Renovascular hypertension caused by compressive adenopathy with hypertensive encephalopathy
Images

CASE SUMMARY
A 28-year-old man presented to the emergency department with an abdominal mass and five days of headache with nausea and vomiting. He was two months status post radical inguinal orchiectomy for right testicular mature teratoma with retroperitoneal and mediastinal nodal metastases, with no follow up after surgery because of a lack of health insurance. His medical history was otherwise negative. His blood pressure was 152/107 mmHg. On exam he had an obvious protrusion of an abdominal mass right of midline that was hard and non-tender. Computed tomography (CT) of the abdomen and pelvis and magnetic resonance imaging (MRI) of the head were performed. The patient required quadrivalent antihypertensives to normalize his blood pressure, which relieved his headache and nausea. He received chemotherapy (etoposide, ifosfamide, mesna, cisplatin) for seven consecutive days as an inpatient, and was discharged without further need of antihypertensive medication.
IMAGING FINDINGS
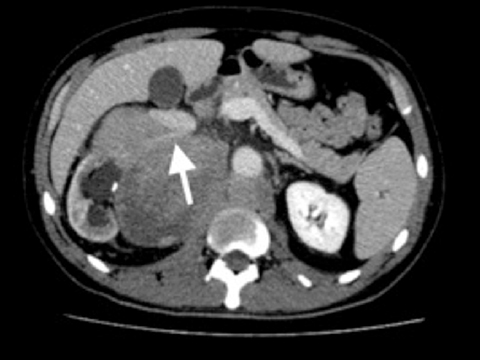
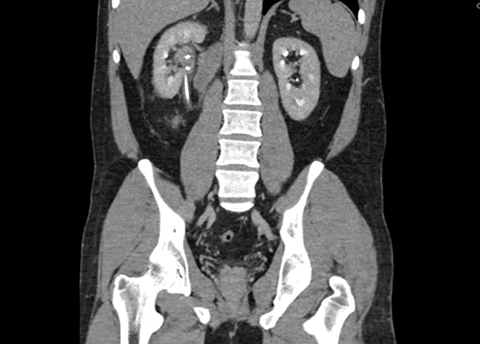
A contrasted CT scan of the abdomen and pelvis demonstrated bulky, conglomerated retroperitoneal lymphadenopathy measuring 18 × 15 × 26 cm. The right kidney was displaced laterally and compressed. The nodal masses engulfed and compressed the renal artery and vein (Figure 1a). There was moderate hydronephrosis and a well-positioned ureteral stent (Figure 1b). A CT-guided fine needle aspiration of this perinephric mass was consistent with the patient’s known testicular teratoma.
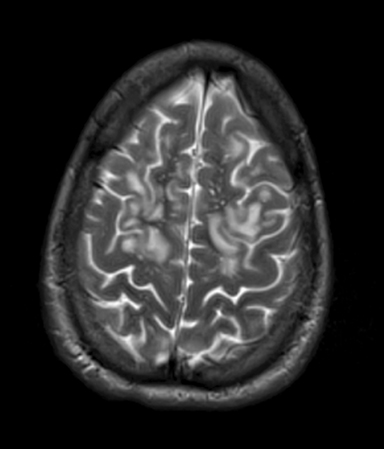
An MRI examination of the head revealed confluent signal hyperintensity on T2 and FLAIR pulse sequences in the subcortical white matter of the cerebral hemispheres bilaterally (Figure 2). The frontal lobes were predominantly involved in a bilaterally symmetric fashion. Differential diagnostic considerations for these radiologic findings included atypical posterior reversible encephalopathy syndrome (PRES), vasculitis, viral encephalitis, and acute disseminated encephalomyelitis (ADEM).
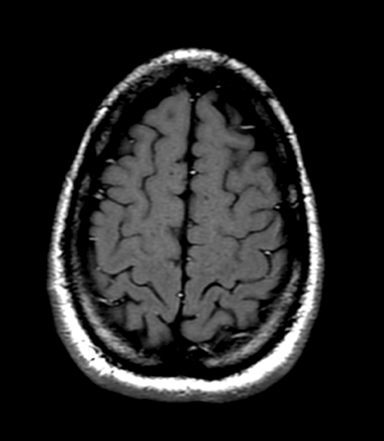
Follow up CT performed after chemotherapy showed near-complete resolution of the patient’s lymphadenopathy and resultant relief of the right kidney compression (Figure 3). Follow up brain MRI confirmed resolution of the subcortical T2/FLAIR signal abnormalities (Figure 4).
