PerformanceBridge: Improving Operational Efficiency
Images
Supplement to November-December 2019 Applied Radiology. Sponsored by Philips Healthcare.
The radiology department at Boston Medical Center (BMC) supports the largest Level 1 trauma center in New England. To maximize the department’s effectiveness in supporting the facility, the radiology team at BMC uses Philips’ PerformanceBridge Practice to monitor operational data and identify opportunities to make impactful workflow changes. The team recently implemented changes to the clinical workflow in computed tomography (CT) for emergency department (ED) patients, resulting in a significant improvement in CT turnaround time (TAT).
Stephan Anderson, MD, a clinical radiologist at BMC, will present his research findings at the 2019 Annual Meeting of the Radiological Society of North America (RSNA) in Chicago, IL. As one of the industry’s more progressive groups utilizing data-driven practice management, BMC has been utilizing practice data to identify opportunities for improvement in such areas as patient flow, task scheduling, and TAT. Through PerformanceBridge, the team has the flexibility to manipulate practice data to get customized dashboards and can pull in other information as needed. The availability of this data to make improvements is what inspired the work they’re sharing with their peers at RSNA.
Workflow changes for efficiency
Dr. Anderson, also the Vice Chairman for radiology research at BMC, specifically targeted the emergency department CT workflow as an opportunity to improve TAT. In the ED, Dr. Anderson noted, there’s always pressure to reduce TAT and get patients to the next stage of care.
The researchers evaluated TAT using the time that elapsed between a CT scan order and its interpretation. Typically, at BMC, the details of a CT ordered by an ED physician must be documented, or protocoled, by a radiologist or resident. This protocol includes directions for the technologist on performing the exam, such as whether to use intravenous or oral contrast, or other variables based on the reason for the exam. Oftentimes, the technologist must call the radiology workroom to ask for an exam to be protocolled so the study can be performed.
Dr. Anderson’s goal was to shorten the TAT for emergency CT exams. Toward that end, he worked with his team and the team at Philips to identify the six CT exams most commonly ordered in the ED, including CT pulmonary angiograms for patients presenting with shortness of breath.
“The whole process of having the technologist call radiology and ask for someone to go to the ordering system to input the protocol took a lot of time and also interrupted the radiologists who were reading scans,” Dr. Anderson explains. “We’re always very mindful of throughput time in the ED, so trying to eliminate any drag on that system is always a priority. The change that we implemented was to remove the need for a physician to protocol. This was possible because many of the CT examinations for the ED are the same.”
A common set of terms, or indications, was created for each of the six CT exams included in the study. A few select indications were identified that technologists would be allowed to protocol themselves, without relying on a radiologist.
“The human piece of the research relied on the technologists. They needed to look at the indications the ED gave them and see if they matched the list of terms we created. If they matched, the technologists could protocol the exams directly,” Dr. Anderson says.
Efficiency improvements
The study started as a four-month pilot program (Oct. 2018-Feb. 2019) — which has continued and was then expanded this past summer — and used PerformanceBridge Practice to evaluate how the changes affected CT turnaround time.
“The way we use PerformanceBridge is to analyze the impact of that change on our workflow,” explains Dr. Anderson. “We can pull out all the data around a patient’s flow through the ED and very quickly calculate everything we need to see as a function of the examination. We can look at abdominal scans, for instance, at each step of the process, and analyze the data before and after we made this protocol change. We can very easily draw out that there was a huge impact on throughput time.”
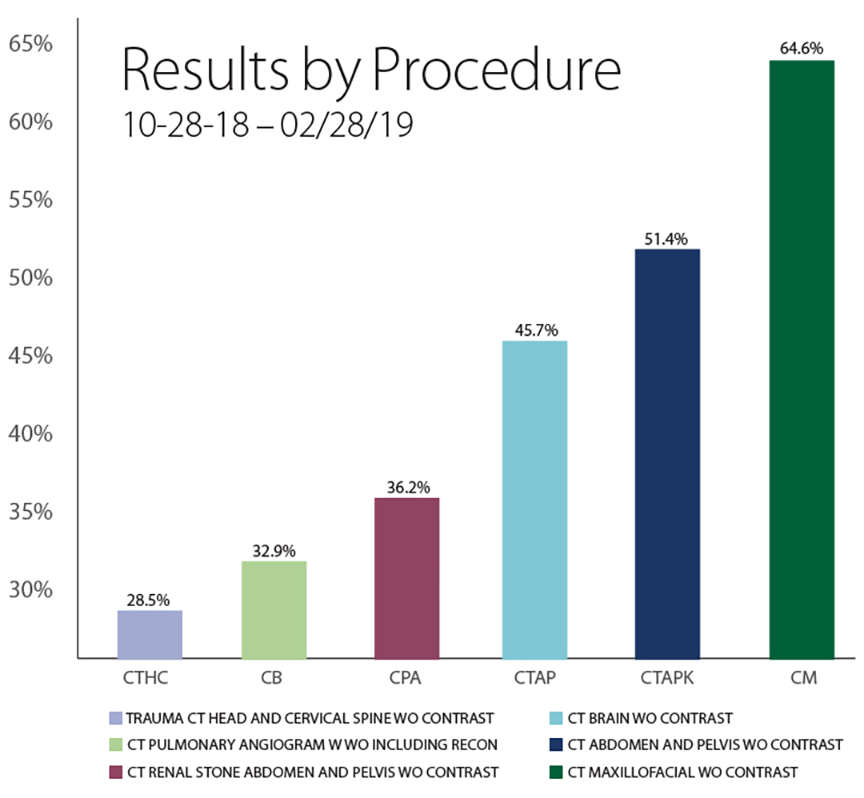
According to Dr. Anderson, the lowest degree of TAT improvement documented was 29 percent, and the highest was 65 percent.
