Radiological Case: Abernethy malformation
Images


CASE SUMMARY
A 60-year-old man was found by his primary care physician to have mildly elevated liver function tests (ALT 46, AST 49) during a routine health screening. He had no other reported medical conditions and was asymptomatic. A CT scan was performed to determine possible etiologies of elevated liver function tests.
IMAGING FINDINGS
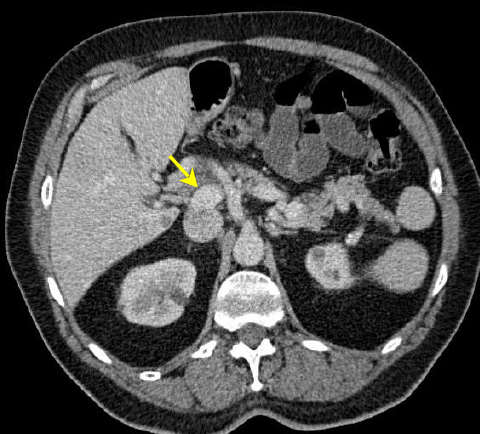
The CT scan revealed anomalous venous anatomy with absence of the intrahepatic portal vein with end-to-side communication of the extrahepatic, hypoplastic portal vein to the inferior vena cava (Figures 1 and 2). Additional imaging findings included a cystic mass at the uncinate process of the pancreas, nodular appearance of the liver and indeterminate hepatic lesions (not shown).
DIAGNOSIS
Abernethy malformation (Type 1b congenital extrahepatic portosystemic shunt)
DISCUSSION
The Abernethy malformation comprises a rare vascular malformation with resultant congenital extrahepatic portosystemic shunt (CEPS). The first known case was described by John Abernethy in 1793, where he described a postmortem evaluation of a 10-month-old girl that, among other congential anomalies, revealed the portal vein to be terminating in the inferior vena cava.1 The eponym referring to congenital extrahepatic portosystemic shunts was suggested by Howard and Davenport in 1997 in recognition of Abernethy.2
Congenital extrahepatic portosystemic shunts are characterized by portomesenteric blood draining directly to a systemic vein, bypassing hepatic flow either completely or partially.3 In 1994, Morgan and Superina proposed a classification system for CEPS according to the presence or absence of hepatic parenchymal perfusion with mesenteric venous blood.4 In Type 1, there are no intrahepatic portal branches and all portal blood is diverted into the systemic circulation by end-to-side shunt. This is sub-classified into type 1a, where splenic and superior mesenteric veins have separate drainage to the systemic venous system (congenital absence of the portal vein) and 1b, where they drain together after forming a common trunk. The intrahepatic portal vein is intact in type 2 malformations, but there is a portosystemic shunt via an end-to-side communication.3-6 Type 2a shunts are congenital whereas type 2b shunts are acquired.4 Shunts most commonly drain to the inferior vena cava, but drainage can be to the renal veins, iliac veins, azygous vein or the right atrium.6
Embyrologic development of the inferior vena cava and portal venous system occurs during the 4th-10th weeks of embryologic life. Pathogenesis of type 1 CEPS is thought to be a result of excessive involution of the periduodenal vitelline venous loop or failure of vitelline veins to form appropriate anastomoses. Type 2 CEPS may be caused by persistent subcardiohepatic anastomoses or persistence of the right vitelline vein.2,3,5
Classification of CEPS is important, as subtypes have varying clinical manifestations and treatment options. Type 1 malformations have a female predominance and are often associated with other congenital malformations, including cardiac anomalies, as in the case described by Abernethy.1,3,5,6 Others include biliary atresia, polysplenia, skeletal anomalies and renal tract anomalies.3,5,6 Apart from renal tract anomalies, associated congenital abnormalities are typically more common in Type 1 CEPS.3,5 Nodular liver lesions are also seen, including regenerative nodular hyperplasia, focal nodular hyperplasia and hepatocellular adenoma, which are benign, but hepatoblastoma and hepatocellular carcinoma has also been reported.3,5,6
Abernethy malformation often, as in the presented case, is detected incidentally while investigating cardiac anomalies or liver dysfunction.6 Sometimes the shunts are detected as a result of encephalopathy or hyperammonemia.5,6 Once the diagnosis is suggested, noninvasive imaging studies, including ultrasound, CT and MR, can be used to better characterize and classify the type of CEPS and also assess for known associated abnormalities. These methods can also help to exclude acquired portosystemic shunts or portal vein thrombosis as a cause for the imaging findings.3 Diagnosis could also include interventional radiologic procedures including conventional angiography and liver biopsy.3
CONCLUSION
The Abernethy malformation congenital extrahepatic portosystemic shunt (CEPS) is a rare entity that most often presents in the pediatric population but may go unidentified until adulthood, as in this case. The malformation is further classified on the presence or absence mesenteric blood flow to the hepatic parenchyma.4 The distinction is important for additional evaluation and management options. Type 1 malformations have a strong female preponderance and are often associated with other congenital disorders. Patients suspected of Type 1 malformation typically require liver biopsy to confirm the absence of intrahepatic portal vein branches and may require liver transplant.3,5 Coil embolization or surgical ligation of the shunt may be options for type 2 malformation.2,3 Radiologists can evaluate CEPS with noninvasive imaging modalities, including ultrasound, CT and MRI. These methods also assist in assessing associated anomalies. However, conventional angiography is considered the standard reference for depicting the portomesenteric vasculature,3 and may be needed for diagnosis.
REFERENCES:
- Abernethy J. Account of two instances of uncommon formation in the viscera of the human body. Philos Trans R Soc Lond. 1793;17:292-299.
- Howard ER, Davenport M. Congenital extrahepatic portocaval shunts—The Abernethy malformation. J Pediatr Surg. 1997;32(3):494-497.
- Alonso-Gamarra E, Parron M, Perez et al. Clinical and radiologic manifestations of congenital extrahepatic portosystemic shunts: A comprehensive review. Radiographics. 2011;31:707-722.
- Morgan, GM, Superina R. Congenital absence of the portal vein: Two cases and a proposed classification system for portasystemic vascular anomalies. J Pediatr Surg. 1994 Sep;29(9):1239-41.
- Gangadhar K, Nair SV, Sunnapwar A, Chintapalli KN. Abernethy malformation and the spectrum of imaging findings: A case report. NJR. 2013;2:97-102.
- Murray CP, Yoo S, Babyn P. Congenital extrahepatic portosystemic shunts. Pediatr Radiol. 2003;33:614-620.
Citation
KL T, TA R, M A.Radiological Case: Abernethy malformation . Appl Radiol. 2015; (12):26-27.
December 17, 2015