Paget-Schroetter Syndrome
Images

Case Summary
An adolescent volleyball player presented with intermittent right-arm numbness, and more than one month of worsening right upper extremity swelling.
Imaging Findings
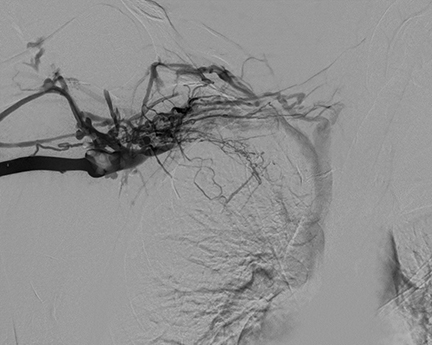
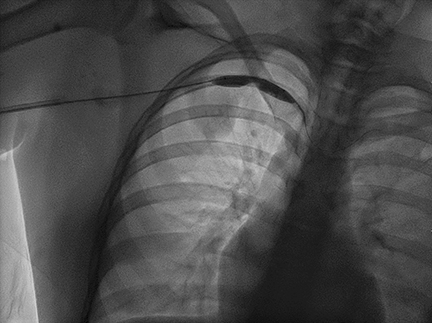
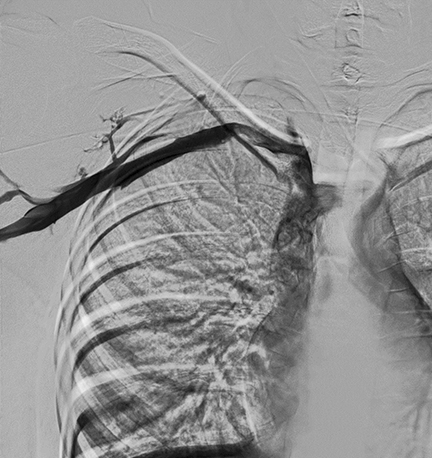
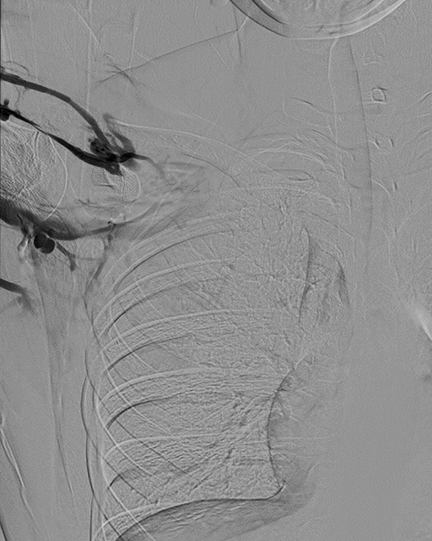
Right upper-extremity digital subtraction venography (DSV) showed a completely occlusive deep venous thrombosis (DVT) of the entire right subclavian vein and a non-occlusive thrombus within the right axillary vein. There was marked narrowing at the overlap of the clavicle and first rib, improved after angioplasty to 8 mm (Figure 1). Following angioplasty, residual DVT was treated with mechanical thrombolysis. A follow-up dynamic venogram was performed with the right upper extremity in adduction, 90-degree abduction, and 180-degree abduction. On adduction, mild, elongated narrowing of the right axillary vein without occlusion of the right subclavian vein was observed (Figure 2).
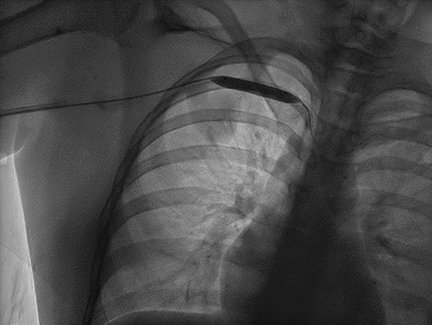
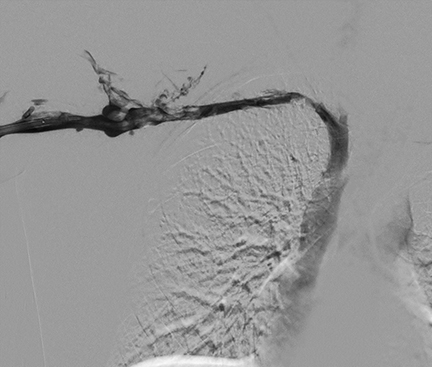
Ninety-degree abduction showed mild narrowing of the right subclavian vein immediately medial to the right first rib/clavicular overlap, as evidenced by concavity of the inferior wall of the subclavian vein (Figure 3). There was resolution of the right-axillary-vein elongated narrowing but delayed contrast outflow from the right axillary vein. Abduction of 180 degrees showed complete occlusion of the right subclavian vein, with no opacification of collateral veins in the proximal right upper extremity and around the shoulder (Figure 4). Once the arm was returned to adduction, contrast transit resumed from the right upper extremity through the subclavian vein.
