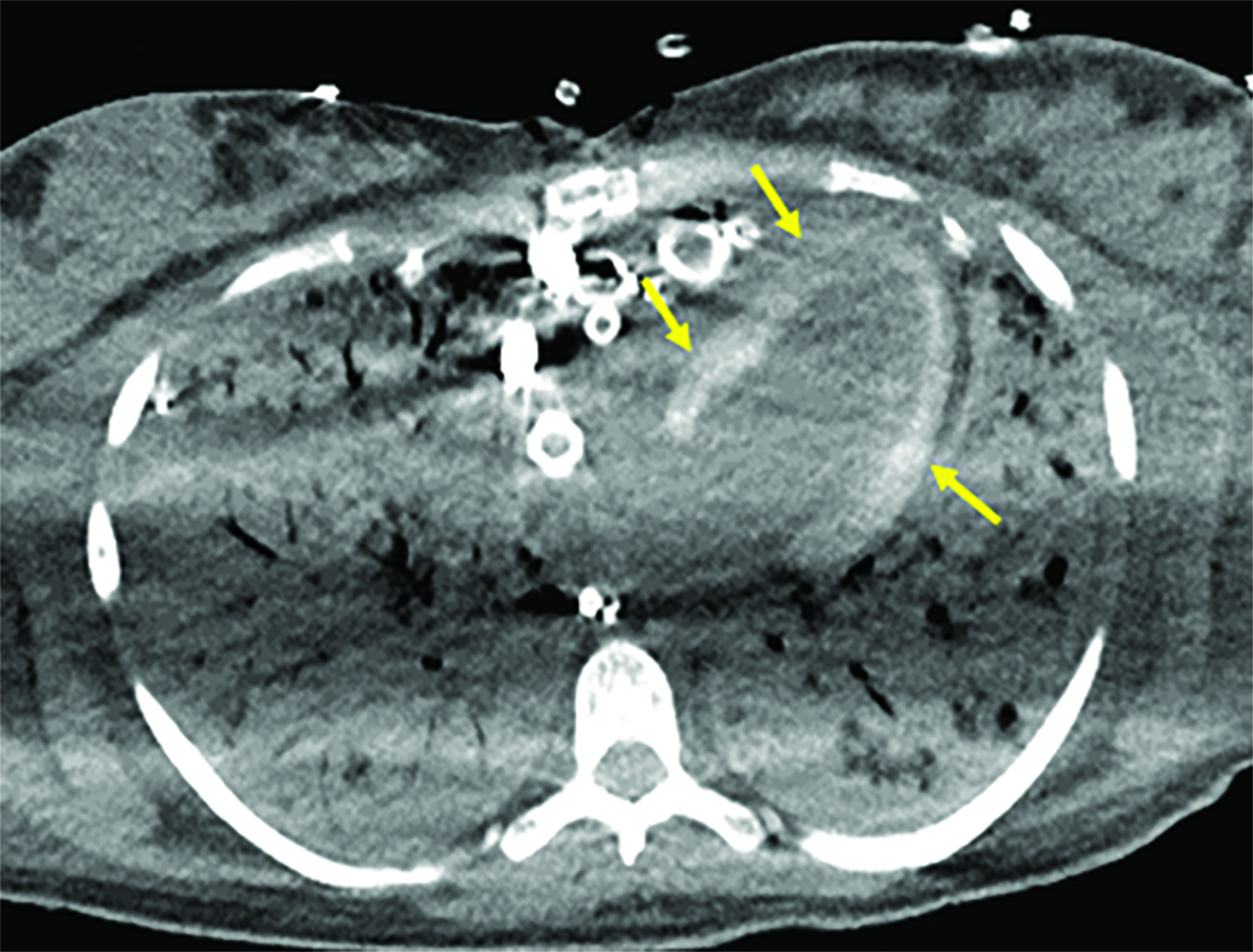
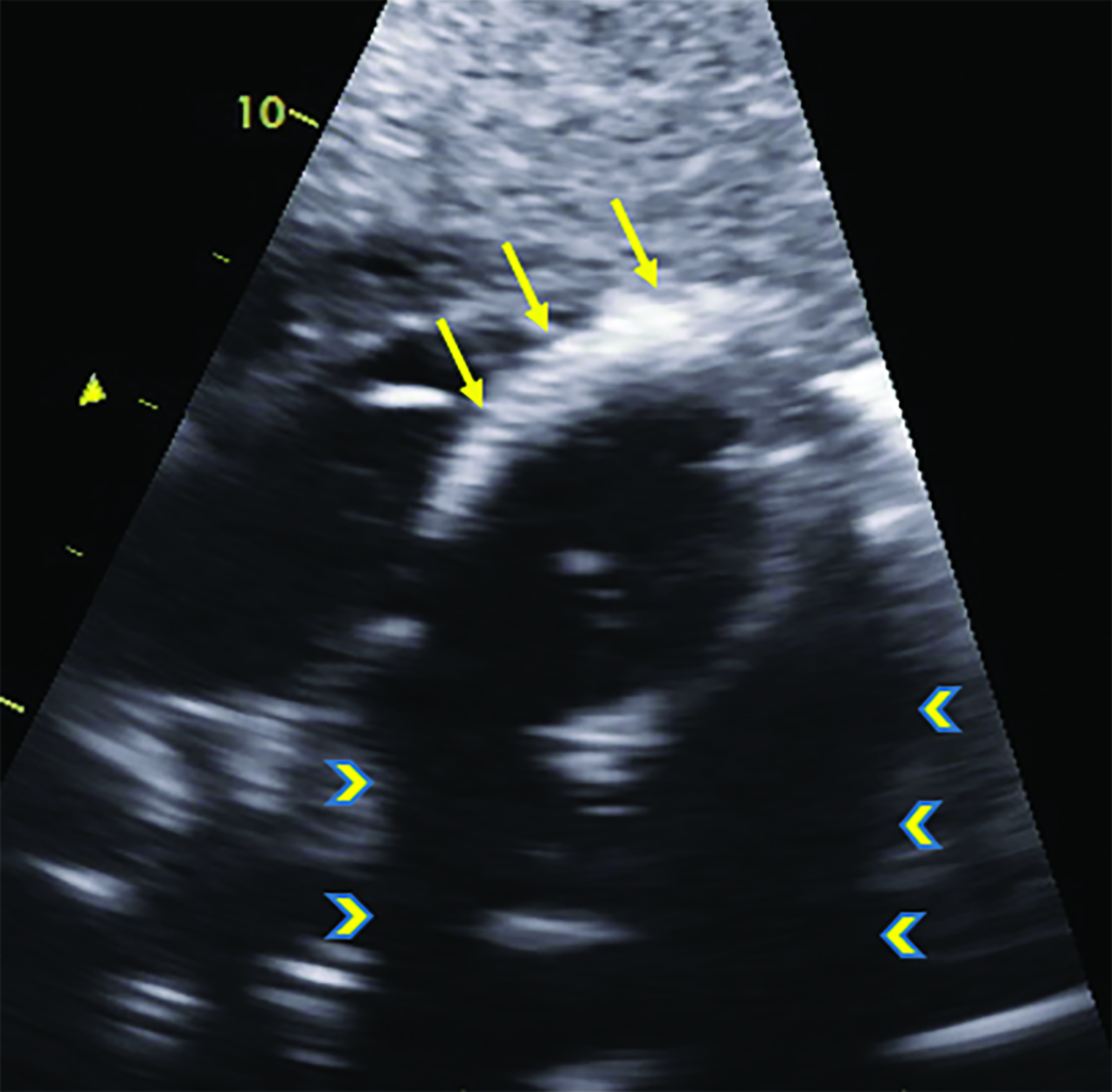
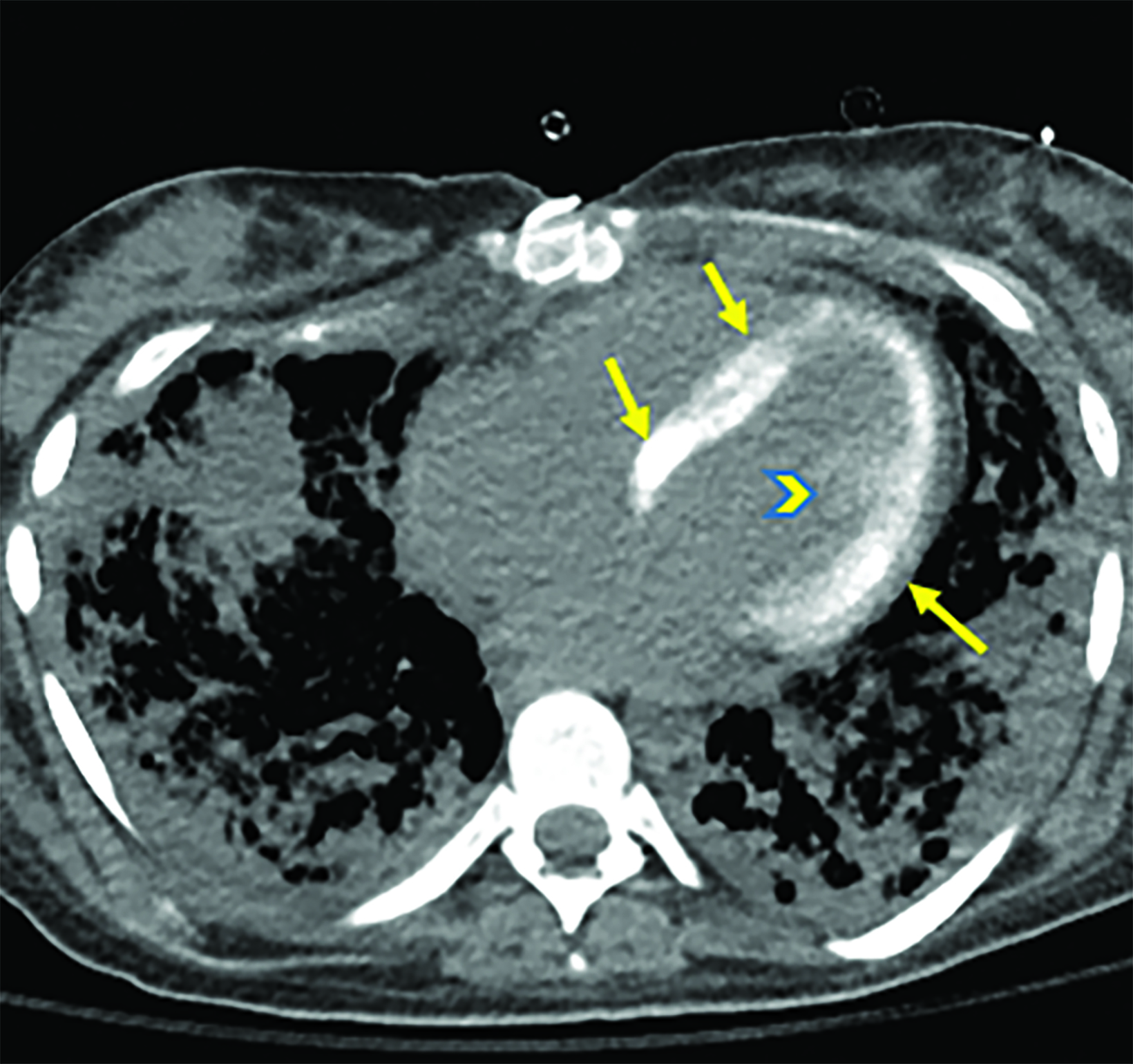
Noncontrast chest CT demonstrated ARDS and early diffuse calcifications involving the left ventricle myocardium and the papillary muscles (Figure 1). However, serum calcium and phosphorus were not elevated and no dystrophic calcifications were noted elsewhere. These finding were confirmed by trans-esophageal echocardiography, which showed dense left ventricle myocardium (Figure 2). These calcifications did not significantly affect the left ventricular EF, which was 60% (n = ≥55%). Follow-up CT chest one month later revealed progressive left ventricular calcification (Figure 3).
