Postpartum Retroperitoneal Hemorrhage Secondary to Ovarian Artery Pseudoaneurysm
Images


Case Summary
A G8P4 patient with sickle cell trait presented to the emergency department with diffuse, cramping abdominal pain ten days after an uncomplicated vaginal delivery. The patient also reported worsening shortness of breath and two syncopal episodes since the delivery. They had light vaginal bleeding and malodorous discharge for one day. Initial vital signs demonstrated tachycardia and tachypnea.
They were normotensive, afebrile, and saturating well on room air. Physical examination demonstrated mild abdominal distension with tenderness to palpation of the left upper quadrant with guarding. Speculum examination revealed a moderate amount of blood in the vaginal vault without abnormal discharge. There was no vulvar hematoma evident.
Imaging Findings
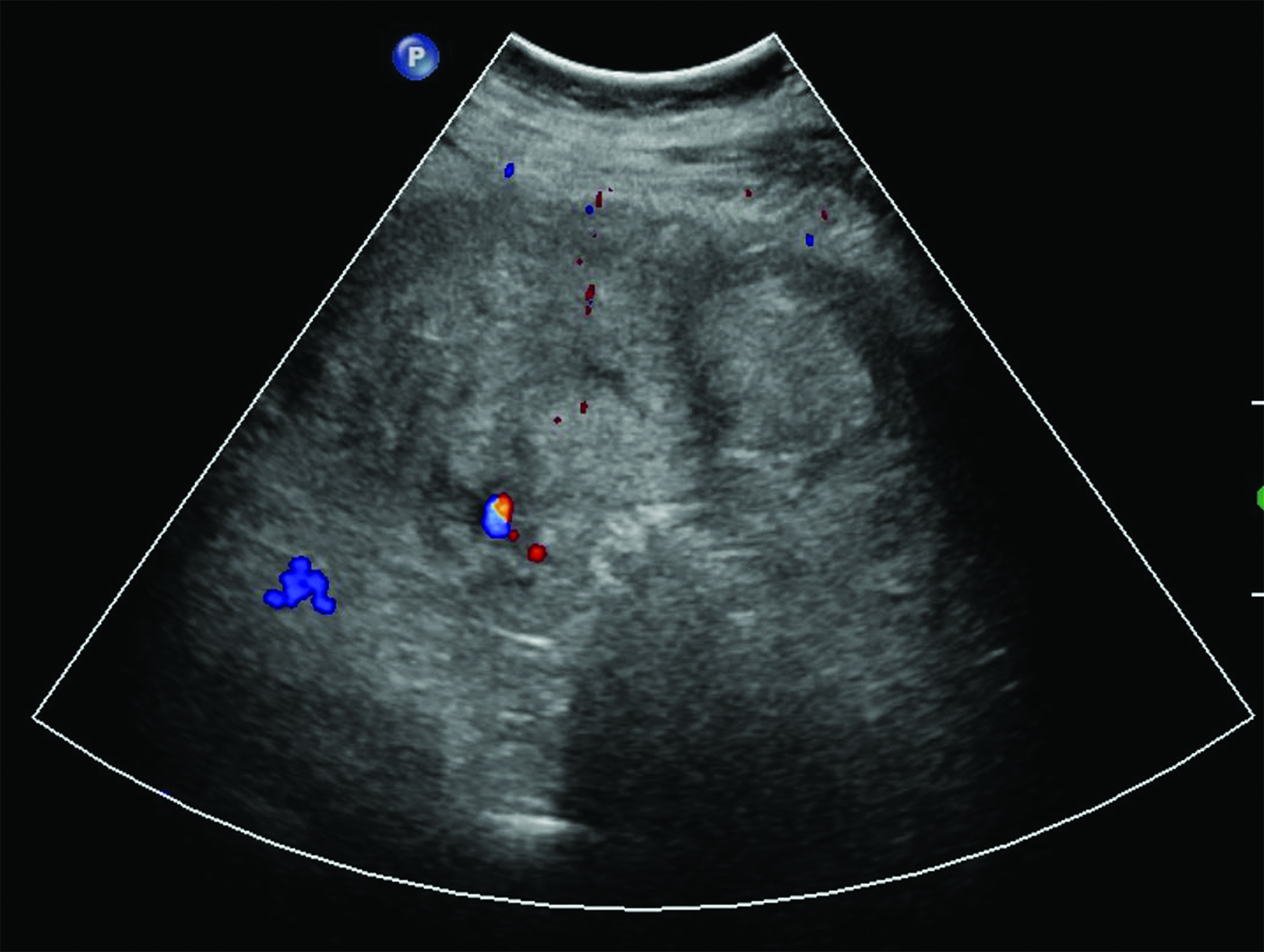
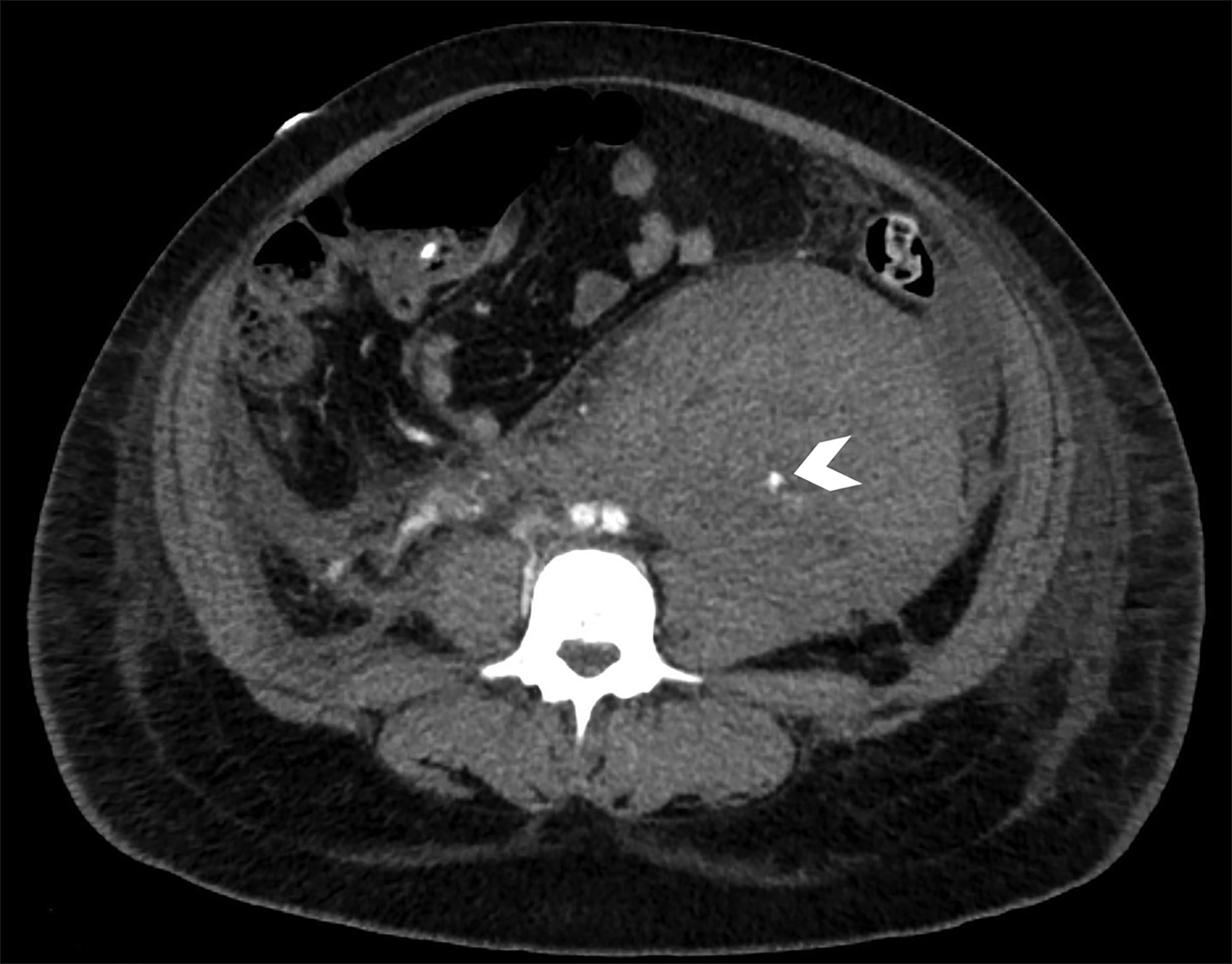
Transabdominal ultrasound (Figure 1) demonstrated a heterogeneous collection extending from the inferior aspect of the left kidney to the left adnexa. CT angiography of the abdomen and pelvis (Figure 2) demonstrated a mixed-attenuation collection in the left retro-peritoneal space extending inferiorly into the pelvis, surrounding the left ovarian vessels. The tortuous left ovarian artery was faintly visualized coursing through the hematoma with a small outpouching of contrast at the mid-segment.
