Pediatric abdominal and pelvic imaging in non-accidental trauma
Images











Historically, the emphasis of imaging in non-accidental trauma (NAT) has been geared towards assessment of intracranial and musculoskeletal injuries, as abdominal and pelvic injuries were considered to be less common.1 There has been an increase in hospitalization of children with abdominal and pelvic injuries secondary to NAT, as these are often severe and may need surgical intervention.2 Recent study has shown that more than 25% of all hospitalizations for abdominal and pelvic trauma in children younger than 1 year of age and 40% of all hospitalizations in children younger than 4 years of age are secondary to NAT.3 Roaten et al found that children with abdominal and pelvic injuries due to NAT were more likely to undergo emergent operations (46% versus 5%) than those without NAT.4 The overall mortality for NAT was 9.7% compared to 2.2% for accidental trauma.3, 5 There is no consensus regarding specificity of the abdominal and pelvic imaging findings in inflicted injury versus accidental trauma. Multiple studies which compared inflicted and accidental abdominal injuries in young children, found an increased rate of pancreatic and bowel injuries in NAT.6, 7 A recent study evaluating abdominal injuries in abused pre-school age children found that abdominal injuries present in a similar pattern to that of children with accidental trauma.8 Regardless of etiology, it is imperative for radiologists to make a timely diagnosis.
Imaging techniques and recommendations
Imaging evaluation is usually directed by the patient’s clinical presentation, which may include abdominal wall bruising, abdominal pain, distention, vomiting, bloody stools and hypoactive or absent bowel sounds. As with accidental injuries, the major priority is patient stabilization and resuscitation. Abnormal laboratory values such as elevated liver enzymes (AST, ALT) and amylase can be used as guiding tools for abdominal imaging utilizing CT of the abdomen and pelvis.9 A timely clinical diagnosis cannot always be made, as the physical signs may be absent and the symptoms are nonspecific, particularly with minor injuries. It is important to note that abdominal wall bruising is not a reliable predictor for underlying abdominal injury, as it was noted to be absent in up to 80% of children with abdominal injuries in a recent review.10, 11 According to the American College of Radiology (ACR) imaging appropriateness criteria, CT of the abdomen and pelvis with intravenous contrast should be obtained if there is suspicion of abdominal injury.12 There is no utility in performing an unenhanced CT in addition to enhanced CT. Although oral contrast may improve evaluation in some cases, such as suspected duodenal hematoma, it is not routinely utilized due to potential delay acquiring the study and surgical management, if required.13
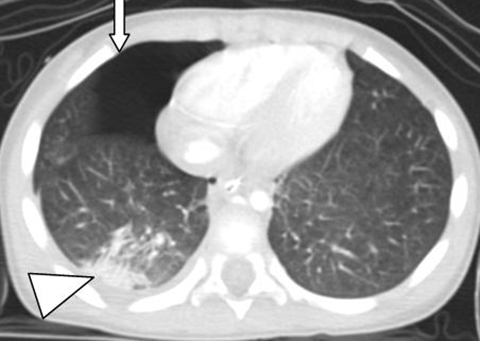
CT permits accurate detection and quantification of organ injury, and can help in prioritizing optimal management by diagnosing life threatening injuries and active hemorrhage. Images are obtained in late arterial or parenchymal phase to best identify solid organ injury. Excretory phase imaging should be performed in cases of genitourinary tract injury. These phases are required to be able to accurately grade solid organ injuries as per the American Association for the Surgery of Trauma (AAST) Organ Injury Scale guidelines.14. Additionally, osseous injuries to the imaged ribs, spine and pelvis can be seen, which may aid in diagnosis. The current generation of multi-detector CT (MDCT) scanners provides high image quality with decreased radiation dose when used in pediatric settings.
Ultrasound (US), although less sensitive than CT, can be useful in urgent screening, as it can be rapidly performed at the bedside in a hemodynamically unstable patient.2 It can also be used as a follow-up study to ensure resolution or in children with low suspicion of injury.1 Studies have shown that US can detect fluid collection, solid organ injury and other direct or indirect evidence for bowel or mesenteric injuries.15, 16 Although whole body imaging in children is feasible with MRI, this is not utilized routinely in the acute setting as younger patients may require sedation or anesthesia. MRI is useful as a problem-solving tool.
