Radiological Case: Dural chondroma
Images


CASE SUMMARY
An 18-year-old female presented with a 1-year history of headache with vomiting and convulsions for the immediately preceding 2months. Papilledema was present on fundoscopy. A CT brain was performed.
IMAGING FINDINGS
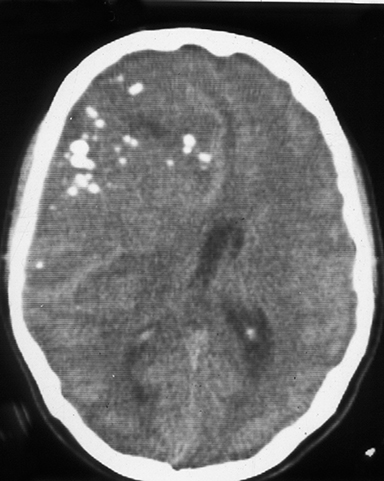
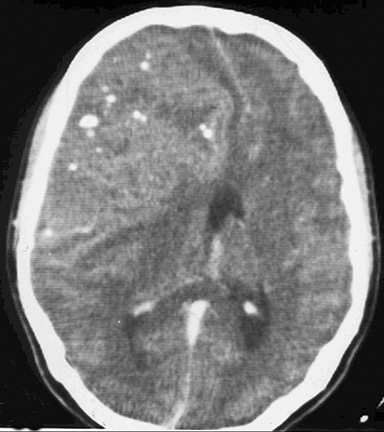
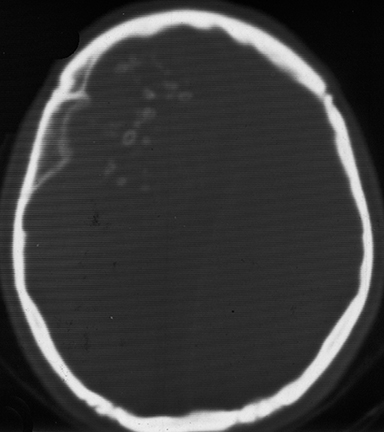
The CT scan (Figures 1A-1C) revealed a large, lobulated, iso- to hypodense, extra-axial lesion with diffuse nodular areas of calcification in the right frontoparietal region. The lesion showed moderate contrast enhancement with few nonenhancing areas. The lesion crossed the midline and had caused anterior subfalcine herniation. However, no perilesional edema was present. Hyperostosis of the underlying skull vault was evident. At craniotomy, a large tumor was attached to the dura of the convexity but easily separable from the surrounding brain parenchyma. The tumor, along with its attachment to the convexity dura, was completely removed. Macroscopically, the tumor was a dural-based firm mass with a lobulated grayish-white surface (Figure 2). Microscopic examination revealed well-differentiated hyaline cartilage arranged in lobules; there were no atypical cells, multinucleation, or mitotic activity (Figure 3).
DIAGNOSIS
Dural chondroma
DISCUSSION
Intracranial chondromas are rare, benign, cartilaginous tumors that constitute about .2 to .3% of all primary intracranial tumors.1,2 They usually originate from the bones of the skull base, at the sphenoethmoidal and spheno-occipital regions, but very rarely can also arise from other intracranial, extra osseous sites like the dura mater, the brain parenchyma or from within the ventricles.3 Lacerte et al,4 reported 2 cases of dural chondroma (one from convexity and other from falx) and compared them with 45 cases of intracranial chondroma reported in the literature in which the tumor had originated outside the skull base. Of these, 34 (72%) arose from the meninges, and 19 arose from the convexity dura. In our review of literature we found 22 cases in which the tumor arose from the convexity dura. Intracranial chondromas may coexist with similar growths in other bones, with a systemic predisposition for such tumors in Ollier’s multiple enchondromatosis5 and Maffuci’s syndrome.