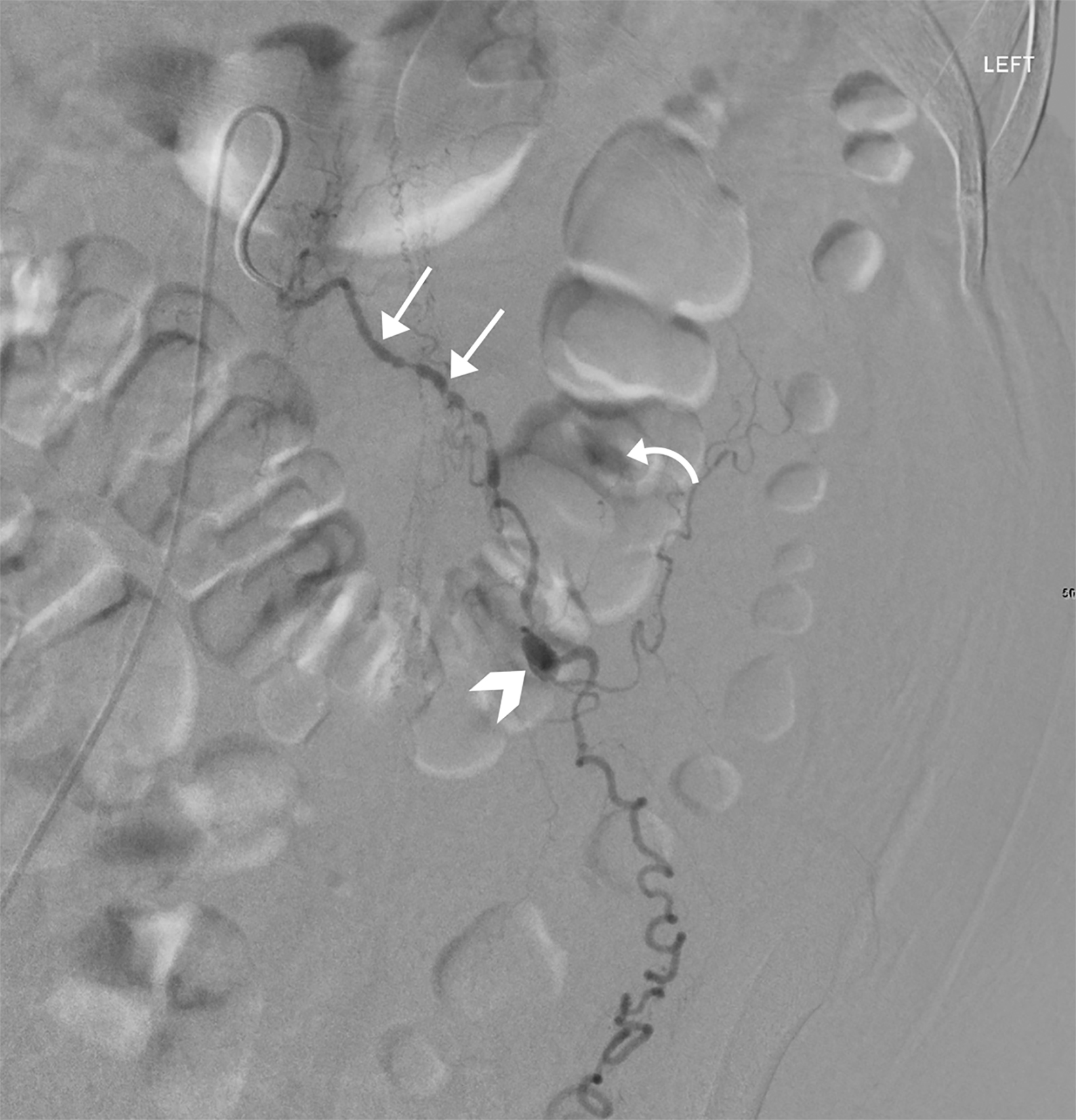
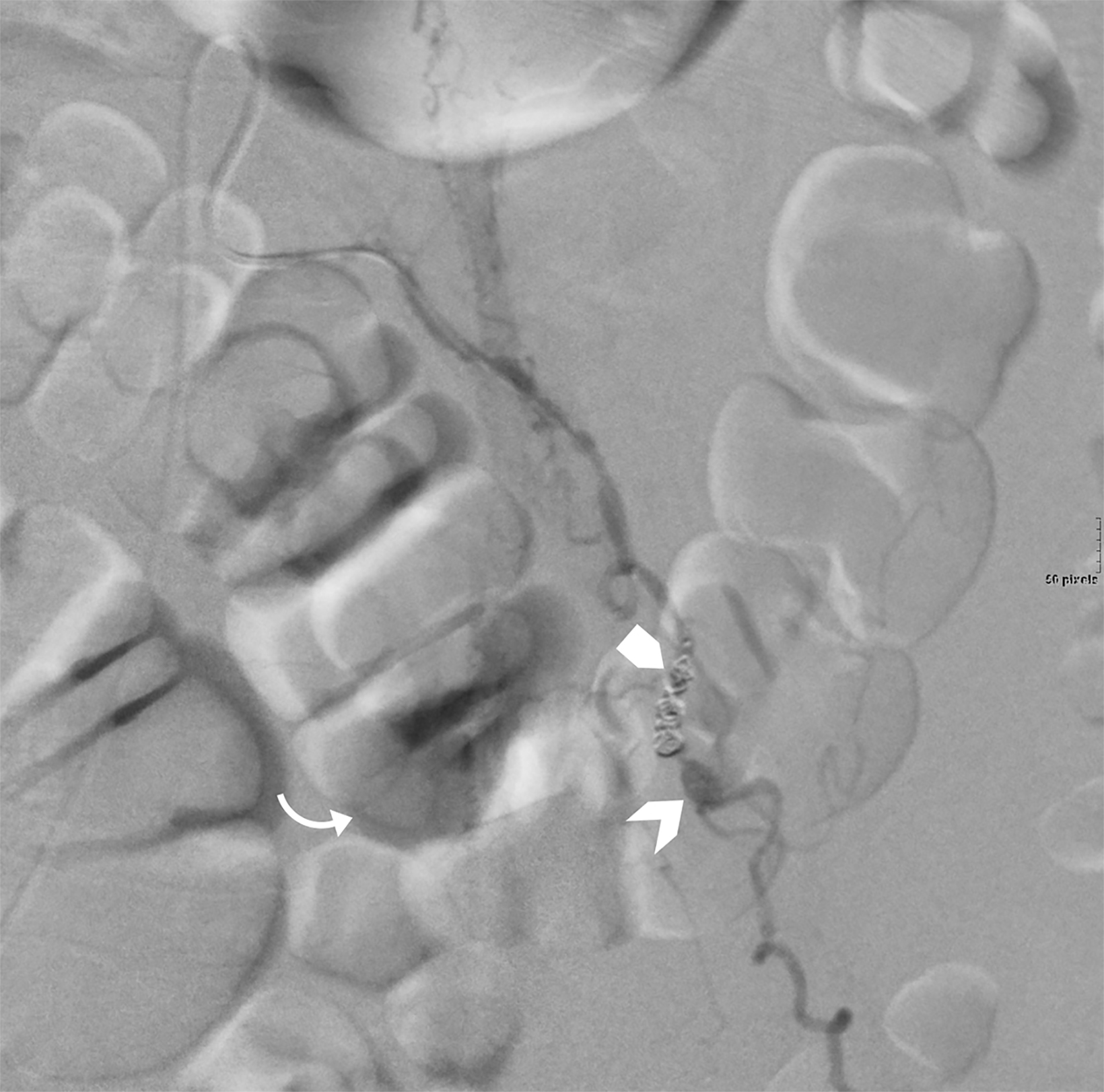
Catheter angiography (Figure 3) demonstrated multiple stenoses with a beaded appearance of the proximal left ovarian artery. Within the mid-segment, there was a 1 cm focal outpouching with active extravasation. The artery and pseudoaneurysm were successfully embolized.
Diagnosis
Postpartum retroperitoneal hemorrhage secondary to ovarian artery pseudoaneurysm.