DIAGNOSIS
Renovascular hypertension caused by compressive adenopathy with hypertensive encephalopathy
DISCUSSION
This patient’s bulky retroperitoneal metastatic lymph nodes displaced the right kidney laterally and compressed the right renal artery and vein. Obstruction of the renal perfusion leads to renal ischemia with subsequent excretory dysfunction1 and activates the renin-angiotensin system.1 This patient’s serum renin level was not measured, but the activation of the renin-angiotensin-aldosterone system can be inferred from his elevated blood pressure of 152/107 mmHg in a young, previously normotensive patient, and elevated BUN to creatinine ratio (44 mg/dL:1.84 mg/dL), and low serum potassium (3.1 mEq/L). Although renovascular hypertension is nearly always caused by atherosclerosis or fibromuscular dysplasia,1 there have been reports of a wide range of etiologies extrinsic to the renal arteries,1 including a case of tuberculous retroperitoneal adenopathy that responded to treatment, reversing the hypertension.2 This patient’s large retroperitoneal nodal metastases with obvious compression of the kidney on CT presents a similar case with similar clinical course.
Posterior reversible encephalopathy syndrome (PRES) is a unique pattern of brain edema that manifests in the setting of neurotoxicity.3 Eclampsia, sepsis, autoimmune disease, cancer chemotherapy, transplantation, and hypertension are clinical scenarios associated with PRES,3 with hypertension the most common and classic scenario.4 PRES occurs when endothelial dysfunction or failure of the cerebral autoregulation leads to cerebral edema,5 and can cause seizures, headache, nausea, vomiting, altered mental status, and visual disturbances.4,6 The cerebral edema is best seen as hyperintensity on FLAIR images,6 and manifests in characteristic patterns on MRI, with the parieto-occipital regions the most commonly involved (94%), followed by the frontal lobe (77%), temporal lobe (64%), and cerebellum (53%),4 basically following the watershed zones.3 Diffusion- weighted imaging generally shows lack of diffusion restriction.3,6 It is usually bilaterally symmetric, and resolves with treatment of the underlying cause.3
CONCLUSION
Renovascular hypertension is most commonly caused by artherosclerosis or fibromuscular dysplasia. However, it may also be caused by extrinsic compression of the renal vessels. Posterior reversible encephalopathy syndrome (PRES) may result from hypertension of any cause, including renovascular hypertension. This is an unusual case of a young patient with encephalopathic symptoms, new-onset hypertension, and bulky retroperitoneal metastasis of right testicular teratoma. CT demonstrated that the metastasis was compressing the right renal artery, causing renovascular hypertension, which in turn led to PRES. The PRES resolved with anti-hypertensive treatment. The retroperitoneal nodes responded to cisplatin treatment, relieving the compression of the renal artery, and allowing for cessation of anti-hypertensives. The patient was discharged to outpatient follow-up with his oncologist.
REFERENCES
- Weber BR, Dieter RS. Renal artery stenosis: epidemiology and treatment. Int J Nephrol Renovasc Dis. 2014;13(7):169-181.
- Puri S, Khurana SB, Malhotra S. Tuberculous abdominal lymphadenopathy causing reversible renovascular hypertension. J Assoc Physicians India. 2000;48(5):530-532.
- Bartynski WS. Posterior reversible encephalopathy syndrome, part 1: fundamental imaging and clinical features. Am J Neuroradiol. 2008;29(6):1036-1042.
- Fugate JE, Claassen DO, Cloft HJ, Kallmes DF, Kozak OS, Rabinstein AA. Posterior reversible encephalopathy syndrome: associated clinical and radiologic findings. Mayo Clinic Proceedings. 2010;85(5):427-432.
- Bartynski WS. Posterior reversible encephalopathy syndrome, part 2: controversies surrounding pathophysiology of vasogenic edema. Am J Neuroradiol. 2008;29(6):1043-1049.
- McKinney AM, Short J, Truwit CL, McKinney ZJ, Kozak OS, SantaCruz KS, M. Posterior reversible encephalopathy syndrome: incidence of atypical regions of involvement and imaging findings. Am J Roent. 2007;189(4):904-912.
Citation
K M, R M, D S.Renovascular hypertension caused by compressive adenopathy with hypertensive encephalopathy. Appl Radiol. 2016; (7):32C-32D.
July 2, 2016