Hepatic and splenic injury
The liver is the most commonly injured solid organ in abusive injury.2 Prior studies have found that elevated liver enzymes, aspartate and alanine transaminases (AST, ALT) can be used as predictors for underlying liver injury and positive findings on CT scans.3 Although some studies have shown lack of specificity with these laboratory markers, these are recommended in children under 5 years of age with suspected NAT, but lacking overt physical exam findings.2, 8 While the posterior segment of the right lobe is the most common location for hepatic injuries, as it is relatively fixed compared to the rest of the liver by the coronary ligaments, the left lobe of the liver is more prone to injury in NAT, likely secondary to direct central blows.17, 18 On US, the contusions appear as echogenic hypovascularized areas in the acute phase which subsequently become hypoechoic or sometimes cystic in subacute to chronic phases.1
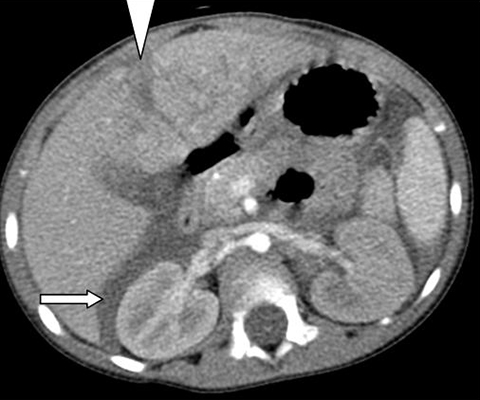
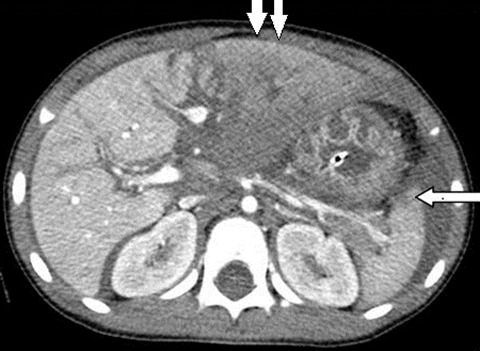
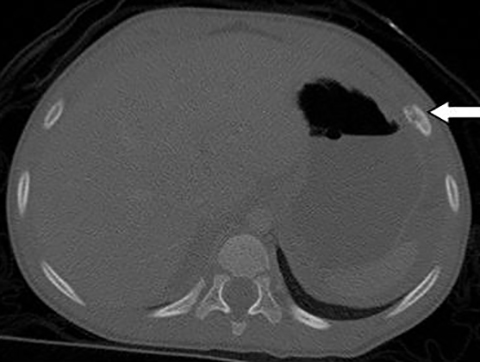
On CT, simple lacerations appear as hypoenhancing linear areas (Figure 1), whereas the complex or stellate lacerations have a branching pattern (Figures 2, 3). The hepatic lacerations may be associated with parenchymal or subcapsular hematoma (Figures 2, 4). If the injury extends to the surface of the liver or if the hepatic capsule is disrupted, there may be an associated hemoperitoneum. Periportal low attenuation, from dilated lymphatics, is a nonspecific finding that can occasionally be seen from injury (bleeding along portal triads) or more likely from elevated IVC pressure producing lymphatic distension.19 Most hepatic injuries in children can be managed nonoperatively regardless of severity. In prior studies, authors found that approximately 1-3% children with hepatic injury required surgical hemostasis.20
Splenic injuries are less common than liver injuries in NAT as opposed to accidental trauma, although there have been some reported cases.6. Imaging appearances of splenic injuries including lacerations and contusions are similar to liver injuries. Splenic lacerations can be linear or branching in appearance and are hypodense areas compared to the normally enhancing parenchyma (Figures 3, 5). There may be associated parenchymal or subcapsular hematoma, which appears as an area of hypoenhancement. In contrast to perisplenic fluid, subcapsular hematoma will indent the splenic parenchyma.2 Management is mostly conservative as hematomas and lacerations tend to gradually decrease in size.4
Urogenital injuries
Isolated urinary tract injury is less frequent with abusive injuries.3, 7 The incidence of renal injuries in abusive abdominal trauma varies from 19-25%, more frequently seen in the setting of multiple injuries.7, 9 Similar to other solid organ injuries, these are classified into hematomas, contusions, lacerations or vascular injuries and have similar imaging appearances which are graded as per the AAST organ injury scale.14 Treatment of renal injuries is largely nonoperative.21
Adrenal hemorrhage has been described in abusive injuries and more commonly affects the right side and is seen in association with other injuries.22 Imaging appearances vary depending on the stage of hemorrhage. Management is conservative.