Diagnosis
Paget-Schroetter Syndrome (PSS)
The clinical differential diagnosis includes rotator cuff tear, shoulder impingement syndrome, Pancoast syndrome, cervical/thoracic disc disorders (radiculopathy, discogenic pain syndrome), brachial plexus injury, and fibromyalgia.
Discussion
Thoracic outlet syndrome (TOS) is an umbrella term for conditions that involve compression of neurovascular structures as they pass from the lower neck to the axilla (the thoracic outlet). These neurovascular structures, which include the brachial plexus and subclavian artery and vein, pass between the clavicle and first rib, a space termed the thoracic outlet. Thrombosis involving the axillary-subclavian vein is termed Paget-Schroetter syndrome, a subtype of TOS. In general, TOS is caused by compression secondary to four main causes, which may be interrelated.1
Congenital abnormalities are common causes; examples include bony anomalies such as the presence of a cervical rib, an elongated transverse process of the first thoracic rib or fibromuscular anomalies.
Post-traumatic causes include soft- tissue injury to the neck, shoulder, or upper limb. In particular, “whiplash” injuries can compress neurovascular structures passing through the scalene muscles. Functional or acquired causes are often reported in athletes, especially those participating in sports with overhand motions, such as volleyball, baseball, and weightlifting. These sports can cause dysfunction, inflammation, or hypertrophy of muscles in the cervicoscapular regions, leading to vascular compression or injury to vein walls. Lastly, acquired causes must be considered. While rare, these can include neoplasms involving the axilla or lung apex such as Pancoast tumors, hyperostosis, and osteomyelitis of the collarbone and/or first rib.
The subtypes of TOS are categorized according to which neurovascular structure is compressed. Neurogenic TOS is the most common and involves brachial plexus compression, leading to paresthesias of the hand and neck.2 Typically, the inferior trunk and roots of the brachial plexus are compressed, which may cause symptoms similar to a Klumpke palsy. However, compression of other brachial plexus trunks is not uncommon. Furthermore, Horner syndrome may be seen if the T1 vertebral roots are affected, disrupting the hypothalamospinal tract and, thus, sympathetic input to the face.
Arterial TOS is characterized by compression of the subclavian artery, which leads to intimal damage, turbulent blood flow, vessel dilation and occasionally thrombosis.3 This presents clinically as pulselessness, pain, pallor, paresthesia, and coldness of the affected arm. Left untreated, arterial TOS can lead to ulceration and gangrene of the digits. Venous TOS, caused by compression of the subclavian vein, leads to abrupt blood flow stagnation and subsequent effort thrombosis.3 This presents clinically as an acute upper extremity swelling, cyanosis, and pain. Raynaud-like symptoms may be appreciated with venous TOS, but they will be unilateral in nature. Further, venous TOS will increase the likelihood of an upper-extremity DVT, otherwise known as Paget-Schroetter syndrome.4
Diagnosis of PSS is straightforward. Ultrasonography or venography is indicated if the clinical presentation suggests an upper-extremity DVT. A plasma D-dimer is useful in excluding thrombosis but will not rule out an underlying venous stenosis without thrombosis as the underlying cause. While duplex sonography of the upper extremity may be diagnostic, venography can offer both diagnostic and therapeutic utility.5 Contrast injection via the brachial vein at the antecubital fossa or via other upper-arm veins may demonstrate a missed diagnosis.6
After thrombolysis, venography can be repeated in adduction, 90-degree abduction, and 180-degree abduction of the right upper extremity to observe for compression at the costoclavicular junction. In our patient, mild narrowing of the right subclavian vein was observed just medial to the lateral first right rib on 90-degree abduction (Figure 3), while complete occlusion was seen with 180-degree abduction (Figure 4). Performing these follow-up studies can guide treatment to reduce the risk for long-term sequelae of PSS.
Patients presenting with a confirmed upper-extremity DVT, as seen in PSS, should be treated with mechanical thrombectomy and/or thrombolysis. The aim of this therapy is a prompt dissolution of the thrombus, minimizing endothelial cell injury and re-establishing venous flow. Subsequently, patients should be placed on anticoagulation for a minimum of three months, as established by guidelines of the American College of Chest Physicians.7,8
There is little role for stenting in PSS, as studies have shown stenting of a non-decompressed costoclavicular junction is complicated by stent fracture, deformation, and re-thrombosis rates as high as 40%.9 While a small subset of patients may remain asymptomatic without sequelae after anticoagulation, decompressive surgery is typically necessary. The goal of this surgery is to provide more space for neurovascular structures of the upper arm to pass through unimpeded. Thoracic outlet decompression should be tailored based on the specific anatomic abnormality.