“One example,” notes Dr. Anderson, “is an oral maxillofacial CT. The TAT went from 65 minutes to 28 minutes. That’s a significant reduction in time, not only from the perspective of the ED, but also for that patient.”
The lowest TAT impact was seen in CT for head and cervical spine trauma, Dr. Anderson says, noting that TAT fell 11 minutes, from 54 to 43 minutes.
“This research is very meaningful because it took only a trivial change to our workflow and no additional effort was needed from anyone,” he explains, adding that without PerformanceBridge, “the project would be much more difficult to complete and require an enormous amount of human effort to get [the] data. We wouldn’t be able to make these kinds of changes quickly and analyze their impacts. From a quality improvement perspective, PerformanceBridge makes analyzing improvement efforts really quite easy.”
Based on the study’s success and positive feedback from the ED, Dr. Anderson plans to move the project beyond the ED to outpatient imaging, where the goal would be less about reducing TAT and more about improving workflows because protocoling could be completed days ahead of patient arrival.
Operational improvements
Completing protocols for outpatient imaging is an overall good use of staff time, except when patients fail to show up for exams. According to Carlos Arellano, Senior Administrative Director of Radiology and Otolaryngology, no-shows in nuclear medicine, for example, are particularly expensive. Arellano is using PerformanceBridge to monitor daily department operations and identify areas where improvements can be made, including finding ways to predict no-shows and keep patients moving through their care journey.
“Each member of my team has their own PerformanceBridge dashboard that they have designed for their particular modality,” explains Arellano, “including information they want to display day to day, and what information they find particularly useful for their department. A year ago, we were using PerformanceBridge for isolated projects, but now it’s much more of a global tool used to manage the entire department.”
Arellano is using PerformanceBridge Practice to follow an initiative targeting inclusion of no-show data through BMC’s patient navigation system. In breast cancer screening, for example, BMC is leveraging PerformanceBridge Practice to track patient screening and follow-up appointments.
“We use the PerformanceBridge to run all the analysis and track which patients we need to be reaching out to schedule for the screening, reschedule patients who missed their appointments, and track all of the findings,” Arellano explains. “Or if a patient has a lesion and needs to come back for an ultrasound, there needs to be a way to keep track of everything in one system, so a flag can be generated and someone can be alerted that a patient’s care path has been interrupted. We don’t want any patient to fall through the cracks.”
Administrative feedback tool
The BMC team is currently realizing clear efficiency gains by using PerformanceBridge. In the future, Arellano wants to leverage the solution’s analysis capabilities even more to continue driving change at BMC. Arellano would like to create an individual PerformanceBridge dashboard for each radiologist and a feedback tool for technologists.
“In the coming year, I want to see us developing individual dashboards for our radiologists so they can understand the types and volume of cases they’re reading. I also want to implement the feedback tool, currently available in the PerformanceBridge Connect application, to improve communication between our radiologists and technologists. The application allows radiologists to communicate quality issues in the images as well as provide positive feedback when technologists are creating high-quality exams,” he says.
Knowledge sharing
“I know the challenges we’re facing aren’t unique to BMC,” Arellano says. “The wonderfully unique thing about our industry is that we can share our expertise and experiences with other facilities without threat of losing competitive advantage. We’re sharing our experiences to highlight the areas in which we’ve excelled, what we’re still working on, and how we’ve prioritized projects, we do not have the bandwidth to work on all issues at once. The more we all share, the better we can all become as healthcare providers.”
Arellano’s team is excited about sharing their recent successes at the 2019 RSNA annual meeting and how PerformanceBridge is being used to identify where changes could be made to improve important metrics like patient wait times — one of the most common pain points in nearly every healthcare facility.
“There is a great deal of data available to us that can help us address various issues. It’s just a matter of organizing, prioritizing and building different views, so we have the right information in the right hands at the right time — that’s where Philips and PerformanceBridge are really helping us.”
Citation
PerformanceBridge: Improving Operational Efficiency . Appl Radiol.
November 13, 2019