Genital injuries may occur following physical or sexual abuse and are usually diagnosed clinically.23 Scrotal hematoma can be seen from direct trauma or extravasation of blood from intra-abdominal bleeding (Figure 6).
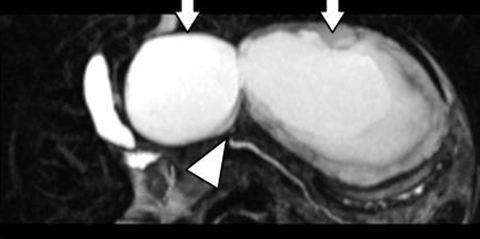
Pancreatic injury
The pancreas may be injured secondary to blunt trauma to the upper abdomen, accounting for 8-17% of abusive abdominal injuries.6, 24 Pancreatitis may develop with disruption of acinar and ductal integrity, with seepage of enzymes into tissue planes, and activation of enzymes. In severe cases, there may be pancreatic laceration or transection resulting from compression of the pancreas against the spine.25 In younger children (average age 27 months) presenting with pancreatitis, there should be a high suspicion for NAT.6, 26 Contrast-enhanced CT (CECT) is the modality of choice for imaging pancreatic injuries.27 Imaging findings include direct signs such as pancreatic laceration or transection (more than 50% of gland involved) and indirect signs such as pancreatic gland enlargement and ill-defined areas of contusion. Laceration, transection and contusion appear as linear or ill-defined areas of hypoenhancement respectively (Figure 7). Fluid in the lesser sac is the most common finding of traumatic pancreatic injury in children on CECT scan.27 Pancreatic pseudocysts in children are frequently seen in the post-traumatic setting. Magnetic resonance cholangiopancreatography is a useful adjunct to CT in delineating the biliary and ductal anatomy in addition to the parenchymal findings (Figure 8). Although US may depict the findings of pancreatic injury, such as gland enlargement, peripancreatic fluid and altered echogenicity, it is not preferred for initial diagnosis. Follow-up screening for development of post-traumatic pseudocyst and image-guided aspiration can be easily performed with US.27 The management of pancreatic trauma is mostly non-operative, with the exception of distal duct injuries, which may require prompt spleen-sparing distal pancreatectomy.29
Hollow-organ injury
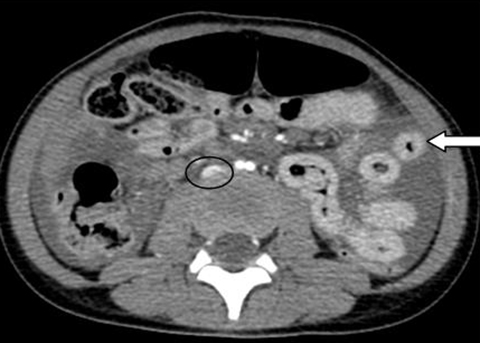
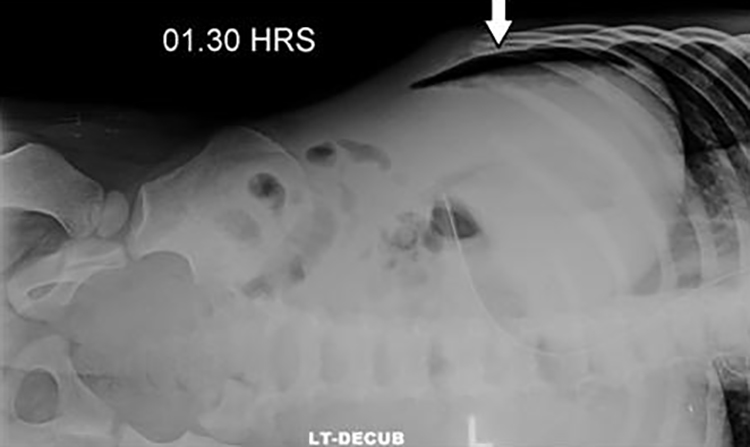
Hollow-organ injuries are disproportionately more commonly seen with inflicted injury as compared to accidental trauma.10, 24. The duodenum is the most commonly involved hollow organ in children with abusive injuries. In a child under 5 years of age, the presence of non-motor vehicle related duodenal trauma raises concern for NAT.10 Intestinal injuries include intramural hematoma and, less commonly, perforation. The radiologic distinction between the two is paramount, as management varies. While duodenal hematomas are mostly managed conservatively, the presence of perforation is a surgical emergency.30. The mechanism of injury is compression of the small bowel against the spine or shearing forces. The duodenum being retroperitoneal in location is more susceptible to compressive injury.