Skull-base chondromas are usually extradural and presumed to arise from embryonic cartilage rests along the basilar synchondroses. The origin of dural chondromas is more controversial. Cartilaginous metaplasia of meningeal fibroblasts, ectopic embryologic rests of cartilage cells, metaplasia of perivascular mesenchymal tissue, or traumatic displacement of cartilaginous elements have all been proposed.6
Clinically, patients with intracranial chondromas often present with longstanding symptoms that can be attributed to the slow-growing nature of these tumors. Headache,seizures, focal neurological deficits, and signs of increased intracranial tension maybe present.7 Chondromas are characterized by their large size at presentation, as was the case in our patient. Unlike meningiomas, chondromas do not have any sex predilection.They have a peak incidence in the third decade of life, although our patient belonged to a younger age group.
On CT, chondromas are well circumscribed, extra-axial lesions that can be iso- or hypodense to brain. Low attenuation areas may be present, correlating with cystic degeneration. Irregular tumor calcification is seen in up to 60% of cases.8 Erosion and destruction of the surrounding bone can be caused by local tumor growth and is present in more than 50% of cases.9 It may also produce hyperostosis of the inner table. Following contrast administration, variable, usually patchy contrast enhancement is noted. Lack of peritumoral edema indicates years of slow growth. On MRI, the signal intensities are nonspecific and mixed on both T1- and T2-weighted images.
The closest differential diagnosis on imaging for a convexity or falx chondroma is meningioma. Considering the rarity of the entity,reaching a preoperative diagnosis based on imaging alone is not possible. However, intense homogenous contrast enhancement in meningiomas and tumoral calcification in chondromas may give a clue to the diagnosis. Some authors have mentioned delayed postcontrast enhancement to be a feature of chondromas.8
On microscopy, chondromas display mature hyaline cartilage arranged in lobules. The mature chondrocytes are situated in a chondroid matrix.Postcontrast peripheral enhancement often corresponds to fibrovascular tissue covering the nonenhancing hyaline cartilage.7 Two rare cases of falcine tumors have been reported, in which the lesions contained both hyaline cartilage and bone, and were so termed as osteochondromas.10
Total surgical resection is usually possible and curative, as the tumors tend not to invade or destroy the surrounding parenchyma. In convexity chondroma, removing the dural attachment along with the tumor is recommended. The prognosis is good with no recurrence reported on long-term follow up.
CONCLUSION
This case emphasizes the clinical features, imaging findings, differential diagnosis, pathological features and management of chondroma, a seldom-encountered pathology.
REFERENCES
- Berkman Y, Blatt E. Cranial and intracranial cartilaginous tumors. Clin Radiol. 1968;19:327-333.
- Kretzschmar H, Egger H, Beck U. Intracranial chondroma. Case report. Surg Neurol. 1989; 32:121-125.
- Valdueza JM, Freckmann N, Herrmann HD. Chondromatosis of the choroids plexus: Case report. Neurosurgery. 1990; 27(2):291-294.
- Lacerte D, Gagne F, Copty M. Intracranial chondromas. Report of two cases and review of literature. Can J Neurol Sci. 1996;23:132-137.
- Traflet R, Barbaria A, Barolt G, et al. Intracranial chondroma in a patient with Ollier’s disease: Case report. J Neurosurg. 1989;70:276.
- De Coene Back, Gillard C, Grandin C, et al. Unusual location of an intracranial chondroma. AJNR. Mar 1997; 18:573-575.
- Brownlee R, Sevick R, Rewcastle N, et al. Radiologic-pathologic correlation. Intracranial chondroma. AJNR. May 1997; 18:889-893.
- Tanohata K, Maehara Temporal, Aida N, et al. Computed tomography of intracranial chondroma with emphasis on delayed contrast enhancement. J Comput Assist Tomogr. 1987;11:820-823.
- Palacios E. Intracranial solitary chondroma of dural origin. Am J Roentgenol.1970;110:67-70.
- Alpers B. Cerebral osteochondroma of dural origin. Ann Surg.1935;101:27-37.
Citation
Radiological Case: Dural chondroma. Appl Radiol.
October 9, 2014