Diagnosis
Sepsis-induced dystrophic left ventricular calcification
Discussion
Dystrophic calcification is a sequel of tissue necrosis that is not associated with elevated serum calcium or renal failure. A suggested explanation for the mechanism of calcification is that membrane damage leads to calcium-ion concentration within membrane-bound vesicles that is then hydrolyzed. The phosphate released from the membrane phospholipids binds to calcium, which gets deposited in the tissues. The most common etiology is myocyte necrosis, which may result from myocardial infarction, sepsis, trauma, or infection.1 Metastatic calcification is a common sequelae of a systemic disorder with abnormal calcium homeostasis affecting normal and diseased tissues.1 Myocardial calcification may also be idiopathic.
The development of myocardial calcification may also be multifactorial. There are several reported cases of extensive post-heart transplantation calcification that could be due to a combination of cellular rejection, renal failure, cardiac trauma, and/or steroid use.2, 3 Cases of rapidly developing cardiac calcifications may be linked to more than one pathogenesis.
Computed tomography is the modality of choice for assessing the extent and involvement of myocardial calcifications. Dystrophic calcifications tend to be more linear, focal, and localized as compared with metastatic calcifications, which are more diffuse and unstructured.4 Infection and inflammatory etiologies present as circumferential linear or diffuse deposits similar to this case.5 Calcifications may cause arrhythmias, abnormal wall movements, restrictive cardiomyopathy, or sudden death.6
Proper description of calcification location, extent, and involvement of pericardium or valves is important for diagnosis. Additionally, documenting the presence of extracardiac calcium deposits helps differentiate types of cardiac calcification and shortens the differential diagnosis.
Conclusion
Various etiologies contribute to myocardial calcification. The most common classification is dystrophic, metastatic, or idiopathic.7 The
presence of myocardial calcifications is an indication of underlying local or systemic pathology. These calcifications can be visualized by radiography, CT, and echocardiography. Properly describing the calcification pattern on imaging helps to narrow the differential diagnosis and potential etiology.
References
- Perkins JA. Tissue Renewal, Regeneration, and Repair. In: Perkins JA, ed. Robbins and Cotran Pathologic Basis of Disease. Eighth Edition. Philadelphia: WB Saunders; 2010:79-110.
- Cohnert TR, Kemnitz J, Haverich A, et al. Myocardial calcification after orthotopic heart transplantation. J Heart Transpl. 1988;7:304-308.
- Pardo-Mindan FJ, Herreros J, Marigil MA, et al. Myocardial calcification following heart transplantation. J Heart Transpl. 1986;5:332-335.
- Freeman J, Dodd JD, Ridge CA, et al. “Porcelain heart” cardiomyopathy secondary to hyperparathyroidism: radiographic, echocardiographic, and cardiac CT appearances. J Cardiovasc Comput Tomogr. 2010;4:402-404.
- Lapatto-Reiniluoto O, Vaalamo M, Takkunen O, et al. Left ventricular calcification following resuscitation. J Intern Med. 2000;248:85-87.
- Okada M, Kyakuno M, Imamura J, et al. An autopsy case of sudden death in renal transplant recipient. Clin Transpl. 2002;16(Suppl 8):58-61.
- Gowda RM, Boxt LM. Calcifications of the heart. Radiol Clin North Am. 2004; 42(3):603-617, vi-vii. doi: 10.1016/j.rcl.2004.03.010. PMID: 15193932.
References
Citation
S M, A K, T L.Sepsis-induced Rapid Left Ventricular Calcification. Appl Radiol. 2022; (3):47-49.
April 26, 2022