CECT of the abdomen and pelvis is the modality of choice to identify bowel and mesenteric injuries.30 If there is a clinical suspicion of hollow-organ injury, water-soluble oral contrast can be given for better depiction of findings, as it can assist in differentiation of intestinal hematoma versus rupture. On CECT, presence of free intraperitoneal fluid, mesenteric focal fluid and duodenal wall thickening with or without focal mass suggest duodenal hematoma. Intraperitoneal or retroperitoneal air and enteric contrast extravasation are indicative of bowel perforation and necessitate emergent surgery (Figure 9).30
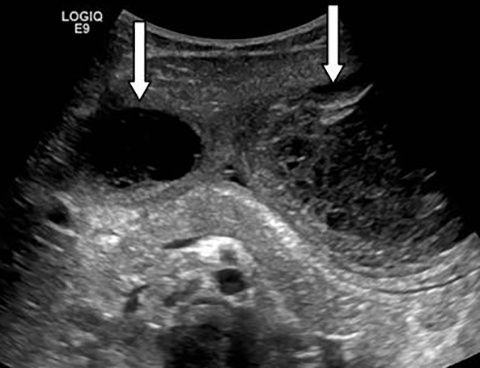
On US, the presence of a focal mass in the duodenum and free fluid in the abdomen suggest the diagnosis of duodenal hematoma.1 Although an upper GI series and ultrasound may depict the findings of duodenal hematoma, they are not as widely applied as CECT (Figure 10). There is insufficient evidence regarding utilization of ultrasound for initial diagnosis of intestinal injury. Ultrasound is more useful in follow up to document resolution of duodenal hematoma.
Hypoperfusion complex or shock bowel
Hypoperfusion complex or shock bowel is indicative of tenuous hemodynamic instability and requires aggressive resuscitation.31 The imaging findings of hypoperfusion complex on CECT include diffusely dilated fluid filled bowel loops with increased enhancement of the bowel wall and mesentery, diminished caliber and intense enhancement of the abdominal aorta and inferior vena cava, increased or less commonly absent renal enhancement, and intense enhancement of the adrenal glands (Figure 3).31 Other variable findings include decreased pancreatic and splenic enhancement, periportal low attenuation zones, peritoneal and retroperitoneal fluid, and bowel wall thickening.
It is important to recognize these findings as they require aggressive medical management.
References
- Raissaki M, Veyrac C, Blondiaux E, et al. Abdominal imaging in child abuse. Pediatr Radiol. 2011; 41(1): 4- 16.
- Sheybani EF, Gonzalez-Araiza G, Kousari YM, et al. Pediatric nonaccidental abdominal trauma: What the radiologist should know. Radiographics. 2014; 34(1): 139-153.
- Lane GW, Dubowitz H, Langenberg P. Screening for occult abdominal trauma in children with suspected physical abuse. Pediatrics. 2009; 124 (6): 1595-1602.
- Roaten JB, Partrick DA, Nydam TL, et al. Nonaccidental trauma is a major cause of morbidity and mortality among patients at a regional level I pediatric trauma center. J Pediatr Surg. 2006; 41(12): 2013-2015.
- Trokel M, DiScala C, Terrin NC, et al. Blunt abdominal injury in the young pediatric patient: child abuse and patient outcomes. Child Maltreat. 2004; 9(1): 111-117.
- Trokel M, DiScala C, Terrin NC, et al. Patient and injury characteristics in abusive abdominal injuries. Pediatr Emerg Care. 2006; 22 (10): 700-704.
- Wood J, Rubin DM, Nance ML, et al. Distinguishing inflicted versus accidental abdominal injuries in young children. J Trauma. 2005; 59 (5): 1203-1208.
- Hilmes MA, Hernandez-Schulman M, Greeley CS, et al. CT identification of abdominal injuies in abused pre-school-age children. Pediatr Radiol. 2011; 41(5): 643-651.
- Trout AT, Strouse PJ, Mohr BA, et al. Abdominal and pelvic CT in cases of suspected abuse: can clinical and laboratory findings guide its use? Pediatr Radiol. 2011; 41(1): 92-98.