Discussion
Retroperitoneal postpartum hemorrhage is a rare complication of childbirth that most commonly occurs following assisted delivery or Caesarean section.1 Anticoagulation therapy, prolonged labor, and manual placental removal have also been associated with the development of postpartum retroperitoneal hemorrhage.2 The incidence of puerperal hematoma formation is approximately between 1 in 309 and 1 in 1500 deliveries.1
Although there is little published information regarding retroperitoneal hemorrhage in the pregnant and postpartum population, data suggest a correlation between parity and ovarian artery aneurysm and pseudoaneurysm formation.2 Twenty-five cases of spontaneous ovarian artery aneurysm (OAA) rupture have been reported in the literature, of which 72% were associated with pregnancy.3,4 Pregnant patients were all multigravida, suggesting that multiparity is a risk factor.5,6 No ruptured OAA have been reported in iparous patients, reinforcing the correlation between OAA formation and pregnancy, leading to an increased risk of retroperitoneal hemorrhage.5
However, the mechanism of OAA formation is not well understood. Hemodynamic changes known to be related to pregnancy include increased cardiac output and blood volume as well as systemic hypertension. Additionally, as the uterus expands, dilatation of the pelvic arteries directly increases uterine blood flow.3 During normal uterine involution in the postpartum period, one or multiple segments of the ovarian artery may not involute; it is thought to be by this mechanism that the artery may become more susceptible to aneurysm formation in subsequent pregnancies.3
Hormonal alterations during pregnancy are also responsible for microscopic vascular wall changes, including intimal hyperplasia, smooth muscle hyperplasia of the media, fragmentation of reticular fibers, and loss of the normal corrugation of elastic fibers, rendering the wall of the ovarian artery susceptible to aneurysm formation.3 Repeated pregnancies bring about further hemo- dynamic and endocrine changes which can exacerbate or rupture a pre-existing aneurysm. Another possible risk factor for OAA rupture is hypertension, found in four of nine ruptured OAA patients in one report.7
Patients with retroperitoneal hemorrhage from OAA rupture may present with severe or worsening flank pain, hemodynamic instability, syncope, and anemia.8 Continuously declining hemoglobin in a postpartum patient should raise suspicion for occult hematoma formation in the absence of vaginal bleeding. Patients may also present with nausea, vomiting, malaise, and vague truncal pain.8,9
Retroperitoneal hematomas appear on ultrasound as heterogeneous structures along the pararenal space extending into the pelvis.9 Triple-phase CT angiography can often determine the etiology of the hemorrhage.9 CT angiography will show a heterogeneous retroperitoneal fluid collection with higher than simple fluid attenuation. Active hemorrhage appears as evolving high-density material within the collection on arterial and venous phase images. Pseudoaneurysms may be identified on CT angiography by their characteristic outpouching along the course of an artery that does not evolve on delayed images. Catheter angiography remains the gold standard for diagnosing and treating the cause of retroperitoneal hematomas with an identifiable etiology.9
Treatment options consist of conservative management, endovascular intervention, and surgical evacuation and vascular repair.9 Conservative management is typically pursued in hemodynamically stable patients without significantly decreasing serum hemoglobin.9 Transarterial embolization is typically performed in patients with continuously decreasing serum hemoglobin, with or without hemodynamic instability, where the etiology of hemorrhage is identified on cross-sectional imaging.3,4 Catheter angiography may be pursued in unstable patients with active hemorrhage without an identified etiology.3,4 Surgical evacuation is reserved for hemodynamically unstable patients in whom endovascular intervention is unsuccessful or the cause of hemorrhage cannot be identified.8
Conclusion
Nontraumatic obstetric retroperitoneal hematomas are an exceedingly rare complication of spontaneous vaginal delivery, with literature demonstrating a correlation between parity and ovarian artery aneurysms. Diagnostic and interventional radiologists should be aware of this complication and its associations to achieve timely diagnosis and management. Ovarian artery pseudoaneuryms, similar to pseudoaneurysms of other visceral arteries, may be treated with embolization.
References
Citation
CC Z, KM Z, TF T, H W, SM S.Postpartum Retroperitoneal Hemorrhage Secondary to Ovarian Artery Pseudoaneurysm. Appl Radiol. 2023; (6):49-51.
November 3, 2023