The approach may include, but is not limited to, a first-rib resection, cervical-rib resection, anomalous band division, and scalenectomy.10,11 However, in the absence of an anatomic anomaly, a first-rib resection may be preferentially performed. In our case, a right first-rib resection, division of the right anterior scalene, and neuroplasty of the right brachial nerve were performed. Postsurgical imaging should be used to confirm patency of the subclavian vein.
Conclusion
Thoracic outlet syndrome is a diagnostic category representing a spectrum of conditions characterized by compression of neurovascular structures as they pass through the thoracic outlet. Paget-Shroetter syndrome is a subtype of TOS characterized by effort thrombosis of the axillary-subclavian vein. The clinical presentation typically consists of acute upper-extremity swelling, cyanosis, and pain. PSS can be diagnosed with duplex sonography, although venography is more diagnostically sensitive and provides an opportunity for minimally invasive, therapeutic procedures.
Venography with upper-extremity adduction and abduction can provide diagnostic information on the etiology and degree of venous compression. Initial treatment should consist of mechanical thrombectomy and/or thrombolysis and subsequent anticoagulation for at least three months. If symptoms persist, thoracic outlet decompression is recommended, which should be tailored to the specific anatomic anomaly. In the absence of an anatomic anomaly and confirmed compression by the costoclavicular junction on the subclavian vein, a first-rib resection may be performed. Patients should be followed postoperatively to evaluate patency of the subclavian vein and to ensure resolution of symptoms.
References
- Laulan J, Fouquet B, Rodaix C, Jauffret P, Roquelaure Y, Descatha A. Thoracic outlet syndrome: definition, aetiological factors, diagnosis, management and occupational impact. J Occup Rehabil. 2011;21(3):366-373. doi:10.1007/s10926-010-9278-9.
- Freischlag J, Orion K. Understanding thoracic outlet syndrome. Scientifica. 2014;2014:248163. doi:10.1155/2014/248163.
- Jones MR, Prabhakar A, Viswanath O, et al. Thoracic outlet syndrome: A comprehensive review of pathophysiology, diagnosis, and treatment. Pain Ther. 2019;8(1):5-18. doi:10.1007/s40122-019-0124-2.
- Sharma H, Tiwari A. Recurrent upper extremity thrombosis associated with overactivity: a case of delayed diagnosis of Paget-Shroetter syndrome. Case Rep Vasc Med. 2017;2017. doi:10.1155/2017/8764903.
- Illig KA, Doyle AJ. A comprehensive review of Paget-Schroetter syndrome. J Vasc Surg. 2010;51(6):1538-1547. doi:10.1016/j.jvs.2009.12.022.
- Green R.M,, Rosen R. Handbook of Venous Disorders: Guidelines of the American Venous Forum Third Edition. CRC Press; 2008.
- Kearon C, Akl EA, Ornelas J, et al. Antithrombotic therapy for VTE disease: CHEST Guideline and Expert Panel Report. Chest. 2016;149(2):315-352. doi:10.1016/j.chest.2015.11.026.
- Kearon C, Akl EA, Comerota AJ, et al. Antithrombotic therapy for VTE disease: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e419S-e496S. doi:10.1378/chest.11-2301.
- Meier GH, Pollak JS, Rosenblatt M, Dickey KW, Gusberg RJ. Initial experience with venous stents in exertional axillary-subclavian vein thrombosis. J Vasc Surg. 1996;24(6):974-983. doi:10.1016/S0741-5214(96)70043-5.
- Urschel HC, Razzuk MA. Paget-Schroetter syndrome: what is the best management? Ann Thorac Surg. 2000;69(6):1663-1668; discussion 1668-1669. doi:10.1016/s0003-4975(00)01151-6.
- Chang KZ, Likes K, Demos J, Black JH, Freischlag JA. Routine venography following transaxillary first rib resection and scalenectomy (FRRS) for chronic subclavian vein thrombosis ensures excellent outcomes and vein patency. Vasc Endovascular Surg. 2012;46(1):15-20. doi:10.1177/1538574411423982.
References
Citation
JH J, RB T, AJ T, CM S, DJ A.Paget-Schroetter Syndrome. Appl Radiol. 2021; (4):56E-56H.
July 14, 2021