- Barnes PM, Norton CM, Dunstan FD, et al. Abdominal injury due to child abuse. Lancet. 2005; 366 (9481):234-235.
- Maguire SA, Upadhyaya M, Evans A, et al. A systematic review of abusive visceral injuries in childhood –their range and recognition. Child Abuse Negl. 2013; 37 (7): 430-445.
- Slovis TL, Smith WL, Strain JD, et al. Expert panel on pediatric imaging. Suspected physical abuse-child. Reston (VA). 2005; (ACR) 5 p. 33.
- Section on Radiology; American Academy of Pediatrics. Diagnostic imaging of child abuse. Pediatrics. 2009; 123 (5): 1430 -1435.
- Tinkoff G, Esposito TJ, Reed J, et al. American Association for the Surgery of Trauma Organ Injury Scale I: spleen, liver, and kidney, validation based on the National Trauma Data Bank. J Am Coll Surg 2008; 207 (5): 646-655.
- Lorente-Ramos RM, Santiago-Hernando A, Del Valle-Sanz Y, et al. Sonographic diagnosis of intramural duodenal hematomas. J Clin Ultrasound. 1999; 27(4): 213–216.
- Rao P. Emergency imaging in non-accidental injury. In: Carty H, ed. Emergency Pediatric Radiology, 2nd ed. Berlin: SpringerVerlag; 2002: 347–380
- Stalker HP, Kaufman RA, Towbin R. Patterns of liver injury in childhood: CT analysis. AJR Am J Roentgenol. 1986; 147(6):1199–1205.
- Herr S. Abdominal and chest injuries in abused children. In: Jenny C, ed. Child abuse and neglect: diagnosis, treatment, and evidence. St. Louis, Mo: Saunders/Elsevier; 2011: 326-331.
- Sivit CJ, Taylor GA, Eichelberger MR, et al. Significance of periportal low attenuation zones following blunt trauma in children. Pediatr Radiol. 1993; 23 (5): 388-390.
- Ruess L, Sivit CJ, Eichelberger MR, et al. Blunt abdominal trauma in children: Impact of CT on operative and nonoperative management. AJR Am J Roentgenol. 1997; 169 (4):1011–1014.
- Mohamed AZ, Morsi HA, Ziada AM, et al. Management of major blunt pediatric renal trauma: single-center experience. J Pediatr Urol. 2010; 6 (3): 301-305.
- Nimkin K, Teeger S, Wallach MT, et al. Adrenal hemorrhage in abused children: imaging and postmortem findings. AJR Am J Roentgenol. 1994; 162 (3): 661-663.
- Hobbs CJ, Osman J. Genital injuries in boys and abuse. Arch Dis Child. 2007; 92 (4): 328-331.
- Roaten JB, Partrick DA, Bensard DD, et al. Visceral injuries in nonaccidental trauma: spectrum of injury and outcomes. Am J Surg. 2005; 190 (6): 827-829.
- Ziegler DW, Long JA, Philippart AI, et al. Pancreatitis in childhood: experience with 49 patients. Ann Surg. 1988; 207 (3): 257-261.
- Arkovitz MS, Johnson N, Garcia VF. Pancreatic trauma in children: mechanisms of injury. J Trauma. 1997; 42 (1): 49–53.
- Bixby SD, Callahan MJ, Taylor GA. Imaging in pediatric blunt abdominal trauma. Semin Roentgenol. 2008; 43 (1): 72-82.
- Jobst MA, Canty TG, Lynch FP. Management of pancreatic injury in pediatric blunt abdominal trauma. J Pediatr Surg. 1999; 34 (5): 818–82.
- Gaines BA, Shultz BS, Morrison K, et al. Duodenal injuries in children: beware of child abuse. J Pediatr Surg. 2004; 39 (4):600-602.
- Kunin JR, Korobkin M, Ellis JH, et al. Duodenal injuries caused by blunt abdominal trauma: value of CT in differentiating perforation from hematoma. AJR Am J Roentgenol. 1993; 160 (6): 1221-1223.
- Sivit CJ, Taylor GA, Bulas DI, et al. Posttraumatic shock in children: CT findings associated with hemodynamic instability. Radiology. 1992; 182 (3): 723- 726.
Related Articles
Citation
A M, EN F. Pediatric abdominal and pelvic imaging in non-accidental trauma. Appl Radiol. 2018;(4):16-21.
April 5, 2018